
Postoperative hypothermia after total aortic arch replacement in acute type A aortic dissection—multivariate analysis and risk identification for postoperative hypothermia occurrence
Introduction
Postoperative hypothermia (PH) is a common physiological abnormality after non-cardiac surgery (1-4). Evidences show PH is associated with increased postoperative morbidity and mortality (5-7). Patients with PH have higher incidence of infection, more blood products consumption, longer mechanical ventilation time and length of hospital stay (8,9).
Risk factors of PH have been identified in previous studies including age, revised cardiac risk index (RCRI, in non-cardiac surgery), preoperative and intraoperative hypothermia, prolonged duration of anesthesia (3,10). A large proportion of patients undergoing cardiac surgery have the abovementioned features. Other than that, patients with acute type A aortic dissection undergoing total arch replacement require deep hypothermic circulatory arrest (DHCA), large volumes of blood products and fluid infusion, and extended operative time. They also have compromised peripheral circulation secondary to dissected arteries which can decelerate the rewarming rate. All these features predispose this population to develop PH.
Several studies have discussed the association between PH and cardiac surgery, which demonstrate that, patients with PH have higher incidence of bleeding, infection and mortality after elective cardiac surgery (11). Bleeding and infection are the major adverse effects of PH, which may significantly compromise the outcomes after total arch replacement.
However, study about PH after arch surgery in acute type A aortic dissection is limited. We felt it was critical to conduct a study to investigate the incidence, risk factors of PH and its impact on early outcomes in this setting.
We present the following article in accordance with the “Strengthening The Reporting of Observational Studies in Epidemiology (STROBE) Statement” reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-1709).
Methods
Study population
From January 2013 to December 2016, consecutive 382 patients with acute type A aortic dissection underwent aortic repair at our institution. Patients underwent total arch replacement were enrolled into this study. Patients with coronary, visceral or peripheral arteries malperfusion related to acute dissection were excluded. Patients with documented active infection prior to surgery were excluded. Patients were divided into the PH and non-PH groups, according to the occurrence of PH (defined as the bladder temperature <36.0 °C upon ICU admission after surgery). A case-control study was conducted to determine the risk factors of PH, and the impact of PH on early outcomes were also investigated.
Surgical technique
All cases were performed under DHCA with anterograde selective cerebral perfusion through sternotomy. Bilateral percutaneous cerebral oxygenation saturation monitoring was routinely used. Both the nasopharyngeal and the bladder temperature were recorded continuously. The cardiopulmonary bypass (CPB) was established through right (or left) common femoral artery, right axillary artery and right atrium appendage cannulation. A retrograde cannula was inserted into the coronary sinus through the right atrium. After the ascending aorta was cross-clamped and opened, 4 °C Del Nido cardioplegia solution was given directly through coronary ostia followed by intermittent retrograde perfusion every 60 to 90 minutes. Topical cooling of the head and the heart with ice slush was routinely used during DHCA and myocardial ischemia, respectively.
During cooling, the aortic root was dissected and inspected. DHCA was instituted after the nasopharyngeal temperature reached 22 °C. Unilateral cerebral perfusion was administrated at 10 mL/Kg/min through right axillary artery. The entire aortic arch was resected. The innominate artery, the left common carotid artery and the left subclavian artery were amputated and anastomosed, respectively. It was at surgeon’s discretion whether or not a stent elephant trunk repair with a stent graft (MicroPort Medical Co Ltd., Shanghai, China) was needed. A 4-branched graft (Gelweave ValsalvaTM TERUMO, Tokyo, Japan) was used to replace the total arch. The distal arch anastomosis was performed first. The graft was cross-clamped at the ascending aorta level and the femoral artery perfusion reinitiated. Then the left common carotid artery anastomosis was completed and rewarming initiated.
The rewarming target was set at bladder temperature 36.0 °C. Force-air and blanket rewarming were used besides systemic rewarming. During rewarming, the left subclavian artery was anastomosed. The root repair as well as the proximal aortic anastomosis were completed, and aortic cross-clamp removed. Then, the innominate artery anastomosis was completed. The patient was weaned off the CPB and the hemostasis was achieved. The patient was transferred to the ICU intubated after surgery. All operations were performed by staff surgeons who were specialized in aortic surgery. Chest closures were performed by staffs or clinical associates with expertise in all cases.
