
Radiotherapy of brain metastasis from lung cancer in limited resource settings
Introduction
Worldwide lung cancer is the leading cause of cancer related death (1). In developing countries, lung cancer predominantly present in advanced or metastatic setting (2). Brain is one of the most common sites of metastasis in lung cancer which causes severe morbidity and worsens the quality of life. Around 10–15% of the patients present with synchronous brain metastasis and approximately 40–50% will present with brain metastasis during the course of their disease (3,4). A median time of 11 months exists between the appearance of non-small cell lung cancer (NSCLC) all stages combined and brain metastasis (5).
Incidence of brain metastases differ according to the histology of lung cancer (5). The incidence of brain metastasis in squamous and adenocarcinoma is approximately 5% and 10–16% respectively (6,7). Around 23–30% of adenocarcinoma patients will have driver mutations like epidermal growth factor receptor (EGFR) (8,9) and 3–5% have Anaplastic lymphoma kinase (ALK) (10). The baseline incidence of brain metastasis in EGFR mutated patients is around 23–32% (11). In NSCLCs with ALK positivity, incidence of brain metastases is seen in approximately 24% to 42% with increasing risk over time, reaching up to 58% at 3 years (11). With the overall survival (OS) improving due to better systemic therapies including tyrosine kinase inhibitor (TKI), incidence of brain metastasis is also rising in NSCLC.
Treatment of brain metastases in NSCLC consists of whole brain radiation therapy (WBRT), surgical excision, stereotactic radiosurgery (SRS), TKI and best supportive care. Optimal treatment modality generally depends on many factors including age, performance status, and presentation, number of brain lesion and driver mutation status. WBRT is the most widely used treatment modality in limited resource settings for multiple brain metastases. Surgical excision followed by WBRT or SRS with or without WBRT is generally employed for limited metastases usually 1–3 lesions. Treatment patterns of brain metastases in limited resource setting is much different than of developed world due to availability of radiotherapy machines, targeted drugs in spite of substantial differences in molecular profiles of lung cancer patients (12).
The median OS of lung cancer with brain metastases has remain dismal with a median OS of approximately 3–7 months (13-15). Various prognostic criteria like recursive partitioning analysis (RPA) and graded prognostic assessment (GPA) score are available to guide the treatment of brain metastases in NSCLC. Median OS differs depending upon RPA and GPA score. In a study conducted in India (15), 97.3% patients were in RPA class II and III with median OS of 5.2 and 2.6 months compared to 4.2 and 2.3 months respectively in a study by Gaspar et al. (16). Approximately 50.2% and 39.8% patients had GPA score of 1.5–2.5 and 0–1 with median OS of 4 and 2.4 months compared to 5.5 and 3.0 months respectively in a study by Sperduto et al. (17).
Management of brain metastasis in limited resource setting
Presentation
Majority of patients with brain metastasis from lung cancer presents with varied symptoms commonly headache and vomiting (raised intracranial tension), convulsions, gait abnormality, motor deficits like weakness, sensory and cranial nerve deficits depending on the location of the lesion. Approximately 15–20% patients are asymptomatic and detected during normal staging workup (18). Common treatment includes steroids to reduce oedema, anticonvulsants for seizure or prophylactically if brain lesions are located close to the epileptogenic focus. Prophylactic use of anticonvulsants remains controversial, however, in resource constrained setup where accessibility to hospitals is a major challenge many clinicians prefers to prescribe anticonvulsant drugs prophylactically.
