Management of subsolid pulmonary nodules in CT lung cancer screening
Introduction
In view of the prospective results of the National Lung Screening Trial (NLST), and baseline results of other trials, interest in low-dose computed tomography (LDCT) for lung cancer screening in high-risk individuals is increasing. In 2011, the U.S. NLST demonstrated that screening using LDCT reduces lung cancer mortality by 20% compared to screening by chest radiography (1). This result was translated by several U.S. medical associations, including the U.S. Preventive Services Task Force, into a recommendation to screen subjects at high-risk for developing lung cancer by LDCT (2-6). Recently, the American College of Radiology released Lung-RADS, a classification system for LDCT lung cancer screening (7).
In these guidelines, a distinction is made between solid and subsolid nodules. Solid lung nodules are by far the most common type of nodules found at lung cancer screening (8,9). In a small number of participants, a subsolid pulmonary nodule (SSN), defined as a circumscribed area of increased lung attenuation with preservation of the bronchial and vascular margins (10), is detected. An SSN can be classified as a nonsolid, purely ground-glass attenuation (GGN), or as part-solid lesion, containing both solid and ground-glass components. Usually, a SSN is due to inflammation, infection, or fibrosis, but it can also represent adenocarcinoma, most likely non-aggressive adenocarcinoma in situ (11-13).
Although usually not lethal, SSN malignancy rates ranging from 19.7-75% have been published (14,15). Development or increase of a solid component in a SSN greatly increases lung cancer risk. Other important predictors of malignancy include increase in mass, larger nodule size and a larger relative percentage of the solid portion of a part-solid nodule, and the presence of a lobulated border (16-19). Very slow growth rates, with volume-doubling times as long as 813 days, are reported for SSNs (20). The major challenge in the management of SSNs in LDCT lung cancer screening is to timely identify increase in cancer stage, but to avoid overdiagnosis and overtreatment of non-aggressive, indolent lung cancers (21).
The distinct appearance and behavior of SSNs has resulted in separate recommendations for the management of solitary SSNs at initial detection, both for incidentally detected (10) as well as for screen detected nodules (7,22,23), as shown in Table 1. Since these guidelines have been based primarily on consensus/expert opinion, recently two studies were published regarding SSNs detected in LDCT lung cancer screening, including management advices (24,25).
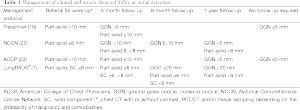
Full table
Results of the studies
Yankelevitz et al. reported the results of nonsolid nodules in the International Early Lung Cancer Action Program (I-ELCAP). In that study, a nonsolid nodule was identified in 2,392 of 57,496 (4.2%) baseline screenings and a new nonsolid nodule in 485 of 64,677 incident screenings (0.7%) (25). Of the 2,877 nonsolid nodules, one third resolved or decreased during follow-up. This happened more frequently in annual repeat rounds than in baseline rounds. Lung cancer diagnosis of a nonsolid nodule was made in 84 participants (73 at baseline), all stage IA adenocarcinoma. All cancer diagnoses were made in growing nodules, and in 22 of 84 cancer cases (26.2%), a solid component appeared in a previously nonsolid nodule. After a median follow-up period since diagnosis of 78 months, the lung cancer survival rate was found to be 100%.
In the different guidelines regarding screen-detected nonsolid nodules, nodule management is based on the diameter of largest nodule, with recommendation of repeat imaging within one year for large nonsolid nodules (7,22,23). However, in the study of Yankelevitz et al., it was found that survival rate did not differ between nodules of different size categories (25). This resulted in the conclusion that screen-detected nonsolid nodules of any size can be safely followed with LDCT at 12-month intervals.
The second study reporting the clinical course of patients with SSNs, by Scholten et al., was published in the European Respiratory Journal. In the Dutch-Belgian randomized lung cancer screening (NELSON) trial, at least one SSN (non-solid or part-solid) was detected in 234 of 7,135 subjects (3.3%) (24). One hundred forty-seven SSNs in 126 participants resolved during follow-up. In total, 69 persistent purely non-solid lesions were detected, of which 20 developed a solid component in follow-up. Median follow-up of all SSNs was 95 months (range, 20-110 months).
In total, 33/126 SSNs (11 nonsolid and 22 part-solid) were resected, including 28 cases of (pre) invasive disease. Of the 11 resected pure nonsolid lesions; six were pre-invasive adenocarcinoma in situ, and four were invasive adenocarcinomas. The remaining nonsolid nodule turned out to be benign. Seven of 20 (35%) nonsolid lesions in which a solid component appeared during follow-up were diagnosed as lung cancer; two adenocarcinoma in situ and five invasive adenocarcinomas. Stage I disease was found for all but one invasive adenocarcinoma (stage IV, due to delayed resection because of a competing malignancy). During follow-up, none of the non-resected SSNs progressed into a clinical relevant malignancy. Scholten et al. (24) concluded that long-term follow-up with CT to monitor changes in persistent SSNs instead of resection may be a safe option in the management of SSNs. They suggest to resect only SSNs that show more than 30% growth or a new appearing or growing solid component.
Most important limitation of both studies was that no histological diagnosis was made for all stable or growing nonsolid nodules. The actual cancer rate, therefore, might be higher. However, after a follow-up time comparable to follow-up of lung cancers, no aggressive lung cancers derived from these nodules.