Temperature monitoring
All patients were transferred from the emergency department to the ICU upon hospital admission. The tympanic temperature was measured every four hours with ear thermometer (ThermoScan, Barun, Hesse, Germany) prior to the surgery. Both left and right-side temperatures were measured, and the higher one was recorded. The temperature taken right before transferring to the operating room was used to represent the preoperative temperature. During surgery, both the nasopharyngeal and the bladder temperature were monitored continuously. They were measured by nasopharyngeal temperature probe (DeRoyal Industries, Powell, TN, USA) and Foley catheter temperature sensor (Level 1, smiths medical, Dublin, OH, USA), respectively. The nasopharyngeal probe was placed 5 cm from the external nares. The postoperative bladder temperature was monitored continuously after arrival at the ICU.
Study endpoints
The primary endpoint was PH, defined as the bladder temperature <36.0 °C upon ICU admission after surgery. The secondary endpoints included bleeding and operative mortality defined as death in hospital or within 30 days after surgery. The severity of bleeding was represented by chest tube output during the first 24 hours after surgery and the amount of packed red blood cell consumption during the hospital stay.
Data collection and ethics
Data on all preoperative, intraoperative, and postoperative variables were obtained from our cardiovascular surgical database or manually collected from the electronic medical record at Zhongshan Hospital, Fudan University, Shanghai, China. The data were approved for use in research by the Zhongshan Hospital Institutional Review Board (IRB), with patient consent waived. The IRB approved the study protocol in accordance with the principles of the Declaration of Helsinki (as revised in 2013).
Statistical analysis
The Kolmogorov-Smirnov test was applied in normality evaluation. Normally distributed continuous variables were presented as mean ± standard deviation and analyzed by independent t-test. Categorical variables were presented as number and percentage and analyzed by the Chi-square test or Fisher exact test (when appropriate). Preoperative and procedural variables significantly associated with PH in univariable analyses (P<0.05) were included in the final multivariable model to identify the independent risk factors for PH. The P value less than 0.05 was considered significant. The statistical package used was SPSS software (Version 22; IBM Corp., New York, NY).
Results
Demographics and baseline characteristics
A total of 300 patients (age 53.8±11.5 years, female 63, 21.0%) underwent total arch replacement were enrolled in this study. Two hundred and twenty-one patients (73.7%) had systemic hypertension. Twenty-two patients (7.3%) were deemed to have genetic aortic disease according to clinical presentation. One hundred and ten patients (36.7%) had aortic regurgitation >2+, 28 patients (9.3%) had severe aortic regurgitation (4+) secondary to commissure detachment. The mean preoperative temperature was 37.2±0.6 °C. The entire cohort was divided into two groups by the occurrence of PH. There were 44 patients in the PH group and 256 patients in the non-PH group. The patients in the PH group were significantly older than the other group (58.9±8.7 vs. 52.9±11.7 years, P<0.001). Other variables were comparable between the two groups. The details of demographics and baseline characteristics are demonstrated in Table 1.
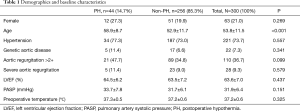
Full table
Procedural outcomes
All patients underwent total arch replacement. Two hundred and nineteen patients (73.0%) had aortic root reinforcement with supracoronary ascending aorta replacement, the ratio was significantly lower in the PH group (52.3% vs. 76.6%, P=0.001). Two hundred and ninety-five patients (98.3%) underwent frozen elephant trunk repair. Fourteen patients (4.7%) underwent CABG after having difficulty in weaning from bypass, which was attributed to compromised coronary ostia reconstruction. The ratio of CABG was significantly higher in the PH group (11.4% vs. 3.5%, P=0.039). Seven patients (2.3%) underwent ascending aorta-iliac artery bypass because of compromised blood flow to the lower limbs, which might be a result of true lumen occlusion or stenosis. Other concomitant surgeries included mitral or tricuspid valve repair, atrial septal defect (ASD) or patent foramen ovale (PFO) repair, aortic root-right atrium shunt and right axillary embolism retrieval. The mean value of the lowest bladder temperature was significantly lower in the PH group (24.6±1.0 vs. 25.5±1.5 °C, P<0.001). No significant difference was reached in the lowest nasopharyngeal and post-CPB temperatures. The details of procedural outcomes are shown in Table 2.