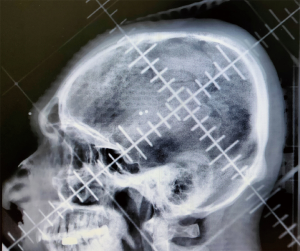
Imaging
The gold standard diagnostic modality for detecting brain metastasis is contrast enhance magnetic resonance imaging (MRI) (Figure 1). However, in a resource constrained setting like India where MRI is not widely available or affordable (19), contrast enhanced computed tomography (CECT) of brain is usually the first ordered investigation because of its availability and a relatively cheaper cost. CECT is less sensitive than MRI in detecting brain lesions as it may not pick up small and non-enhancing lesions. Hence, CECT limits the scope of better prognostication using GPA and score index of radiosurgery system. MRI is essential in detecting number and size of individual brain lesions, leptomeningeal dissemination hence, plays an important role in the treatment decision for brain metastases. In radiotherapy planning, MRI is essential for precision treatment like SRS and for close follow up after SRS, observation and differentiating pseudoprogression from true progression. In a resource constrained setting where MRI is not usually performed for diagnosing brain metastases, treatment options like WBRT is the commonly used safe technique for majority of patients.

Treatment
The treatment of lung cancer patients with brain metastases generally depends upon age, performance status, number of brain metastasis, primary disease status, extracranial disease, histology and molecular signature of the tumour tissue. Prognostic scores like GPA and RPA guide the treatment decisions based on the above factors. Various treatment modalities like surgery, radiation therapy and tyrosine kinase inhibitors individually or in combination plays a vital role.
Radiation therapy (RT) plays the most vital role in the treatment of brain metastases, as most of the chemotherapy drugs are known to have poor CNS penetration due to presence of blood-brain barrier, which makes brain as pharmacological sanctuary. Radiation therapy for brain metastases is being used for almost 5–7 decades with WBRT being the most common technique. Advanced techniques like SRS or hippocampal sparing WBRT are the new armamentarium in the radiation therapy.
Whole brain radiotherapy (WBRT) using German helmet or slanting field technique are the most commonly used technique for radiation delivery in developing countries (Figure 2). These techniques are simple, easy to perform and are of low cost making them widely popular in a busy centre with limited facilities. Patients usually have poor performance status, multiple lesions and limited finances hence by default WBRT is the treatment of choice. Various dose fractionation schedules like 12 Gy in 2 fractions once weekly, 20 Gy in 5 fractions once daily and 30 Gy in 10 fractions once daily over 2 weeks are the commonly employed dose regimens. Based on the prognostic scores, physician preference, institutional and patient logistics, dose fractionation schedule is decided. In patients with poor prognosis, poor PS and difficulty in travelling daily to hospitals, 12 Gy in two fractions once weekly is also used as a palliative dose regimen. These group of patients generally do not survive much to experience neurotoxicity because of large dose per fraction, however, use of this regimens should be questioned especially after the publications of Quartz study and targeted therapy (20,21). In patients with relatively better performance status, protracted schedules are usually preferred depending upon institutional practice.
In a tertiary cancer centre of India, the short course accelerated radiotherapy regimen (SCAR) i.e., 20 Gy in 5 fractions, radio biologically equivalent dose fractionation schedule to cater a large population is the most commonly used dose regimen with equivalent survival in RPA class II and III. This finding is particularly vital in large volume centres with limited resources and long waiting list in developing countries (14). Less than 10% of patients had received 30 Gy in 10 fractions which is usually prescribed in a good prognostic score patients or as a post-operative regimen.
SRS is indicated for 1–3 metastatic brain lesion with or without WBRT. SRS alone results in less neurocognitive decline but with higher intracranial failure rate than combined with WBRT (22). SRS combined with WBRT results in OS benefit in good prognosis patients compared with SRS alone (23). Penetration of SRS in community practice settings is limited in resource constrained setting due to various reasons, namely, lack of expertise, lack of infrastructure, lack of eligible patients, cost and follow up surveillance with MRI brain. Patients of young age, good PS, favourable histology, tumours with driver mutation, controlled primary and low extracranial disease burden are generally offered SRS with or without WBRT. Number of eligible patients are very less especially in developing countries where majority presents with widespread metastases and poor PS. There is a clear disparity of SRS facilities in community and corporate centres which routinely practice SRS for eligible patients. However, with the increasing numbers of community centres getting equipped with modern radiotherapy machines, we hopefully expect the increased use of SRS treatment in eligible patients.
