
Clinical features of 64 patients (outside Hubei) with COVID-19 in Wenzhou, China
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1). Given its rapid spread worldwide, the epidemiological and clinical features of COVID-19 mandate further clarification. According to previous Wuhan-based studies, which respectively included 41 (2), 99 (3) and 52 (4) laboratory-confirmed COVID-19 patients, SARS-CoV-2 mimicked severe acute respiratory syndrome coronavirus in terms of severity and high mortality, however, a subsequent study conducted on 13-cases in Beijing demonstrated that all patients were mildly infected (5). Results of these studies varied greatly and were contradictory, therefore, we collected the data from 64 patients admitted to Oujiangkou Branch, the Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, aiming to describe the epidemiological and clinical characteristics of COVID-19 patients in Wenzhou city which, although far away from Hubei Province, is the most-affected area in China outside Hubei.
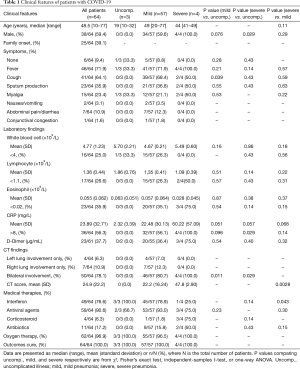
For this retrospective study, 64 laboratory-confirmed COVID-19 patients, admitted from Feb 6, to Feb 11, 2020 in above mentioned hospital were recruited. Confirmation of SARS-CoV-2 was done by real-time RT-PCR assay of sputum, throat-swab specimen. Patients were categorized into 3 groups, uncomplicated illness, mild-pneumonia and sever-pneumonia respectively, according to the severity defined by World Health Organization interim guidance (6). Epidemiological, demographic, clinical, laboratory and radiological data were extracted from medical records of patients. CT score was obtained by synthesizing the grading of range and density of the exudative lesion, following protocol from a previous study (7). Present study was approved by the Ethics Committee of above-mentioned Hospitals of Wenzhou Medical University (L-2020-13), along with a waiver of informed consent.
Of all the 64 cases, 38 (59.4%) were male. Median age was 48.5 years (range, 10–77). Fever (71.9%) and cough (64.1%) were the most common symptoms, whereas nausea/vomiting (3.1%), abdominal pain/diarrhea (10.9%), and conjunctival congestion (1.6%) were rare (Table 1). A 5th-generation case was found in the study (Figure 1A). Patient 1 (Generation 2), who had never contacted with wildlife or Huanan Seafood Market, transmitted the SARS-CoV-2 to Patient 2 (Generation 3) during his visit. The latter transmitted the virus to his family members (Patient 3 & 4, Generation 4). Finally, the virus reached to hairstylist (Patient 5, Generation 5) when he repeatedly contacted with one of the family members and got laboratory-confirmed for COVID-19 on the following day.
Full table

Twenty-five (39.1%) cases were involved in SARS-CoV-2 infected family clusters (Table 1), among them was a 9-member cluster from a 12-member family, which originated from a local epidemic area (Intime-Mall). Index patient worked at a local epidemic Mall. She spread the virus to 8 other members of the family when she traveled to her hometown in another District with her husband and son (Figure 1B). Presence of a considerable number of family clusters strengthened.
Lymphopenia was observed in 15 (26.3%) patients with mild-pneumonia and 2 (50.0%) patients with severe-pneumonia. Eosinophils reduction was also documented in 20 (35.1%) patients of the mild-pneumonia group and 3 (75.0%) of severe-pneumonia group. CRP rose in 32 (56.1%) patients of mild-pneumonia group and 4 (100%) of severe-pneumonia group, but in none of the uncomplicated-illness group (Table 1, Figure 1C). Neutrophil to lymphocytes ratio (NLR) of severe-pneumonia group was significantly higher than that of mild-pneumonia group (P=0.0406) (Figure 1D). Level of D-Dimer rose in 20 (36.4%) of 55 patients of mild-pneumonia group and 3 (75%) of 4 patients of severe-pneumonia group while normal levels of alanine aminotransferase, PCT, bilirubin, serum creatinine were documented only in a small number of patients (data not shown). CT findings showed that 50 (78.1%) patients manifested bilateral involvement. Average CT score was 24.9±22.2. Compared to that of mild-pneumonia group (22.2±16.24), CT score of the severe-pneumonia group (47.8±2.9) was markedly higher (P=0.0028) (Table 1, Figure 1E). All 64 patients in our study were cured and discharged till March 10, 2020, although 3 of them were transferred to Intensive Care Unit once during treatment. In this study, the cure rate was 100% and the mortality was 0 (Table 1).