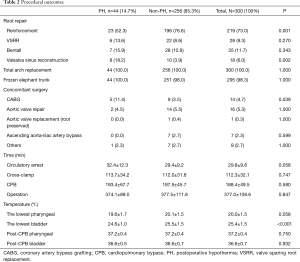
Full table
Postoperative outcomes
The operative mortality and stroke rate were 6.7% (20 patients) and 4.0% (12 patients), respectively. Eight patients (2.7%) underwent venous-venous extracorporeal membrane oxygenation (ECMO) insertion due to refractory severe hypoxia. Fifty-four patients (18.0%) required prolonged ventilation. The mean volume of chest tube output in the first 24-hour was 474.0±339.0 mL. No significant difference was reached in any postoperative outcomes between PH and non-PH groups. The details of postoperative outcomes are shown in Table 3.
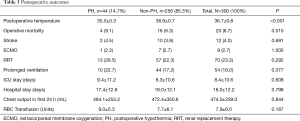
Full table
Multivariate regression analysis of the risk factors of PH
Among the preoperative and procedural variables, age, the ratio of patients underwent reinforcement, Valsalva sinus reconstruction and CABG, the lowest intraoperative bladder temperature were found to be significant different between the PH and non-PH groups. These variables were included into our final multivariate regression model to determine the independent risk factors of PH. Age (odds ratio 1.036, 95% CI: 1.003–1.071) and the intraoperative lowest bladder temperature (odds ratio 0.636, 95% CI: 0.483–0.839) were found to be the independent risk factors of PH. The details of the multivariate regression model are shown in Table 4.
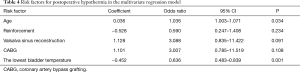
Full table
Discussion
The recognition of PH in the surgical community can be traced back to the early 1980s (2). Since then, PH is deemed to have series of adverse effects in recovery after non-cardiac surgery, which include prolonged mechanical ventilation, bleeding, increased blood products consumption, longer length of stay in the ICU and increased mortality (1,9,10).
Compared to non-cardiac surgery, more concerns need to be taken when study the incidence and effects of PH in on-pump cardiac surgery. The intraoperative deliberate hypothermia may extend into the postoperative period and increase the incidence of PH. On the other hand, active rewarming through CPB can effectively correct the PH, however, the aggressive rewarming may have its intrinsic adverse effect, including cerebral hyperthermia. Controversy exists on the impact of PH on recovery after cardiac surgery. At least transient hypothermia is believed to be non-influential on mortality after cardiac surgery (11). Findings in another study suggest that complete rewarming after hypothermic CPB be not necessary in all cases (12). Conversely, evidence have shown, postoperative hyperthermia is highly associated with adverse outcomes including acute kidney injury and neuronal injury after on-pump cardiac surgery (13,14). Rungatscher and colleagues found that, compared to normothermia, hyperthermia was independently associated with a higher risk of 30-day mortality, stroke incidence, and poor neurologic outcome after DHCA for aortic arch surgery, while no significant differences were demonstrated between hypothermia and normothermia (15).
The occurrence of PH after DHCA for aortic arch surgery is even more complicate. Extended operative time, application of deep hypothermia, large amount of bleeding and blood products and fluid infusion predispose these patients to develop PH. At the same time, the brain ischemia makes patients prone to cerebral complications associated with potential hyperthermia. Unfortunately, previous studies focused on this topic are limited. We found it is necessary to conduct this study to investigate the incidence of PH as well as its impact on early outcomes after aortic arch surgery with DHCA.
The incidence of PH after on-pump cardiac surgery varied in literatures from 28% to 66% (9,11,15). Although, deliberate hypothermia is used in most on-pump cardiac surgery, patients have lower incidence of PH after cardiac surgery as compared to non-cardiac surgery, which may be a result of active systemic rewarming with CPB (16,17). The incidence of PH in our cohort was 14.7%. The relatively lower incidence of PH is contributed to the intraoperative rewarming protocol. We set our target of rewarming at bladder temperature 36.0°C. The gradient between the nasopharyngeal and the bladder temperature during rewarming process is maintained at <3 °C. The temperature gradient between water and blood is typically maintained at <10 °C. Fluid warmer is used when massive cold fluid and blood products infusion are required during rewarming. And we set a higher ambient room temperature at 24 °C to facilitate the rewarming.