Conclusions
What are we to conclude from these studies? SSNs are a specific subtype of pulmonary nodules, which, because of their non-aggressive behavior, should be dealt with differently compared to solid nodules. Despite the relatively high risk of malignancy in these nodules, especially in part-solid nodules, progression to cancer stage beyond stage I is very rare. Thus immediate resection of these nodules may mostly be not desirable, and close follow-up of SSNs by annual LDCT usually is sufficient. Implementation of the results of Yankelevitz et al. (25) and Scholten et al. (24) contributes to the optimization of management of screen-detected SSNs, in terms of reduction of overdiagnosis and overtreatment. Future research should point out if biannual follow-up of screen-detected SSNs does not increase overall mortality and morbidity rates.
Acknowledgements
None.
Footnote
Provenance: This is a Guest Editorial commissioned by the Section Editor Lihua Chen [Department of Radiology, Taihu Hospital (PLA 101Hospital), Wuxi, Jiangsu, China].
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [PubMed]
- Detterbeck FC, Mazzone PJ, Naidich DP, et al. Screening for lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e78S-92S.
- Wender R, Fontham ET, Barrera E Jr, et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin 2013;63:107-17. [PubMed]
- Humphrey LL, Deffebach M, Pappas M, et al. Screening for lung cancer with low-dose computed tomography: a systematic review to update the US Preventive services task force recommendation. Ann Intern Med 2013;159:411-20. [PubMed]
- American Lung Association Lung Cancer Screening Committee. Providing Guidance on Lung Cancer Screening to Patients and Physicians. 2012. Available online: http://www.lung.org/lung-disease/lung-cancer/lung-cancer-screening-guidelines/lung-cancer-screening.pdf
- Moyer VA. Screening for Lung Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2014;160:330-8. [PubMed]
- American College of Radiology. Lung CT Screening Reporting and Data System (Lung-RADS). Available online: http://www.acr.org/Quality-Safety/Resources/LungRADS
- van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med 2009;361:2221-9. [PubMed]
- Veronesi G, Bellomi M, Mulshine JL, et al. Lung cancer screening with low-dose computed tomography: a non-invasive diagnostic protocol for baseline lung nodules. Lung Cancer 2008;61:340-9. [PubMed]
- Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 2013;266:304-17. [PubMed]
- Suzuki K, Asamura H, Kusumoto M, et al. "Early" peripheral lung cancer: prognostic significance of ground glass opacity on thin-section computed tomographic scan. Ann Thorac Surg 2002;74:1635-9. [PubMed]
- Aoki T, Nakata H, Watanabe H, et al. Evolution of peripheral lung adenocarcinomas: CT findings correlated with histology and tumor doubling time. AJR Am J Roentgenol 2000;174:763-8. [PubMed]
- Vazquez M, Carter D, Brambilla E, et al. Solitary and multiple resected adenocarcinomas after CT screening for lung cancer: histopathologic features and their prognostic implications. Lung Cancer 2009;64:148-54. [PubMed]
- Oh JY, Kwon SY, Yoon HI, et al. Clinical significance of a solitary ground-glass opacity (GGO) lesion of the lung detected by chest CT. Lung Cancer 2007;55:67-73. [PubMed]
- Park CM, Goo JM, Lee HJ, et al. Nodular ground-glass opacity at thin-section CT: histologic correlation and evaluation of change at follow-up. Radiographics 2007;27:391-408. [PubMed]
- de Hoop B, Gietema H, van de Vorst S, et al. Pulmonary ground-glass nodules: increase in mass as an early indicator of growth. Radiology 2010;255:199-206. [PubMed]
- Nakata M, Saeki H, Takata I, et al. Focal ground-glass opacity detected by low-dose helical CT. Chest 2002;121:1464-7. [PubMed]
- Park CM, Goo JM, Kim TJ, et al. Pulmonary nodular ground-glass opacities in patients with extrapulmonary cancers: what is their clinical significance and how can we determine whether they are malignant or benign lesions? Chest 2008;133:1402-9. [PubMed]
- Lee HJ, Goo JM, Lee CH, et al. Predictive CT findings of malignancy in ground-glass nodules on thin-section chest CT: the effects on radiologist performance. Eur Radiol 2009;19:552-60. [PubMed]
- Hasegawa M, Sone S, Takashima S, et al. Growth rate of small lung cancers detected on mass CT screening. Br J Radiol 2000;73:1252-9. [PubMed]
- Infante M, Berghmans T, Heuvelmans MA, et al. Slow-growing lung cancer as an emerging entity: from screening to clinical management. Eur Respir J 2013;42:1706-22. [PubMed]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Lung Cancer Screening. 2013.
- Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e93S-120S.
- Scholten ET, de Jong PA, de Hoop B, et al. Towards a close computed tomography monitoring approach for screen detected subsolid pulmonary nodules? Eur Respir J 2015;45:765-73. [PubMed]
- Yankelevitz DF, Yip R, Smith JP, et al. CT Screening for Lung Cancer: Nonsolid Nodules in Baseline and Annual Repeat Rounds. Radiology 2015:142554. [Epub ahead of print]. [PubMed]


