Theoretical models of carcinogenic particle deposition and clearance
in children’s lungs
Brunnleitenweg 41, A-5061 Elsbethen, Salzburg, Austria
|
Original Article
Theoretical models of carcinogenic particle deposition and clearance
in children’s lungs
Brunnleitenweg 41, A-5061 Elsbethen, Salzburg, Austria
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract
Introduction: Deposition and clearance of carcinogenic particles in the lungs of subjects belonging to four different age groups (infants, children, adolescents, and adults) were theoretically investigated. The study is thought to contribute to the improvement of our knowledge concerning the behaviour of inhaled particles in lungs that may be attributed to different stages of development. Methods: Particle deposition and clearance were simulated by using a well established stochastic lung model, allowing the generation of nearly realistic scenarios. For the computation of particle deposition all main deposition forces were considered. Additionally, any influences on particle behaviour due to particle geometry were covered by using the aerodynamic diameter concept. Particle clearance was simulated by defining both a fast mucociliary clearance phase and a slow bronchial/alveolar clearance phase, the latter of which is based on previously published models and suggestions. Results: As clearly provided by the modelling computations, lung deposition of particles with aerodynamic diameters ranging from 1 nm to 10 μm may significantly differ between the studied age groups. Whilst in infants and children most particles are accumulated in the extrathoracic region and in the upper bronchi, in adolescents and adults high percentages of inhaled particular substances may also reach the lower bronchi and alveoli. Although mucus velocities are significantly lower in young subjects compared to the older ones, fast clearance is more efficient in small lungs due to the shorter clearance paths that have to be passed. Slow clearance is commonly characterized by insignificant discrepancies between the age groups. Conclusions: From the study presented here it may be concluded that particle behaviour in infants’ and children’s lungs has to be regarded in a different light with respect to that in adolescents and adults. Although young subjects possess natural mechanisms of protecting their lungs from hazardous aerosols (e.g., expressed by breathing behaviour and lung size), they are much more sensitive to any particle exposure, since particle concentrations per lung tissue area may reach alarming values within a short period of inhalation. Key words
Stochastic lung model; random walk; deposition force; mucociliary clearance; slow clearance
J Thorac Dis 2012;4(4):368-376. DOI: 10.3978/j.issn.2072-1439.2012.08.03 | |||||||||||||||||||||||||||||||||||||||||||||||||
|
Introduction
Based on numerous epidemiological studies (1-3), it may be
regarded as a largely accepted fact that several kinds of airborne
particles act as serious health hazards when they are taken up
into the respiratory tract. During the past 40 years most scientific
investigations dealing with health effects of inhaled particles
primarily included adults exposed to certain aerosols in their
working environments (e.g., workers in mines or cotton mills).
Additionally, biological effects of either naturally or artificially
occurring radioactive aerosols on adult males and females were
subjected to an extensive physical and medical analysis (1).
Although the number of scientific articles and books on these
topics has been increased exponentially during the past decades,
detailed studies on the inhalation of different aerosol particles
by children and the consequences of this respiratory uptake for
the child’s lung have been conducted for about 20 years (4,5).
Meanwhile, it is a well-known fundamental in paediatric science
that children especially living in urban environments may be
exposed to higher aerosol doses (e.g., CO, CO2, diverse dusts raised by enhanced traffic, soot) (3). In rural environments
children may be for instance confronted with increased amounts
of biogenic aerosols, from which some types have been identified
as triggers of infectious or allergic diseases (6,7).