The major finding of our present study is that, the independent risk factors of PH are age and the lowest bladder temperature during DHCA.
Older age is proved to be a risk factor of PH in previous publications (1,3), which are consistent with our study. Elderly patients are prone to develop PH due to less efficient temperature regulation and lower basal metabolic rate (18,19). Providers should be aware of this relationship, and pay more attention to elderly population to avoid PH.
Nasopharyngeal temperature monitoring is a satisfactory surrogate of brain temperature during DHCA, surgeons can be confident that the true brain temperature is at or below the nasopharyngeal measurement (20). That is the reason the nasopharyngeal temperature is used in routine practice as a reference to determine the optimal occasion to initiate circulatory arrest. For instance, we set our target nasopharyngeal temperature at 22 °C, although it will continue to decline during the DHCA process. However, it is the bladder temperature which is deemed a reliable index of the core temperature during times of thermal stability (21). Since that, we set our target of rewarming at the bladder temperature 36.0 °C. It is easy to understand the significant relationship between the intraoperative lowest bladder temperature and the incidence of PH.
In addition to this, in univariate analysis, we have found that, patients in PH group had lower opportunity to undergo root reinforcement and higher opportunity to undergo Valsalva sinus reconstruction and CABG. This can be interpreted as positive relationship exists between the surgical complexity and incidence of PH. And, the mean duration of DHCA and the lowest nasopharyngeal temperature were longer and lower in the PH group, which showed a marginal trend toward significance (P=0.058).
As above mentioned, PH has significant adverse effects on recovery after non-cardiac surgery. However, few studies have successfully demonstrated this relationship in cardiac surgery. Only persistent hypothermia (not corrected within 24 hours) is associated with markedly increased risk of death after cardiac surgery (11). In our practice, we use the protocol recommended in guidelines for perioperative care in cardiac surgery to prevent persistent hypothermia, which include using forced-air, warming blankets, raising the ambient room temperature, and warming irrigation and intravenous fluids (22). When we looked closer at our 44 patients with PH, 41 patients (93.2%) were rewarmed to over 36.0 °C within four hours. As a result, no significant difference is demonstrated in early postoperative outcomes in patients with or without PH, which is consistent with previous studies. The result indicates that the influence of transient PH on early outcomes after aortic arch surgery with DHCA, is minimal.
The study has several limitations. Although the technique for total arch replacement in this study was almost uniform, the heterogeneity of the details in technique cannot be eliminated. Also, there were tiny variations in temperature management protocols among cases to cope with different situations. However, the influence of the above issues on the incidence of PH were limited.
Conclusions
The incidence of PH after total arch replacement in acute type A aortic dissection is relatively low. The independent risk factors of PH in this population include age and the intraoperative lowest bladder temperature. With delicate rewarming protocol after arrival at the ICU, the PH is easily corrected, and the adverse effect of transient PH on early outcomes after arch surgery with DHCA is minimal.
Acknowledgments
We thank Dr. Jiali Chen for her knowledge and explanation of the details in the cardiopulmonary bypass technique used in this study.
Funding: This work was supported by National Natural Science Foundation of China Youth Science Foundation Project [81801743].
