
Effect of an unsupervised walking program on tolerance to exercise in patients with chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a preventable disease characterized by persistent respiratory symptoms and airflow limitation that is usually caused by the exposure to harmful particles, mainly tobacco smoke (1). In the course of the disease, lung function deteriorates, exercise tolerance decreases and quality of life worsens. All these factors contribute to an increased risk of death. Exercise intolerance measured with a 6-minute walk test (6MWT) is a powerful indicator of health deterioration and a predictor of prognosis (2). An increase of 30 meters in this test is considered the minimal clinically relevant distance to consider effective any intervention (3). This test assesses disability as well as the effectiveness of pulmonary rehabilitation (4). Furthermore, it is safe, reproducible, and inexpensive and can assess the overall pulmonary, cardiovascular and muscular system functions (5). It is also well known that low physical activity, associated with poor mobility, has been related with worse prognosis (6). Furthermore, sedentary lifestyle in COPD patients is an independent predictor of mortality and exacerbations (6). Avoiding sedentary lifestyle and increasing physical activity is an important component in a respiratory rehabilitation plan. For this purpose, pedometers may play a role as they are small, portable devices that determine the number of steps a subject walks during the day and have been frequently used in patients with COPD (7). However, there are few studies analysing the impact of unsupervised physical activity on exercise capacity in COPD patients. The objective of the present study was to determine the effect of an unsupervised walking program on exertion capacity and tolerance and peripheral oxygen saturation (SpO2) measure in the 6MWT in COPD subjects without an indication of chronic oxygen therapy.
We designed a prospective, consecutive sample, single-centre study that included patients with previous diagnosis of COPD according to the global strategy for the diagnosis, management, and prevention of COPD [Global Initiative for Chronic Obstructive Lung Disease (GOLD)] [post-bronchodilator forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC) ratio <0.70]. Subjects between 45 and 75 years old, which had a SpO2 baseline greater than 93% and classified as sedentary [scoring less than 51 in the Yale Physical Activity Survey (YPAS) questionnaire] were consecutive recruited between October 2017 and June 2018 at the tertiary Reina Sofia University Hospital in Córdoba (Spain). Patients that had any contraindication to undergo a 6MWT, those who have had an exacerbation in the last 6 weeks or had a severe comorbidity with a vital prognosis of less than 6 months were excluded. Patients were verbally encouraged to increase their physical activity and were given counselling by a list of general recommendations that included best hours to do the activity, some personalized street walking circuits and dietary habits including Mediterranean diet between others at each visit (baseline and 3rd month). They were also provided with a follow-up diary and instructed to record information each week. Regular physical activity was monitored with a pedometer (Geonaute ONstep400®, Oxylane, France) with the ability to store daily data over a week. 6MWT was performed following actual recommendations (8). Demographic data, age, gender, body mass index (BMI), comorbidity (Charlson index), FEV1, dyspnea according to the modified Medical Research Council (mMRC) and 6MWT results were recorded. An increase of more than 600 between the steps performed in the baseline week and the average number of steps during the last 4 weeks of the program was considered to be compliant with the program. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by committee ethics board of Hospital Universitario Reina Sofia of Córdoba (NO.: 3502). All patients included gave informed consent to participate in the study.
Sample size was calculated based on data of the intervention effect to achieve 1,100 steps/day (9). The sample size calculation (two-tailed) to achieve a power of 0.8 with a significance level of α=0.05 was 44 patients. To mitigate the possible effect of lost data, a 15% increase was added with a final sample size of 51 individuals.
For the comparison of (baseline) means at the beginning of the study and means at the end of the study, Student’s t-test for paired samples was used. In the case of data not being normally distributed, Wilcoxon’s non-parametric test was used. All comparisons were two-tailed. The statistical significance threshold for all values was set at P<0.05.
Sixty-six patients were eligible during the recruitment period, 8 of them did not gave consent to be included. Of the remaining 58 patients, 2 (3.4%) did not complete the follow-up program and 1 (1.7%) had erroneously completed the follow-up diary. The mean age of the included population was 65±4.1 years, 90% men, 80% ex-smokers, mean BMI 30±3.1 kg/m2, FEV1 51%±11.2%, Charlson index 3.8±0.74 and mMRC 1.7±0.56.