Concerning the carcinogenicity of airborne particles, especially
four categories of aerosols have to be mentioned in conjunction with
children (Figure 1): the first category includes all kinds of dusts,
i.e., particles originating from diverse mechanical manufacturing
processes. Due to their geometric shape highly deviating from an
ideal sphere, this particular matter is characterized by a peculiarity
regarding both its deposition and its clearance in the respiratory
tract (8). Bioaerosols, belonging to the second category, may also
contain carcinogenic particle types (e.g., plant fibers), whereby the
interactions between biogenic particles and different lung tissues are
not fully decoded hitherto (9). The third category of carcinogens
with enhanced relevance for children includes various kinds
of smokes and, even more important, soot resulting from
combustion processes (8-11). As demonstrated by histological
studies, soot particles not soluble by any metabolic processes have
the ability to intrude into lung cells, where they may unfold their
unwholesome efficacy after years of intracellular accumulation
and storage (12). Ultrafine particles have been attributed to an individual category, although they include participants from the
other categories mentioned above. Carcinogenicity of ultrafines
mainly arises, if these particles are increasingly accumulated
in respiratory compartments or adjacent structures (e.g., the
lymphatic system) (1).
Figure 1. Sketch illustrating those aerosol particle categories which are
commonly known to have a hazardous effect on children. Besides the particles
acting as triggers for infections and allergic reactions, some of these particular
substances are also discussed to possess carcinogenic properties.
Deposition experiments conducted with children of different
age and gender clearly showed that tidal volume positively
correlates with age, whilst breathing frequency is subject to a
continuous decrease from younger to older subjects (13,14).
As a result of this physiological development, deposition
fractions among children as well as between children and adults
may be characterized by significant differences (4,10,11,15).
Despite these preliminary results lots of questions regarding the
deposition behaviour of inhaled particles in children’s lungs have
to be studied more in detail in order to be brought to a largely
accepted solution.
Data regarding the clearance of particles from children’s
lungs are only available in scarce amounts hitherto (5). It is
assumed that tracheal mucus transport and, as a consequence of
that, also mucociliary clearance in the bronchi and bronchioles
is permanently accelerated with increasing age, reaching its
maximum at an age between 18 and 25 years (16,17). Theoretical
models based on this assumption suggest slightly smaller
clearance efficiency in children with respect to adults which is
compensated or even over-compensated by significantly shorter
clearance paths that have to be mastered in the respiratory
systems of infants and adolescents (18). Due to the lack of any
information, slow clearance (bronchial and alveolar) is equally
handled in children and adults so far. However, questions arising
in conjunction with particle clearance in children are of much
higher complexity than any deposition problems noted above.
The purpose of the present study was to extend our
knowledge on both particle deposition and particle clearance in
the lungs of infants (1 year), children (5 years), and adolescents
(15 years). In order to come to satisfactory results, a theoretical
model that has been continuously extended and improved over
the past ten years was applied. This mathematical approach
is based on stochastic descriptions of lung architecture and
particle transport and additionally enables the variation of a high
number of morphometric and physiological parameters. Based
on the modelling computations it is hypothesized that particle
behaviour may be indeed categorized according to the age of the
studied subjects.
| |||||||||||||||||||||||||||||||||||||||||||||||||
|
Methods
Model of the child’s lung morphometry
Simulation of lung morphometry was commonly conducted
by application of the stochastic model originally defined by
Koblinger and Hofmann (19). Within this theoretical approach morphometric data obtained from interferometric measurements
of the tracheobronchial tree (20) and the acinar compartment
of the human lung (21) were subjected to extensive statistical
evaluations. This, among other, resulted in the definition of
reliable generation-specific probability density functions for
the distributions of airway diameters, airway lengths, branching
angles, and gravity angles (i.e., the angles of single airway tubes
relative to the direction of gravity). For the generation of a
nearly-realistic lung architecture airway parameters were selected
from the related probability density functions with the help of
a pseudo-random number generator. During this step of the
mathematical process also potential correlations between the
morphometric parameters themselves were considered. The
procedure ended in the construction of random airway paths
and the junction of a pre-selected number of these paths (e.g.,
10,000) to the stochastic lung.