For treatment, oxygen therapy, antiviral therapy, interferon inhalation, intravenous antibiotics and glucocorticoid therapy were selectively initiated in different patients (Table 1).
Before the official announcement of Wuhan lockdown, around 20,000 Wenzhou businessmen traveled back to Wenzhou for the spring festival, thus making it the most seriously hit city outside Hubei, where then strictest quarantine strategy was implemented. Interestingly, we found that the severity and mortality in Wenzhou-cases were much milder than those in Hubei-cases. A significantly lower fatality rate was found in Wenzhou (outside Hubei), compared to previous Wuhan-based studies where it was 15% (2) and 4.3% (8). Moreover, we discovered that rate of severity and complications related to COVID-19 was very low in Wenzhou, as compared to those in Wuhan. The low mortality in Zhejiang Province (9) suggests the prominent role of quarantine policies and emphasizes their strict implementation as the global epidemic continues to worsen (10).
Family clusters accounted for 39.1% of all cases in our study, strengthening the idea of efficient human-to-human transmission. Consistently, strong longitudinal infectivity was further proved by our discovery of a 5th-generation COVID-19 case. Our study also revealed the presence of asymptomatic cases (9.4%), which might be a potential source of infection. Aiming to extend the diagnostic parameters, we looked for new markers to predict the severity of COVID-19 and discovered that NLR and CT score were significantly elevated in severe-pneumonia group.
Presence of a considerable number of asymptomatic patients in our study cohort draws attention towards more strict screening and contact tracing of infected individuals, because of the likelihood that presence of asymptomatic patients might lead to misdiagnosis of the potential infected source and contribute to the rapid spread of the virus. Specifically involving Wenzhou-patients, the study is limited by the small sample size of severe-pneumonia group. Finally, considering the recruitment of Wenzhou-based patients only, our study depicts a true picture of the clinical condition and characteristics of patients outside Hubei.
Acknowledgments
We acknowledge all the patients involved in our study and all the health-care workers involved in treatment and diagnosis of patients in Wenzhou.
Funding: This study was supported by National Natural Science Foundation of China (grant numbers 81800028, 81570027).
Footnote
Provenance and Peer Review: This article was a free submission to the journal. The article was sent for external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-1861). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work (including full data access, integrity of the data and the accuracy of the data analysis) in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen L, Liu W, Zhang Q, et al. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg Microbes Infect 2020;9:313-9. [Crossref] [PubMed]
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [Crossref] [PubMed]
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507-13. [Crossref] [PubMed]
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8:475-81. [Crossref] [PubMed]
- Chang D, Lin M, Wei L, et al. Epidemiologic and Clinical Characteristics of Novel Coronavirus Infections Involving 13 Patients Outside Wuhan, China. JAMA 2020;323:1092-3. [Crossref] [PubMed]
- WHO. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected. 2020. Available online: https://apps.who.int/iris/handle/10665/331446?search-result=true&query=10665%2F331446&scope=&rpp=10&sort_by=score&order=desc
- Xie H, Huang X, Zhong X, et al. Pneumocystis jiroveci pneumonia in AIDS: the correlation between SLDH and CT quantitive score of exudative lesion. Electron J Emerg Infect Dis 2018;3:15-20.
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020;323:1061-9. [Crossref] [PubMed]
- Xu X, Wu X, Jiang X, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ 2020;368:m792. [Crossref] [PubMed]
- Aggarwal S, Garcia-Telles N, Aggarwal G, et al. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): Early report from the United States. Diagnosis (Berl) 2020;7:91-6. [Crossref] [PubMed]


