
Policy during coronavirus disease 2019 (COVID-19) pandemic: a protector for acute exacerbation of COPD (AECOPD) patients?
The novel coronavirus disease 2019 (COVID-19) was first identified in 2019 (1). COVID-19 is a respiratory and systemic illness that may progress to severe hypoxemia and acute respiratory distress syndrome, which ultimately leads to death. The global number of COVID-19 cases (as June 13, 2020) has reached 7,553,182, which has led to a global economic burden and negative impact on the entire world’s population (2). Although the outbreak of COVID-19 is relatively controlled in China, the risk factor remains.
Chronic obstructive pulmonary disease (COPD) is a common respiratory disease with a prevalence rate of 13.7% (among people over 40 years of age) in China (3). Factors such as genetic predisposition, lung growth, and exposure to particles are associated with the risk and progression of COPD (4). Patients with COPD generally experience exacerbations and hospitalizations during winter months when more respiratory influenza viral infections are prevalent in the community. Outdoor air pollution is also elevated in winter, which is positively associated with COPD-related morbidity and mortality. This is consistent with the epidemic period of COVID-19 in China (from December 2019 to April 2020). Although patients with COPD are not very susceptible to COVID-19 as compared to those with diabetes or hypertension, they have a higher risk of developing severe COVID-19 infection (5).
During this crisis period, the Chinese Thoracic Society (CTS) and the American Thoracic Society (ATS) have published important guidelines to assist pulmonologists on how to manage their COPD patients. Keeping patients on their regular maintenance therapies and home quarantine are the main suggestions. The Chinese Government has ordered all people to stay at home and avoid going out unnecessarily. Simultaneously, all hospitals mandated that every patient needs to be tested of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by qualitative real-time reverse-transcriptase-polymerase-chain-reaction (rRT-PCR) assay before admission. If a patient was diagnosed to have COVID-19, he or she was immediately transferred to the designated hospitals. All kinds of patients with a COVID-19 negative result were admitted in hospitals without any restrictions. We found that the hospitalization rate of patients with acute exacerbation of COPD (AECOPD) started to decrease during the outbreak of COVID-19. Therefore, we planned to investigate the hospitalization rate of patients with AECOPD from January 1 to May 31 in 2017 to 2020. We recorded the numbers of AECOPD patients who were admitted and collected their details from the Department of Respiratory Medicine by the electronic health records (EHRs) system in each hospital. We included all cases with the first diagnosis of AECOPD from the EHRs system. We defined hospitalization rate percent = number of hospitalized COPD patients/total number of hospitalized patients at the same period ×100. A total of 72,661 hospitalized patients including 15,579 patients with AECOPD from 11 hospitals (10 third level and 1 second level) in southern China were enrolled (Table 1). All hospitals were not COVID-designated centers. In 2020, the total hospitalization rate of patients with AECOPD was 24.98% lower than that in the same period in 2017 to 2019 (P<0.001, <0.001, <0.001, respectively). The mean admission rate of patients with AECOPD in 3 years was 27.91% higher than that in 2020 (P<0.001). Compared to that in 2019, the admission rate of patients with AECOPD in 2020 decreased in 8 hospitals (P<0.05), but not in three hospitals (P>0.05).