In the original model, stochastic lung size was calibrated to a
functional residual capacity (FRC) of 3,300 mL which represents
the mean value for a male Caucasian adult (1). In order to model
children’s lung morphometry in an appropriate way, respective
dimensions of the tracheobronchial tree were re-calibrated by
the application of scaling factors. As found by Phalen et al. (22),
the dimensions of the trachea and bronchi may be related to
body height according to the simple mathematical equation
 In equation [1] the scaling factor, SF, denotes the ratio of airway
diameter or length in the subject compared to that in reference
man, whilst HS is the height of the subject in meters and a an
airway-generation-specific constant [1]. Alternatively, scaling
factors for the diameters and lengths of the tracheobronchial
airways were calculated according to the expression
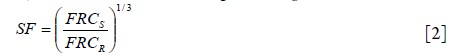 where FRCS denotes the functional residual capacity of the
subject of interest and FRCR represents the functional residual
capacity of a reference subject [1]. Respective values for airway
calibration derived from equation [2] are summarized together
with age-specific physiological parameters necessary for
modelling computations in Table 1.
Modelling the deposition of particles in the child’s lung
Computation of particle deposition in individual airways due
to various deposition forces was carried out by application of
analytical deposition equations that are only valid for straight
cylindrical tubes and spherical spaces. Generally, four deposition
mechanisms, namely Brownian motion, inertial impaction,
interception, and gravitational settling, were distinguished.
Particle deposition forced by Brownian motion was computed
using the related empirical equation outlined by Cohen and
Asgharian (23). This approximation considers an increase in
deposition in the upper bronchial airways due to developing
flow. Particle deposition in more peripheral airway tubes was
enabled with the help of the diffusion equation proposed by
Ingham (24). Deposition of particles in the upper airways due
to inertial impaction and interception was chiefly approximated
by the application of correction factors (25) that are added to
the respective standard equations. Extrathoracic deposition
efficiencies, expressing the ability of nasal and oral airways to
filter inspired particular material, were estimated on the basis of
empirical equations derived either from in vivo measurements or
from collected experimental data.
Analytical and empirical equations for the prediction of
particle deposition in the human respiratory tract are founded
upon the hypothesis that all particles inhaled from the ambient
atmosphere have ideal spherical shapes. However, this ideal
geometry is limited to a low number of aerosol categories
that may be found in nature or emanate from anthropogenic
processes. Most particle types, above all those representing
a serious health hazard for children, are characterized by
nonspherical (e.g., fibrous or disk-like) shapes (see above). In
some cases, aerosol particles also occur as irregularly shaped
aggregates that consist of a high number of randomly arranged
spherical or nonspherical components (26).
The problem of irregular particle shapes is most successfully
approximated by the aerodynamic diameter concept (mobility
diameter for ultrafine particles). This parameter, named dae, corresponds to the diameter of a unit-density sphere with
identical aerodynamic characteristics as the nonspherical particle
of interest. Mathematically, dae is commonly expressed by the
formula (27-30)
 where dve represents the volume-equivalent diameter (i.e.,
the diameter of a sphere with exactly the same volume as the
investigated particle) and χ the dynamic shape factor, whilst
ρp and ρ0 denote the density (g.cm-3) of the particle and unitdensity
(1 g.cm-3). The remaining variables Cdve and Cdae are
the so-called Cunningham slip correction factors for spheres
with diameters dev and dae, respectively. For oblate (i.e., disklike)
or prolate (i.e., fibrous) geometry the dynamic shape
factor χ generally adopts values greater than 1 and, in the case of
particles with highly irregular geometries, also values around 15
(26,30). The Cunningham correction factors may be neglected
for particles that are transported in the continuum regime
(i.e., particles with diameters greater than 1 μm), because they
uniformly take values around 1. In the slip-flow regime, which
represents the dominant aerodynamic environment for particles
smaller than 1 μm and especially for ultrafine particles (<100 nm),
the factors become significant determinants with regards to the
calculation of dae, thereby following an exponential increase with
decreasing particle size.
Modelling the clearance of deposited mass from the child’s
respiratory tract
The stochastic clearance model includes several assumptions and
experimental findings that have been published during the last
years (31,32). As particle deposition is considered to take place
in the first half of a respective airway due to diffusion, inertial
impaction, interception or sedimentation, clearance always starts
from the midpoint of the initial bifurcation within the computed
path. The calculation of the mucus velocity within a specific
airway of the clearance path is made possible by including the
airway geometry. Concerning a single bifurcation, the first step
in this algorithm is the determination of a velocity factor that
is derived from the respective cross-section function, i.e., the
quotient of cross sections between the daughter airway (Ai)
and the related parental airway (Ai-1). The mucus velocity in a
daughter airway, vi, is then simply available by multiplying the
related velocity of the parent tube, vi-1, with this factor:
 According to this concept, all velocities needed for a
simulation are calculated from the initial tracheal mucus velocity.
