Right lung cancer with partial anomalous pulmonary venous return and absent right upper lobe
Background
Congenital anomalous conditions such as pulmonary arterial, venous, or bronchial variations are sometimes found. When a vascular shunt is present, major lung resection may cause acute right heart failure. We report a case of ipsilateral partial anomalous pulmonary venous return (PAPVR) with right lung cancer and absent right upper lobe managed by pneumonectomy.
Case presentation
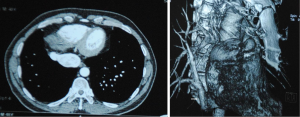
A 48-year-old former smoker presented with a 6-month history of cough and blood sputum. Enhanced computed tomography (CT) demonstrated a mixed-density mass located at right pulmonary hilus without mediastinal lymph node swelling, an anomalous right pulmonary vein draining into inferior vena cava was revealed, bronchus and pulmonary artery of right upper lobe was absent (Figure 1). PAPVR was confirmed. Fiberoptic bronchoscopy revealed occlusion of the B6-10 bronchus by an endobronchial lesion with absence of B1-3 bronchus. Echocardiogram showed normal cardiac function without septal defect [LVIDd (end-diastolic left ventricular internal diameter) 41 mm, IVSd (end-diastolic interventricular septum) 8 mm, LVIDs (end-systolic left ventricular internal diameter) 26 mm, RV (right ventricular) 33 mm, LA (left atrium) 30 mm, RA 35 mm, EF (ejection fraction) 65%]. Blood gas analysis showed a partial pressure of oxygen of 87 mmHg, the carbon dioxide pressure was 45 mmHg in room air.
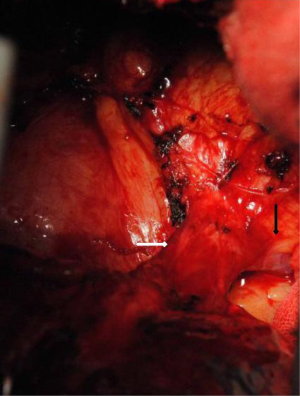
Exploratory thoracotomy revealed only one pulmonary vein draining into inferior vena cava, which was divided at its insertion point (Figure 2). Right upper lobe was absent. Pulmonary artery and bronchus were divided sequentially with lymph nodes dissection. A central type mass with diameter of 3 cm was found in exposure specimen after right pneumonectomy. Pathological examination revealed a T2aN2M0 high-graded squamous cancer. The patient was discharged 12 days post-surgery with an uneventful recovery. Blood gas analysis showed a partial pressure of oxygen of 83 mmHg, the carbon dioxide pressure was 40 mmHg in room air. The patient received radiation therapy and four cycles of chemotherapy. He is now doing well 2 years after operation without relapse or metastasis.
Discussion
PAPVR is a rare congenital anomaly, with a reported incidence of 0.2% to 0.7% (1). One or more branches of pulmonary vein connect with right atrium directly or through systemic circulation by vena cava instead of left atrium. Typically, these anomalies are right sided associated with atrial septal defects, or ventricular septal defect (2).
There have been some reports of pulmonary venous anatomic abnormality recognized during operation. Khasati and colleagues reported a case of an anomalous left superior pulmonary vein requiring anastomosis to the left atrial appendage at the time of lung transplantation (3). Sakurai and associates reported a successful treatment of a 48-year-old man with left lung cancer and contralateral PAPVR (4). Smith and colleagues reported a case of an obstructing left lower lobe carcinoid tumor combined with a PAPVR of the left superior pulmonary vein, it was successfully managed by left lower lobe resection and left superior pulmonary vein connected to the atrial appendage by anastomosis (5). These reports and our case all suggest that thoracic surgeons should consider concommitant pulmonary venous anomalies with careful evaluation of venous return during preoperative work up.
It is quite rare that right anomalous pulmonary venous return combines with absence of right upper lobe and right lung cancer. Since only one pulmonary vein could be found connected with inferior vena cava and lung cancer was located centrally, pneumonectomy was performed. The patient tolerated well without notable descending of arterial oxygen pressure. Patients with PAPVR may present with no symptom, however, PAPVR would affect ventilation/perfusion ratio. Failure to correct the PAPVR at the time of pulmonary resection might potentially increase the left-to-right shunt and right ventricular pressure, sometimes even fatal (6). Black reported a case in which patient developed acute right heart failure with systemic hypotension after a curative right intrapericardial pneumonectomy for primary lung cancer ignoring a major left to right shunt through previously unsuspected partial anomalous venous drainage of the left upper lobe (7). For heart structural anomaly may present with PAPVR, echocardiogram was necessary when chest CT revealed abnormal pulmonary vein return. Invasive cardiac evaluation was not performed in this case, since PAPVR and lung cancer was located at the same side, echocardiographic examination showed good cardiac function. However, it should be considered when such an anomaly was found.
Conclusions
We have described a rare case of ipsilateral PAPVR and lung cancer with absence of right upper lobe. This report highlights the fact that although PAPVR in an adult is uncommon, it should be appropriately managed before pulmonary resection.
Acknowledgements
We are very appreciating of Dr. Mingyue Wan for the pathological interpretation.
Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kavakli K, Gaudet M, Balderson SS, et al. Partial anomalous pulmonary venous return to azygos vein with absent segmental bronchus. Ann Thorac Surg 2013;96:1486. [PubMed]
- Baron N. Association of Left Superior Vena Cava, Sinus Venosus Defect and partial anomalous pulmonary venous return: an echographic and MDCT study. Int J Cardiol 2014;172:e423-4. [PubMed]
- Khasati NH, MacHaal A, Thekkudan J, et al. An aberrant donor pulmonary vein during lung transplant: a surgical challenge. Ann Thorac Surg 2005;79:330-1. [PubMed]
- Sakurai H, Kondo H, Sekiguchi A, et al. Left pneumonectomy for lung cancer after correction of contralateral partial anomalous pulmonary venous return. Ann Thorac Surg 2005;79:1778-80. [PubMed]
- Smith RL 2nd, Zorn GL 3rd, Peeler BB, et al. Combined bronchial sleeve resection and repair of partial anomalous pulmonary venous return. J Thorac Cardiovasc Surg 2006;132:982-3. [PubMed]
- Garg G, Tyagi H, Radha AS. Transcatheter closure of sinus venosus atrial septal defect with anomalous drainage of right upper pulmonary vein into superior vena cava--an innovative technique. Catheter Cardiovasc Interv 2014;84:473-7. [PubMed]
- Black MD, Shamji FM, Goldstein W, et al. Pulmonary resection and contralateral anomalous venous drainage: a lethal combination. Ann Thorac Surg 1992;53:689-91. [PubMed]