Effect of neurocognitive decline with WBRT is well documented in literature (24). Gondi et al. has suggested hippocampal sparing WBRT technique to preserve neurocognitive function (NCF) in brain metastases patients (25). However, similar to SRS, majority of the patients would not be a candidate for hippocampal sparing WBRT for similar reasons. Also, neurocognitive function testing is very rarely done in developing countries except few tertiary cancer centres. Many of the centres including ours used a technique of WBRT with simultaneous integrated boost (SIB) and hippocampal avoidance (HA) which gives you the benefit of less intracranial failure rate, higher doses to brain lesions and preserved NCF in patients with 1–3 brain metastases (26,27). This technique is being seen as an alternative to SRS as less intracranial failure rate is expected due to whole brain irradiation, however, evidence is still evolving and no definite conclusion can be made. Applicability of WBRT with SIB and HA especially in limited resource setting is very limited similar to SRS, and practiced in few tertiary cancer centres in good prognostic group of patients.
In poor prognostic group patients like RPA class III and GPA score 0–2, the role of WBRT is questioned by the results of Quartz trial. In a retrospective study of Tibdewal et al., approximately 25% patients succumbed to the disease within 30 days of diagnosis of BM, (16.5% patients belonged to RPA class I–II and 36.4% patients had GPA score of ≥2.5). The group suggested to accurately identify these patients and provide them best supportive care so that limited RT resources could be properly channelized in a limited resourced setting. The QUARTZ trial also concluded that in poor prognostic group like RPA III omitting WBRT did not affect QOL and OS (20). The Quartz trial results were applied in a clinical practice setting of limited resource in India (28). Median OS of 70 days probability was considered the cut off for stratifying the patients to institute optimal supportive care versus WBRT. A prognostic modelling was proposed taking in to account age, sex, KPS, number of brain metastases, extracranial disease status, type of metastases, EGFR status and neuro-deficits to categorise patients to high, intermediate and low risk depending on the total scoring and probability of survival in days. This study reports that patients with probability of survival of less than 70 days can be chosen to omit WBRT. Decision for optimal supportive care is predominantly based on performance status assessed by physician and it has been reported to have interobserver variation due to inherent subjectivity of it. Agarwal et al. has compared physician assessed and patient reported PS in a prospective study and has concluded that patient reported PS has the same prognostic information (29).
Role of RT in molecular era
TKI therapy has changed the management of metastatic NSCLC harbouring driver mutations to EGFR and ALK. Many second or third generation TKI have good CNS penetration rate. Approximately 23–31% of patients with driver mutations will have BM at presentation (11,21,30,31). Because of the improved survival in this cohort of patients, incidence of brain metastases has also increased considerably. Approximately 10–20% of driver mutation positive patients with BM are asymptomatic. The management remains the same for symptomatic patient as in non-mutated patients. However, for asymptomatic patients there is a therapeutic dilemma as to administer upfront brain radiation or not. There is a growing trend to withhold/reserve cranial RT in asymptomatic patients until symptomatic or documented cranial progression. This approach might not be feasible with first and second generation TKI since they have limited penetration to central nervous system (32). Retrospective studies and meta-analysis have shown inferior survival outcomes and shorter intracranial control rate with TKI alone than combination of cranial RT and TKI (33,34). In contrast, third generation TKI have better penetration to central nervous system and role of upfront cranial RT may be questioned (21,31).
Issues in withholding cranial RT
First, availability of second or third generation TKI with good CNS penetration is limited in developing countries because of cost. Clinical trials and patient support programmes are very beneficial for making these drugs accessible to eligible patients. Second, regular surveillance MRI is must at follow-up to document radiological progression. Cost and availability of MRI brain is a major hindrance in a limited resource setting. Third, in our clinical experience, CNS symptoms usually develop immediately when patient temporarily stops or withhold TKI due to cost or non-availability of drugs. Fourth, basic awareness of CNS related symptoms and early access to MRI also pose a significant challenge. Hence, the authors believe in affordable aware patients at a tertiary cancer centre or corporate hospitals, withholding cranial RT might be an option but treatment with only TKI in a patient with known CNS metastases is not an option at present.