Changes of this initial velocity or the lung morphometry
can significantly influence clearance rates within the whole
tracheobronchial tree.
As found by instillation of labelled material in the upper
bronchial airways of rats, mucus transport is affected by a certain
delay at the carinal ridges of single bifurcations. At these sites,
mucus flow is splitted on the one hand and accumulated for
some time on the other hand. In the rat lung, the half-life of
clearance from the carinal ridges is about 1 hour, while similar
information for the human lung is not available at the moment.
In the stochastic clearance model, this phenomenon can be
considered optionally by defining a mucus delay time, td, which is
uniformly applied to all bifurcations of the tracheobronchial tree.
As a simplification, all mucus is affected by this delay, but not
only the mucus at the carinal ridges (about 10 %), so that delay
time has to be diminished remarkably (about 10 minutes). Total
residence time, tr,i, of a deposited particle in airway i with length
Li is given by the formula:
 As outlined in previous contributions (27,31,32),
tracheobronchial clearance can include a significant fraction
fs of slowly cleared particles due to their uptake into the
epithelium, accumulation in the sol phase or phagocytosis by
airway macrophages. As already found by shallow aerosol bolus
experiments, fs strongly depends on the size of inhaled particles.
In the clearance model of this study, the slow clearance fraction
is simply calculated from the following linear equation:
 where dg denotes the respective geometric particle diameter in
μm. Final residence time of particulate matter with given size is
derived from equation [5] as follows:
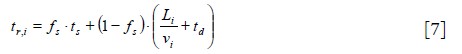 with ts denoting the average half-time of the slow clearance
process (5-20 days). In order to consider the contribution
of alveolar clearance, the model is additionally extended by
respective alveolar clearance half-times (1) being on the order of
several hundreds of days.
| |||||||||||||||||||||||||||||||||||||||||||||||||
|
Results
Theoretical lung morphometry of children and adults
Independent of the age of the investigated subject, airway
diameter is related to airway length by a logarithmic function
(Figure 2). Whilst in lung generation 1, representing the trachea,
airway length exceeds the respective airway diameter by a factor
of 5, in the terminal lung generations lengths and diameters of
single airway tubes may be on the same order of magnitude. The
development of such short tubular segments of the respiratory
tract results in partly significant consequences for particle
deposition and clearance (see below).
Figure 2. Graphs exhibiting the mathematical relationship between airway length and airway diameter for lung generations 1 to 16 (mean
values ± standard deviations). Due to the constant scaling factor, being equally applied to each airway generation, the diameter-length
correlations are nearly identical in infants (A), children (B) and adolescents (C), and adults (D).
Due to the scaling procedure introduced in the preceding
section, airway geometry of infants is reduced in size by a factor of
3 with respect to that of adults, whereas tubular morphometry of
children being at the age of 5 years exhibits almost half the size of
an adult lung structure. In adolescents with an age of 15 years lung
geometry is nearly fully developed, so that discrepancies compared
to adult lungs may be regarded as insignificant (Figure 2).
Particle deposition in children’s and adults’ lungs
As illustrated in the graphs of Figure 3, deposition of particular
matter in the human respiratory tract commonly depends on the
size of inhaled particles expressed by the aerodynamic diameter
(see above). Independent of the subject’s age, total and regional
(i.e., tubular and alveolar) lung deposition may be regarded as
functions of aerodynamic diameter insofar as small particles
(<100 nm) as well as large particles (>1 μm) show a somewhat
different deposition behaviour with respect to intermediately
sized particles (100 nm -1 μm). In the case of total deposition
this circumstance results in the development of U-shaped or
V-shaped functions. Concerning tubular deposition, representing
the accumulation of inhaled particular matter in all kinds of
bronchial structures, deposition maxima are slightly displaced
towards intermediate aerodynamic diameters (Figure 3),
whereas smallest (1 nm) and largest particles (10 μm) are again
characterized by a more or less dramatic decline of deposition.