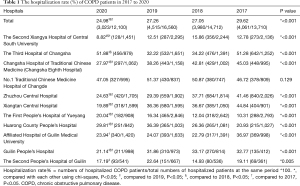
Full table
Some reasons may be attributed to this result. During the COVID-19 period, to prevent virus transmission, the Chinese Government implemented policies to restrict people gathering at functions and parties and made it mandatory to check body temperature daily and to stay at home. All hospitals established regulations to restrict the numbers of patients in both outpatient and inpatient settings to reduce COVID-19 transmission. Most of the patients with COPD had to comply with home quarantine rules, which directly reduced the effect of air pollution and consequently decreased the incidence, prevalence, and mortality due to COPD. In addition, people were recommended to wear a face mask whenever they ventured outside in order to protect them from air pollution and the virus. Thus, not only COVID-19 but also influenza virus infection, which commonly occurs in winter and leads to AECOPD, could be inhibited. In addition, vaccination is an effective method to protect from pneumococcal and influenza virus infection. However, the coverage rate of influenza vaccination in patients with COPD is only 0.9% in the Shanghai region of China (6). One of our studies also found that the vaccination rate in patients with COPD is only 0.3% (7). Therefore, we recommend patients with COPD who have not taken pneumococcal and influenza virus vaccination should wear a face mask when going out doors. Different respirator types have diverse effects on ventilation physiology and respiratory pattern adaptation. Kyung SY and his colleagues recommend the use of filtering facepiece respirator (N95) for mild and moderate COPD patients for protection during outdoor activities under high particulate matter (PM) conditions. Patients with severe COPD with modified Medical Research Council dyspnea scale (mMRC) score >3 or forced expiratory volume in one second % predicted <30% should be very careful when using the N95 mask because of increased risk for inducing hypoxic or hypercapnic respiratory failure (8).
In conclusion, many factors can affect the hospitalization rate of AECOPD patients during the outbreak of COVID-19. Although we cannot definitively state which factor is the main cause, we recommend that patients with COPD should go outdoor less in winter and at the beginning of spring. In addition, people without pneumococcal and influenza virus vaccination should wear a face mask whenever going outside, especially in high PM conditions. More detailed and larger sample size studies on individual management of patients with COPD should be conducted.
Acknowledgments
Thanks to Libing Ma from Affiliated Hospital of Guilin Medical University, Qimi Liu from the Second People’s Hospital of Guilin, Yingqun Zhu from the Third Hospital of Changsha, Ming Chen from No.1 Traditional Chinese Medicine Hospital of Changde, Rong Yi from Zhuzhou Central Hospital, LingMei Huang from the First People’s Hospital of Yueyang, Ying Xiao from Guilin People’s Hospital, Mingyan Jiang from Xiangtan Central Hospital, and Dan Liu from the Changsha Hospital of Traditional Chinese Medicine (Changsha Eighth Hospital) to provide the data.
Funding: This work was supported by the National Key Clinical Specialty Construction Projects; Xiangya Mingyi grant (2013); the National Natural Science Foundation of China (NSFC, 1970044) and NSFC (81770046). Ping Chen provided the funding for this study.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-3342
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-3342). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Reference
- Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395:565-74. [Crossref] [PubMed]
- World Health Organization. Coronavirus disease 2019 (COVID-19). Available online: https://www.who.int/docs/defaultsource/coronaviruse/situation-reports/20200613-covid-19-sitrep-145.pdf?sfvrsn=bb7c1dc9_4. Last Accessed on June 13, 2020.
- Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet 2018;391:1706-17. [Crossref] [PubMed]
- Pérez-Rubio G, Córdoba-Lanús E, Cupertino P, et al. Role of genetic susceptibility in nicotine addiction and chronic obstructive pulmonary disease. Rev Invest Clin 2019;71:36-54. [Crossref] [PubMed]
- Lippi G, Henry BM. Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19). Respir Med 2020;167:105941 [Crossref] [PubMed]
- Wang Y, Cheng M, Wang S, et al. Vaccination coverage with the pneumococcal and influenza vaccine among persons with chronic diseases in Shanghai, China, 2017. BMC Public Health 2020;20:359. [Crossref] [PubMed]
- Zeng Y, Cai S, Chen Y, et al. Current Status of the Treatment of COPD in China: A Multicenter Prospective Observational Study. Int J Chron Obstruct Pulmon Dis 2020;15:3227-37. [Crossref] [PubMed]
- Kyung SY, Kim Y, Hwang H, et al. Risks of N95 Face Mask Use in Subjects With COPD. Respir Care 2020;65:658-64. [Crossref] [PubMed]