In case of limited and asymptomatic CNS progression with good extracranial control, focal RT in the form of SRS/SRT to the progressive lesion could also be considered along with continuation of the same TKI. In case of multiple CNS site progression, WBRT with switching to higher generation TKI with higher CNS efficacy is warranted. However, in clinical practice, such treatment decisions cones down to the limited and financial resources of RT and higher generation TKI.
Re-irradiation for brain metastases
With the improved survival due to better systemic chemotherapeutic drugs and TKI, many patients present with symptomatic CNS progression after WBRT, hence warrants the need of re-irradiation. It could be either focal or to whole brain depending upon the number of lesions. Decision of re-WBRT is challenging and has to be taken in consideration with age, performance status, driver mutation status, status of primary disease, progression free survival, time since prior irradiation and neuro-cognitive decline. There are no standard dose fractionation regimens exist for re-WBRT. Dose schedule commonly used are 25 Gy in 10 fractions or 20 Gy in 5 fractions. Agarwal et al. has shown that less than 10% of patients actually received re-WBRT and majority of them were driver mutation positive with a median interval of 17.1 months from the date of first WBRT (35).
Conclusions
Lung cancer with brain metastasis is in its rising trend across developing countries due to increased life expectancy because of improved radiotherapy techniques and better systemic drugs. However, there is a clear disparity among the developed and developing countries in the management of brain metastases due to limited resources and its availability. Hence, the research data generated from the developed world may not be applicable in clinical practice of developing world owing to differences in clinical and treatment patterns. First, SRS is indicated for limited brain metastases for better intracranial control, however, the availability of SRS and MRI in limited resource setting is limited. Hence, in limited resource setting where basic oncological treatment options are limited, to say, SRS is the treatment of choice for better intracranial control and neurocognitive function might not be correct. Also, there should be a cost effective analysis in developing world comparing SRS with WBRT and WBRT alone with respect to OS and quality of life. Second, the emerging trend of observation as compared to cranial irradiation in driver mutated patients might not be applicable in developing countries as a cost effective approach since it requires close surveillance with regular follow up MRI. Hence, the approach of observation compared with WBRT in asymptomatic NSCLC patients should be examined in a clinical trial with cost effective analysis in a limited resource setup. Focus should also be on generating one’s own data so that it is more relevant and applicable in clinical practice (36). There should also be a concerted effort between developed and developing world for collaboration in clinical research of brain metastases from lung cancer especially given the fact that approximately one-third of these patients are driver mutated. In the near future, we hope to see a better change in the radiotherapy techniques, generation of good quality of data and availability of higher generation TKI at a cheaper cost for eligible patients at community level practice in limited resource countries.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Lucyna Kepka) for the series “Radiotherapy for Brain Metastases from Lung Cancer” published in Journal of Thoracic Disease. The article has undergone external peer review.