In the case of 10-μm particles deposition is significantly decreased
with respect to 3-μm particles. Alveolar deposition is marked
by similar trends as tubular particle accumulation, whereby
deposition maxima are further displaced towards intermediate
aerodynamic diameters and generally range from 2% to 20 % of the
whole particular mass inhaled during a breathing cycle (Figure 3).
As underlined by the respective graphs of Figure 3, both particles
of molecular size and largest particles being subject to inhalation
are practically not deposited in the alveolar structures, lowering
their significance in the case of microdosimetric considerations.
Figure 3. Total, tubular (i.e., bronchial and bronchiolar), and alveolar deposition of particles and their dependence on the aerodynamic particle diameter: (A) infants (1 y), (B) children (5 y), (C) adolescents (15 y), and (D) adults.
Whilst deposition patterns of variably sized particles are
characterized by partly notable similarities among the subjects’
age classes, there may be recognized partly significant differences
regarding the amount of particular mass accumulated in the
tubular and alveolar compartment (Figure 3). In general, total
deposition is positively correlated with age, with respective
values for adult lungs exceeding those for infants by a factor
of 1.5-3 and those of children by a factor of 1.3-2.5. Total deposition functions change from broad U-shape in infants to
nearly V-shape in adults. Lower values of total deposition in
infants’ and children’s lungs have consequences with regards to
regional deposition: whilst tubular accumulation of particular
matter amounts to about 20% (infants) and 50% (children) with
respect to that in adolescents and adults, alveolar deposition
commonly reaches values of 10% (infants) and 40% (children)
compared to that in adolescents and adults.
Particle clearance from lungs of subjects with different age
For a comprehensible presentation of clearance efficiency in
subjects of different age, 24-h as well as 5-d and 10-d retention
values and their dependences on aerodynamic diameter have been
drawn for infants, children, adolescents, and adults (Figure 4).
Whilst 24-h retention enables an appropriate differentiation
between fast mucociliary and slow transepithelial/macrophage
clearance, 5-d and 10-d retention values provide an insight into
the course of slow clearance and the fraction of particles directly
cleared from the alveoli. According to the clearance model
introduced in the preceding section removal of particles on the
mucociliary escalator commonly takes place for those particles
that are mainly deposited in the proximal tubular compartment
of the lung, whereas slow clearance mechanisms are chiefly
concentrated in the lower tubular and alveolar compartment.
Independent of the age group fraction of slowly cleared particles
is highest for aerodynamic diameters ranging from 0.01 to 1 μm.
Contrary to that, particles with aerodynamic diameters of <0.01 μm
and >1 μm are almost completely evacuated from the lung within
shorter periods of time. Thereby, highest clearance efficiency
may be attested for infants, where all particular mass is removed
after 24 h. In the remaining age groups complete removal of very
small and large particles takes place within several days (Figure 4).
Slow bronchial and alveolar clearance of intermediately sized
particles may be evaluated as nearly constant among the age
groups.
| |||||||||||||||||||||||||||||||||||||||||||||||||
|
Discussion
Deposition and clearance of inhaled particular matter depend
on a high number of factors, among which lung morphometry
plays a superior role. As already proven by numerous inhalation
experiments, the probability of particles being deposited in
the respiratory tract increases with the length of the path,
upon which these particles are transported (33-35). A
counterpart to the airway path length is commonly given by
the medium airway caliber [sensu Horsefield et al. (36)] that
exhibits a negative correlation with deposition probability. Since both morphometric factors do not compensate each
other, discrepancies in particle deposition may be already
observed between lungs of nearly identical size (note: breathing
parameters are assumed to be constant) and principally between
lungs of adult males and females belonging to the same age
group. Highest relevance of this phenomenon may be observed
by the comparison of infants, children, and adolescents, whereby
gender-specific differences remain insignificant (1).