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-1709
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-1709
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-1709
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-1709). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The data were approved for use in research by the Zhongshan Hospital Institutional Review Board (IRB), with patient consent waived. The IRB approved the study protocol in accordance with the principles of the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Slotman GJ, Jed EH, Burchard KW. Adverse effects of hypothermia in postoperative patients. Am J Surg 1985;149:495-501. [Crossref] [PubMed]
- Vaughan MS, Vaughan RW, Cork RC. Postoperative hypothermia in adults: relationship of age, anesthesia, and shivering to rewarming. Anesth Analg 1981;60:746-51. [Crossref] [PubMed]
- Kleimeyer JP, Harris AHS, Sanford J, et al. Incidence and Risk Factors for Postoperative Hypothermia After Orthopaedic Surgery. J Am Acad Orthop Surg 2018;26:e497-503. [Crossref] [PubMed]
- Chun EH, Lee GY, Kim CH. Postoperative hypothermia in geriatric patients undergoing arthroscopic shoulder surgery. Anesth Pain Med 2019;14:112-6. [Crossref]
- Samoila G, Ford RT, Glasbey JC, et al. The Significance of Hypothermia in Abdominal Aortic Aneurysm Repair. Ann Vasc Surg 2017;38:323-31. [Crossref] [PubMed]
- Ruetzler K, Kurz A. Consequences of perioperative hypothermia. Handb Clin Neurol 2018;157:687-97. [Crossref] [PubMed]
- Kander T, Schott U. Effect of hypothermia on haemostasis and bleeding risk: a narrative review. J Int Med Res 2019;47:3559-68. [Crossref] [PubMed]
- Mason SE, Kinross JM, Hendricks J, et al. Postoperative hypothermia and surgical site infection following peritoneal insufflation with warm, humidified carbon dioxide during laparoscopic colorectal surgery: a cohort study with cost-effectiveness analysis. Surg Endosc 2017;31:1923-9. [Crossref] [PubMed]
- Insler SR, O’Connor MS, Leventhal MJ, et al. Association between postoperative hypothermia and adverse outcome after coronary artery bypass surgery. Ann Thorac Surg 2000;70:175-81. [Crossref] [PubMed]
- Luís C, Moreno C, Silva A, et al. Inadvertent postoperative hypothermia at post-anesthesia care unit: incidence, predictors and outcome. Open J Anesthesiol 2012;2:205-13. [Crossref]
- Karalapillai D, Story D, Hart GK, et al. Postoperative hypothermia and patient outcomes after elective cardiac surgery. Anaesthesia 2011;66:780-4. [Crossref] [PubMed]
- Nathan HJ, Parlea L, Dupuis JY, et al. Safety of deliberate intraoperative and postoperative hypothermia for patients undergoing coronary artery surgery: a randomized trial. J Thorac Cardiovasc Surg 2004;127:1270-5. [Crossref] [PubMed]
- Newland RF, Tully PJ, Baker RA. Hyperthermic perfusion during cardiopulmonary bypass and postoperative temperature are independent predictors of acute kidney injury following cardiac surgery. Perfusion 2013;28:223-31. [Crossref] [PubMed]
- Nussmeier NA. Management of temperature during and after cardiac surgery. Tex Heart Inst J 2005;32:472-6. [PubMed]
- Rungatscher A, Luciani GB, Linardi D, et al. Temperature Variation After Rewarming from Deep Hypothermic Circulatory Arrest Is Associated with Survival and Neurologic Outcome. Ther Hypothermia Temp Manag 2017;7:101-6. [Crossref] [PubMed]
- Karalapillai D, Story D. Hypothermia on arrival in the intensive care unit after surgery. Crit Care Resusc 2008;10:116-9. [PubMed]
- Pezawas T, Rajek A, Plöchl W. Core and skin surface temperature course after normothermic and hypothermic cardiopulmonary bypass and its impact on extubation time. Eur J Anaesthesiol 2007;24:20-5. [Crossref] [PubMed]
- Lee HJ, Kim KS, Jeong JS, et al. The influence of mild hypothermia on reversal of rocuronium-induced deep neuromuscular block with sugammadex. BMC Anesthesiol 2015;15:7. [Crossref] [PubMed]
- Li LR, You C, Chaudhary B. Intraoperative mild hypothermia for postoperative neurological deficits in intracranial aneurysm patients. Cochrane Database Syst Rev 2012.CD008445. [Crossref] [PubMed]
- Kaukuntla H, Harrington D, Bilkoo I, et al. Temperature monitoring during cardiopulmonary bypass--do we undercool or overheat the brain? Eur J Cardiothorac Surg 2004;26:580-5. [Crossref] [PubMed]
- Fallis WM. Monitoring urinary bladder temperature in the intensive care unit: state of the science. Am J Crit Care 2002;11:38-45. [Crossref] [PubMed]
- Engelman DT, Ben Ali W, Williams JB, et al. Guidelines for Perioperative Care in Cardiac Surgery: Enhanced Recovery After Surgery Society Recommendations. JAMA Surg 2019;154:755-66. [Crossref] [PubMed]