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form, available at: http://dx.doi.org/10.21037/jtd-2019-rbmlc-02. The series “Radiotherapy for Brain Metastases from Lung Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Reference
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Noronha V, Dikshit R, Raut N, et al. Epidemiology of lung cancer in India: Focus on the differences between non-smokers and smokers: A single-centre experience. Indian J Cancer 2012;49:74-81. [Crossref] [PubMed]
- Li N, Zeng ZF, Wang SY, et al. Randomized phase III trial of prophylactic cranial irradiation versus observation in patients with fully resected stage IIIA-N2 nonsmall-cell lung cancer and high risk of cerebral metastases after adjuvant chemotherapy. Ann Oncol 2015;26:504-9. [Crossref] [PubMed]
- Mamon HJ, Yeap BY, Jänne PA, et al. High risk of brain metastases in surgically staged IIIA non-small-cell lung cancer patients treated with surgery, chemotherapy, and radiation. J Clin Oncol 2005;23:1530-7. [Crossref] [PubMed]
- Berghoff AS, Schur S, Füreder LM, et al. Descriptive statistical analysis of a real life cohort of 2419 patients with brain metastases of solid cancers. ESMO Open 2016;1:e000024 [Crossref] [PubMed]
- Lee H, Jeong SH, Jeong BH, et al. Incidence of Brain Metastasis at the Initial Diagnosis of Lung Squamous Cell Carcinoma on the Basis of Stage, Excluding Brain Metastasis. J Thorac Oncol 2016;11:426-31. [Crossref] [PubMed]
- Yang B, Lee H, Um SW, et al. Incidence of brain metastasis in lung adenocarcinoma at initial diagnosis on the basis of stage and genetic alterations. Lung Cancer 2019;129:28-34. [Crossref] [PubMed]
- Chougule A, Prabhash K, Noronha V, et al. Frequency of EGFR mutations in 907 lung adenocarcioma patients of Indian ethnicity. PLoS One 2013;8:e76164 [Crossref] [PubMed]
- Wu YL, Zhong WZ, Li LY, et al. Epidermal Growth Factor Receptor Mutations and Their Correlation with Gefitinib Therapy in Patients with Non-small Cell Lung Cancer: A Meta-Analysis Based on Updated Individual Patient Data from Six Medical Centers in Mainland China. J Thorac Oncol 2007;2:430-9. [Crossref] [PubMed]
- Dearden S, Stevens J, Wu YL, et al. Mutation incidence and coincidence in non small-cell lung cancer: meta-analyses by ethnicity and histology (mutMap). Ann Oncol 2013;24:2371-6. [Crossref] [PubMed]
- Rangachari D, Yamaguchi N, VanderLaan PA, et al. Brain metastases in patients with EGFR-mutated or ALK-rearranged non-small-cell lung cancers. Lung Cancer 2015;88:108-11. [Crossref] [PubMed]
- Agarwal JP, Lee VHF. East Meets West: Convergence of the Art and Science of Oncology. Clin Oncol (R Coll Radiol) 2019;31:487-9. [Crossref] [PubMed]
- Sperduto PW, Kased N, Roberge D, et al. Effect of tumor subtype on survival and the graded prognostic assessment for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys 2012;82:2111-7. [Crossref] [PubMed]
- Agarwal JP, Wadasadawala T, Munshi A, et al. Validation of Recursive Partitioning Analysis Classification in Patients with Brain Metastases from Non-small Cell Lung Cancer Treated with Short-course Accelerated Radiotherapy. Clin Oncol (R Coll Radiol) 2010;22:837-43. [Crossref] [PubMed]
- Tibdewal A, Pathak R, Laskar SG, et al. Prognostic Factors and Survival Outcomes of Lung Cancer Patients with Brain Metastasis: Experience of a Tertiary Cancer Centre. J Brain Tumors Neurooncol 2016;1:106.
