Transcatheter arterial embolization for intercostal arterial bleeding in a patient after chest tube insertion
Introduction
Transcatheter arterial embolization (TAE) for treatment of thoracic disease is mainly applied in the setting of massive hemoptysis and progressively enlarging hemothorax. Progressive hemothorax is known to have a variety of etiologies; usually the sources of bleeding are the aorta and intercostals and pulmonary vessels (1). Contrast enhanced CT plays a significant role in localizing bleeding points (2). When contrast CT is non-diagnostic, exploratory thoracotomy, video-assisted thoracic surgery (VATS) exploration or angiography are usually considered. We present a case of iatrogenic massive bleeding, with retrograde radiography revealing bleeding points. The patient was successfully treated using TAE.
Case report
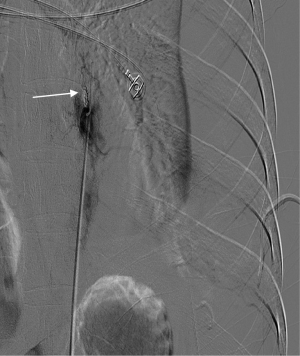
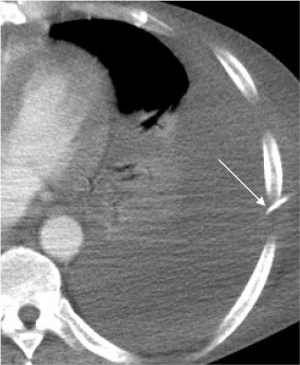
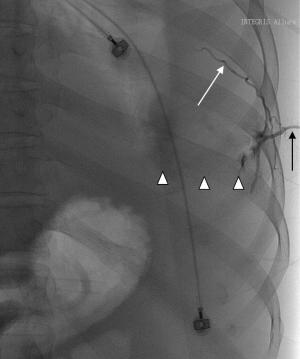
Our patient was a 54-year-old man who underwent emergent gastrorrhaphy due to gastric perforation, with a history of alcoholic cirrhosis for 15 years. A central venous puncture tube with side holes was inserted into the left 7th intercostal space for pleural effusion, and an average 500 mL of yellowish liquid was drained every day. On the 10th day after tube insertion, more than 1,000 mL of bloody fluid was suddenly drained. Fluid analysis revealed presence of whole blood, and the patient went into hypovolemic shock (emergent full blood count revealed a haemoglobin of 5.7 g/dL, platelet count of 28×109/L;and prothrombin time of 26.8 s, INR 2.54). The patient recovered from hemorrhagic shock after massive blood and fluid transfusion. Emergency chest CT scans with contrast revealed no exact point of contrast extravasation (Figure 1). However, bloody fluid was continually drained from the tube. Due to the unstable hemodynamic condition and coagulation disorders of the patient, VATS and exploratory laparotomy were deemed to not be tolerated well. Angiography was considered with continuous blood and fluid transfusion. Because no exact contrast extravasation was found on CT, retrograde angiography was performed via the chest tube and it revealed the left 7th intercostal artery (Figure 2). Subsequent transcatheter intercostal artery angiography through the right femoral artery revealed extravasation from the left 7th intercostal artery (Figure 3) and TAE was performed utilizing gelatin sponge particles and 2 coils. The extravasation of the contrast medium ceased (Figure 4) after embolization and the patient’s hemodynamic condition stabilized without massive fluid resuscitation being necessary.

Discussion
Chest tube insertion is a common procedure in the management of air and fluid collection within the pleural space. The procedure is considered safe but serious complications are encountered even in the hands of experienced personnel (3-5). Common complications include tube displacement, injury to chest wall vessels and to major cardiac and intrathoracic vascular structures (6). The rate of serious complication was reported to be around 2-3% (7). Among all the complications, injury to vessels leading to hemothorax or hematoma was the commonest, potentially leading to hypovolemic shock or sudden death (4). In our case, 10 days after chest tube insertion, the patient went into shock due to massive chest tube bleeding. Intercostal arteriography revealed contrast extravasation from the left 7th intercostal artery directly into the chest tube, and we assumed that tube displacement injured the intercostal artery and the side hole of the tube connected to the ruptured artery by chance. This resulted in little blood remaining in the pleural cavity and a lack of a hematoma in the thoracic wall. Contrast enhanced CT therefore could not detect active contrast extravasation.