When comparing baseline characteristics and mean in the 12 weeks, a significant increase in distance travelled (2,932±1,855.9 vs. 4,397±1,404.1 steps/day; P<0.001) respectively was observed, with a difference in means of 1,465 steps (95% CI: 1,181–1,749; P<0.001). At the end of the 6MWT, significant changes in baseline and after intervention in the degree of dyspnea (6.3±1.4 vs. 5.3±1.9; P=0.001) and exertion tolerance (15±2.0 vs. 14±2.7; P=0.017) in Borg scale were also observed. There were no significant differences in baseline, minimum, mean or end-of-test SpO2 value.
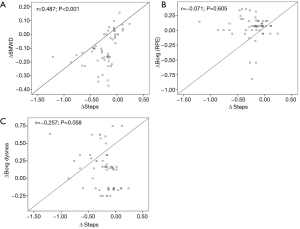
When the increase of steps between the first week and twelfth week were correlated, it was found a positive correlation with the meters walked in the 6MWT and negative with the increase in perceived exertion and dyspnea measured by the Borg scale (Figure 1).
Finally, 64% of patients (35/55) increased significantly the distance walked in the 6MWT (>30 meters). This was driven mainly by the group of patients who had an increase of more than 600 steps/day between the first and last week (P<0.001).
The present study shows that in sedentary patients with COPD, a counselling program encouraging physical activity and the help of a pedometer is effective to increase physical activity and has a direct impact on the distance walked in the 6MWT.
Our study shows that there is a significant increase in the distance walked of more than 30 meters in the 6MWT in up to 63% of the patients. This could have a prognostic and economic impact on this type of patient with minimal intervention and low cost.
A limitation of this study is that the short follow-up of patients and the absence of a maintenance program after week 12 have not allowed us to determine the continuity of the results over time and their real prognostic impact (10). The absence of a control group also limits the strength of the study. In addition, the variables determined in the first week may have a non-response bias as they are influenced by the delivery of the pedometer and inclusion in the study.
The results obtained suggest that in COPD patients, verbal encouragement and an unsupervised walking program effectively in increase exercise capacity and improve exercise tolerance, reinforcing the role of physical activity in this type of patient. However, more long-term studies are required to confirm if our results are maintained over time and their real prognostic impact.
Acknowledgments
Funding: This work was supported by Esteve Pharmaceuticals SA, Barcelona, Spain.
Footnote
Provenance and Peer Review: This article was a free submission to the journal. The article was sent for external peer review.
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-2272
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-2272). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2020 report). Available online: https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf
- Durheim MT, Smith PJ, Babyak MA, et al. Six-minute-walk distance and accelerometry predict outcomes in chronic obstructive pulmonary disease independent of Global Initiative for Chronic Obstructive Lung Disease 2011 Group. Ann Am Thorac Soc 2015;12:349-56. [Crossref] [PubMed]
- Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J 2014;44:1447-78. [Crossref] [PubMed]
- Puente-Maestu L, Palange P, Casaburi R, et al. Use of exercise testing in the evaluation of interventional efficacy: an official ERS statement. Eur Respir J 2016;47:429-60. [Crossref] [PubMed]
- Casas A, Vilaro J, Rabinovich R, et al. Encouraged 6-min walking test indicates maximum sustainable exercise in COPD patients. Chest 2005;128:55-61. [Crossref] [PubMed]
- Furlanetto KC, Donária L, Schneider LP, et al. Sedentary Behavior Is an Independent Predictor of Mortality in Subjects With COPD. Respir Care 2017;62:579-87. [Crossref] [PubMed]
- Mendoza L, Horta P, Espinoza J, et al. Pedometers to enhance physical activity in COPD: a randomised controlled trial. Eur Respir J 2015;45:347-54. [Crossref] [PubMed]
- Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 2014;44:1428-46. [Crossref] [PubMed]
- Demeyer H, Burtin C, Hornikx M, et al. The Minimal Important Difference in Physical Activity in Patients with COPD. PLoS One 2016;11:e0154587. [Crossref] [PubMed]
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013;188:e13-64. Erratum in: Am J Respir Crit Care Med. 2014 Jun 15;189(12):1570. [Crossref] [PubMed]