- Gaspar L, Scott C, Rotman M, et al. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 1997;37:745-51. [Crossref] [PubMed]
- Sperduto CM, Watanabe Y, Mullan J, et al. A validation study of a new prognostic index for patients with brain metastases: the Graded Prognostic Assessment. J Neurosurg 2008;109:87-9. [Crossref] [PubMed]
- Niviere P, Sculier JP, Meert AP, et al. Impact de l’imagerie cérébrale systématique dans le bilan initial des cancers du poumon. Rev Mal Respir 2018;35:55-61. [Crossref] [PubMed]
- Jankharia GR. Commentary - radiology in India: the next decade. Indian J Radiol Imaging 2008;18:189-91. [Crossref] [PubMed]
- Mulvenna P, Nankivell M, Barton R, et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiorit. Lancet 2016;388:2004-14. [Crossref] [PubMed]
- Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in Untreated EGFR -Mutated Advanced Non-Small-Cell Lung Cancer . N Engl J Med 2018;378:113-25. [Crossref] [PubMed]
- Brown PD, Jaeckle K, Ballman KV, et al. Effect of Radiosurgery Alone vs Radiosurgery With Whole Brain Radiation Therapy on Cognitive Function in Patients With 1 to 3 Brain Metastases: A Randomized Clinical Trial. JAMA 2016;316:401-9. [Crossref] [PubMed]
- Sperduto PW, Shanley R, Luo X, et al. Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1-3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys 2014;90:526-31. [Crossref] [PubMed]
- Li J, Bentzen SM, Li J, et al. Relationship Between Neurocognitive Function and Quality of Life After Whole-Brain Radiotherapy in Patients With Brain Metastasis. Int J Radiat Oncol Biol Phys 2008;71:64-70. [Crossref] [PubMed]
- Gondi V, Pugh SL, Tome WA, et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): A phase II multi-institutional trial. J Clin Oncol 2014;32:3810-6. [Crossref] [PubMed]
- Hsu F, Carolan H, Nichol A, et al. Whole brain radiotherapy with hippocampal avoidance and simultaneous integrated boost for 1-3 brain metastases: a feasibility study using volumetric modulated arc therapy. Int J Radiat Oncol Biol Phys 2010;76:1480-5. [Crossref] [PubMed]
- Oehlke O, Wucherpfennig D, Fels F, et al. Whole brain irradiation with hippocampal sparing and dose escalation on multiple brain metastases. Strahlenther Onkol 2015;191:461-9. [Crossref] [PubMed]
- Agarwal JP, Chakraborty S, Laskar SG, et al. Applying the QUARTZ Trial Results in Clinical Practice: Development of a Prognostic Model Predicting Poor Outcomes for Non-small Cell Lung Cancers with Brain Metastases. Clin Oncol (R Coll Radiol) 2018;30:382-90. [Crossref] [PubMed]
- Agarwal JP, Chakraborty S, Laskar SG, et al. Prognostic value of a patient-reported functional score versus physician-reported Karnofsky Performance Status Score in brain metastases. Ecancermedicalscience 2017;11:779. [Crossref] [PubMed]
- Guérin A, Sasane M, Zhang J, et al. Brain metastases in patients with ALK+ non-small cell lung cancer: clinical symptoms, treatment patterns and economic burden. J Med Econ 2015;18:312-22. [Crossref] [PubMed]
- Gadgeel S, Peters S, Mok T, et al. Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALKþ) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann Oncol 2018;29:2214-22. [Crossref] [PubMed]
- Costa DB, Shaw AT, Ou SHI, et al. Clinical experience with crizotinib in patients with advanced ALK-rearranged non-small-cell lung cancer and brain metastases. J Clin Oncol 2015;33:1881-8. [Crossref] [PubMed]
- Soon YY, Leong CN, Koh WY, et al. EGFR tyrosine kinase inhibitors versus cranial radiation therapy for EGFR mutant non-small cell lung cancer with brain metastases: A systematic review and meta-analysis. Radiother Oncol 2015;114:167-72. [Crossref] [PubMed]
- Gerber NK, Yamada Y, Rimner A, et al. Erlotinib versus radiation therapy for brain metastases in patients with EGFR-mutant lung adenocarcinoma. Int J Radiat Oncol Biol Phys 2014;89:322-9. [Crossref] [PubMed]
- Agarwal JP, Karmakar S, Mummudi N, et al. EP-1362 Re-Irradiation Of Whole Brain For Symptomatic Progression In Lung Cancer Patients. Radiother Oncol 2019;133:S744. [Crossref]
- Aggarwal J, Chakraborty S, Ghosh Laskar S, et al. Reference Data for Standardized Quality of Life Questionnaires in Indian Patients with Brain Metastases from Non-small Cell Lung Cancer: Results from a Prospective Study. Cureus 2017;9:e1149 [Crossref] [PubMed]