As underlined by the theoretical results exhibited in Figure 3, particle deposition is partly characterized by significant
differences among the investigated age groups, with highest
deposition fractions being commonly recognizable for
adolescents (15 y) and adults and lowest deposition fractions
being computed for infants (1 y). A physical reason for this
phenomenon may be found in the complex interaction between
deposition mechanisms and breathing parameters which both
depend upon lung morphometry (1,22). Low tidal volumes
measured in infants (Table 1) cause a rather shallow breathing
with the important consequence that residence times of
inhaled particles are set to a minimum. The contrary case may
be observed for the lungs of adolescents (high tidal volumes
and higher particle residence times). On the other hand, lung
architecture of infants increases the efficiency of single deposition
forces (Brownian motion, inertial impaction, interception and
gravitational settling) which all depend on airway diameter
and, slightly less important, airway length (1,18,27). Brownian
motion results in an enhanced deposition of ultrafine particles
in the upper bronchi, whilst inertial impaction, interception and
gravitational settling mainly affect larger particles (>1 μm) to be
accumulated in the proximal and distal lung. In adolescents and
adults the increased efficiency of deposition forces due to lung
morphometry is much less significant (Table 1) (1).
Regarding particle clearance, phenomena similar to those
explaining particle deposition may be recognized; on the one
side, lengths of clearance paths are strongly reduced in infants
with respect to children, adolescents, and, most of all, adults.
This circumstance is most effectively expressed by the so-called
scaling factor (Table 1) that may be applied to both airway
diameter and airway length, and whose determination is largely
founded upon comprehensive morphometric investigations
(1,20-22). On the other side, mucus transport times, reflecting
the velocity of the so-called mucociliary escalator (26,27,32),
represent a function of age (16,17), thereby continuously
increasing from zero to 25 years and being subject to a decrease
from 26 to 60 years. Basically, the age dependence of mucociliary
clearance is found by a simple mathematical approximation: the scaling factor is compared with the quotient of the tracheal
mucus velocity of the age group of interest and the tracheal
mucus velocity of 5.5 mm∙s-1 (mean value for adults). If the first
quotient is lower than the second one, lung morphometry has
to be regarded as main determinant of mucociliary clearance;
if, on the other side, the first quotient is higher than the second
one, mucus transport velocities represent the main determinant
of fast clearance. In the theoretical case presented here, the
influence of morphometry slightly exceeds the influence of
transport velocities, so that mucociliary clearance efficiency
has to be attested as a function which correlates negatively with
subject age (17).
As underlined by this theoretical study, deposition and
clearance of carcinogenic particles have to be regarded as a
function of subjects’ ages. Nevertheless, it has to be further
noted that also within a specific age group great discrepancies
in particle deposition and clearance, commonly known
as intersubject variability, may occur. This circumstance
significantly influences the precise investigation of relationships
between age and particle behaviour in the human respiratory
tract (37). Therefore, this contribution concerns mean values of
deposition and clearance that have been derived from numerous
inhalation experiments and related hypothetical computations.
According to the study presented here, children develop
protective mechanisms against carcinogens transported as
aerosols in such a way that most particle sizes are already
separated from the inhaled air in both the extrathoracic region
and the main bronchi. The penetration of particular matter
into the alveoli is additionally limited by the shallow breathing
behaviour of infants and children. Nevertheless, the risk of
malignant transformations in the extrathoracic and upper
bronchial compartments should not be underestimated,
especially in regions with enhanced exposure to hazardous
aerosols.
| |||||||||||||||||||||||||||||||||||||||||||||||||
|
Acknowledgements
Disclosure: The authors declare no conflict of interest.
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
References
Cite this article as: Sturm R. Theoretical models
of carcinogenic particle deposition and clearance in
childrens lungs. J Thorac Dis 2012;4(4):368-376. doi:
10.3978/j.issn.2072-1439.2012.08.03
|
|||||||||||||||||||||||||||||||||||||||||||||||||