When a patient is hemodynamically unstable, contrast-enhanced computed tomography (CECT) can detect the site of active bleeding in many cases, helping to direct angiographic embolization for haemostasis (8,9). In pulmonary injury associated with severe rib fracture, CECT is indicated when ≥200 mL/h of blood drains from the chest tube (2). However, when contrast CT is negative, exploratory thoracotomy and VATS should be considered in the absence of a coagulopathy. In our case, prothrombin time barely met the requirements of angiography and the patient’s hemodynamic condition remained unstable even with massive fluid and blood transfusion. Retrograde radiography was performed via the chest tube in order urgently locate the bleeding point, and we located the ruptured artery.
TAE is widely used to manage active bleeding in splenic, hepatic, and renal injury, as well as pelvic fractures in trauma patients (10). This modality is also an effective method of hemostasis that minimizes iatrogenic injury in trauma patients with hemothorax, which is much less invasive than a thoracotomy (2,11-14). Our patient was not a suitable candidate for surgery or VATS; TAE therefore became the most effective and minimally invasive method of choice.
In conclusion, retrograde tube radiography may be an alternative method for cases with the massive bleeding from drainage tubes, which can assist in localization of bleeding points.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Muthuswamy P, Samuel J, Mizock B, et al. Recurrent massive bleeding from an intercostal artery aneurysm through an empyema chest tube. Chest 1993;104:637-9. [PubMed]
- Hagiwara A, Yanagawa Y, Kaneko N, et al. Indications for transcatheter arterial embolization in persistent hemothorax caused by blunt trauma. J Trauma 2008;65:589-94. [PubMed]
- Sundaramurthy SR, Moshinsky RA, Smith JA. Non-operative management of tube thoracostomy induced pulmonary artery injury. Interact Cardiovasc Thorac Surg 2009;9:759-60. [PubMed]
- Menger R, Telford G, Kim P, et al. Complications following thoracic trauma managed with tube thoracostomy. Injury 2012;43:46-50. [PubMed]
- Sethuraman KN, Duong D, Mehta S, et al. Complications of tube thoracostomy placement in the emergency department. J Emerg Med 2011;40:14-20. [PubMed]
- Kao CL, Lu MS, Chang JP. Successful management of pulmonary artery perforation after chest tube insertion. J Trauma 2007;62:1533. [PubMed]
- Rombolá CA, Tomatis SB, Honguero Martínez AF, et al. Parapneumonic pleural effusion. Accidental insertion of a chest tube into right pulmonary artery. Eur J Cardiothorac Surg 2008;34:903. [PubMed]
- Boersma WG, Stigt JA, Smit HJ. Treatment of haemothorax. Respir Med 2010;104:1583-7. [PubMed]
- Khalil MW, Cleveland TJ, Sarkar PK, et al. Successful angiographic embolisation of bleeding into the chest wall after chest drain insertion. Interact Cardiovasc Thorac Surg 2009;8:166-7. [PubMed]
- Hastings GS. Angiography and intervention radiology. In: Mirvis SE, Shanmuganathan K, editors. Imaging in Trauma and Critical Care. 2nd ed. Philadelphia: Saunders; 2003:607-29.
- Hagiwara A, Iwamoto S. Usefulness of transcatheter arterial embolization for intercostal arterial bleeding in a patient with burst fractures of the thoracic vertebrae. Emerg Radiol 2009;16:489-91. [PubMed]
- Carrillo EH, Heniford BT, Senler SO, et al. Embolization therapy as an alternative to thoracotomy in vascular injuries of the chest wall. Am Surg 1998;64:1142-8. [PubMed]
- Matsumoto H, Suzuki M, Kamata T, et al. Intercostal artery injuries treated by angiographic embolization: case report. J Trauma 1998;44:392-3. [PubMed]
- Kessel B, Alfici R, Ashkenazi I, et al. Massive hemothorax caused by intercostal artery bleeding: selective embolization may be an alternative to thoracotomy in selected patients. Thorac Cardiovasc Surg 2004;52:234-6. [PubMed]