Simultaneous thoracoscopic resection for coexisting pulmonary and thymic lesions
Background
Thymic tumors are potentially associated with synchronous or asynchronous second malignancies, such as primary lung cancer (1,2). Although rarely reported, it is feasible to remove both of synchronous thymoma and lung cancer by simultaneous thoracoscopic operation (3-5). Between August 2008 and November 2013, nine patients underwent simultaneous removal of thymic and pulmonary lesions through single-staged thoracoscopic approach at West China Hospital, Sichuan University. We reviewed the records of these patients to summarize the results of this procedure, as well as its clinical feasibility and patient outcomes. To the best of our knowledge, this is the largest case series of patients who underwent simultaneous thoracoscopic resection of thymic and pulmonary lesions until now. This study aims to retrospectively review our preliminary experience and results of performing simultaneous thoracoscopic resection of coexisting diseases of the lung and thymus.
Materials and methods
Patients
The demographic and clinical characteristics of these patients are listed in Table 1. There were four female and five male patients between 43 and 70 years old (median age, 64 years). Among them, three male patients were current smokers, and the rest were non-smokers. The most common symptom was cough (five patients). One patient had chest pain, and the other three patients were referred to our hospital for accidentally detected pulmonary nodules. None of the patients suffered from myasthenia gravis.
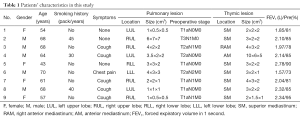
Full table
Preoperative assessment
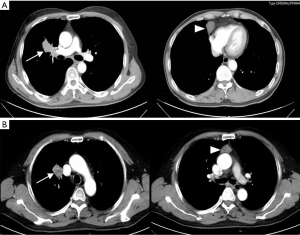
All the patients had chest contrast computed tomography (CT) scan after admission. Each patient had thymic neoplasm combined with solitary pulmonary lesion on chest CT scan (Figure 1). Both of the pulmonary and thymic neoplasms were carefully evaluated by the multidisciplinary group including thoracic surgeons, radiologists and oncologists. On chest CT scan, the pulmonary lesions were 1-7 cm (median, 3 cm) in maximum diameter, including one case of ground-glass opacity, three cases of pulmonary mass and five cases of solitary pulmonary solid nodule. Thymic lesions were 2-5 cm (median, 3 cm) in maximum diameter. Two patients with hilum neoplasm were diagnosed as non-small cell lung cancer (NSCLC) via bronchoscopic biopsy, including one case of lung cancer involving the both the bronchus and main pulmonary artery. The other patients were failed to confirm the diagnosis of pulmonary lesions before surgery. All the patients received abdominal CT scan, brain CT/magnetic resonance imaging scan, and single photon emission CT scan of the bone, to exclude distant metastasis. Preoperative assessment also included electrocardiogram, pulmonary function tests, blood cell count and biochemical tests to evaluate the patients’ status to tolerate the operation. The eligibility to carry out simultaneous thoracoscopic resection of both the lesions was decided according to: (I) general condition to tolerate the operation; (II) technically feasible to remove both neoplasms via the same incision. Patients were excluded from the operation if they had a history of ipsilateral thoracotomy or pleuritis. Informed consent of the operation was obtained from all the patients before surgery. Retrospective review of the medical records was approved by the Institutional Review Board (IRB) of West China Hospital.
Surgical procedures
The operations were carried out under general anesthesia with single lung ventilation. In patients with confirmed lung cancer or other lesions requiring lobectomy, lateral decubitus position was applied. The surgeon stood in the ventral side of the patient to perform lobectomy first. Three ports were made, including a 1-cm thoracoscopic port in the 7th intercostal space (ICS) on the mid-axillary line, a 3-cm incision on the anterior axillary line in the 3rd ICS for upper lobectomy and in the 4th ICS for lower lobectomy, a 2-cm incision in the 9th ICS between the posterior axillary line and scapular line. We usually perform the single-direction thoracoscopic lobectomy that started at the most superficial structures in the root of the hilus after raising the lung, and proceeded gradually without the necessity for repeated turnover of the pulmonary lobes. In the meantime, it can overcome the difficulty in manipulation of the hypoplastic lung fissure (6). Then the surgical table was adjusted to change the patient into the 30° semi-lateral decubitus position. The surgeon moved to the dorsal side to perform thoracoscopic thymectomy/thymic cyst resection (TCR).
For these patients with solitary peripheral pulmonary nodules, when wedge resection was indicated according to preoperative assessment, semi-lateral decubitus position was applied directly. Routine thoracoscopic thymectomy approach was applied, including a 1-cm thoracoscopic port on middle axillary line in the 6th ICS, two 2-cm incisions on the anterior axillary line in the 3rd and 6th ICS, respectively. The surgeon stood on the dorsal side of the patient when performing the operation. Pulmonary wedge resection was carried out first, followed by thoracoscopic thymectomy/TCR. The diagnosis of all the lesions was confirmed by intraoperative frozen section.
Results
Four patients underwent thoracoscopic lobectomy and thymectomy. One of the patients with central NSCLC involving both the bronchus and main pulmonary artery underwent thoracoscopic bronchovascular sleeve lobectomy combined with TCR. The other four patients received wedge resection of the pulmonary nodules and thymectomy (n=3)/TCR (n=1). The operation lasted from 35-480 min (median, 110 min). Intra-operative blood loss ranged from 20-380 mL (median, 120 mL). No blood transfusion was needed. There was no conversion to thoracotomy.
The patients stayed in the intensive care unit (ICU) for the first 12 h after surgery and were transferred to the general ward then. Two patients developed post-operative pneumonia without mortality. These patients were discharged home within 9 days (median, 5 days) after the operation. All the patients were followed up regularly during a period of 6 to 41 months (median, 18 months). Two of them died from metastatic lung cancer 14 months after surgery. The other patients are alive without recurrence or metastasis currently. Detailed information of the operation and follow-up are listed in Table 2.
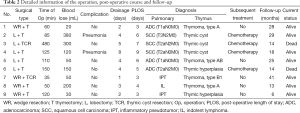
Full table
Discussion
A few patients may suffer from synchronous thymic and pulmonary lesions. However, the management of this problem remains a challenge due to the lack of case series and surgical guidelines. Both the thymus and the lungs lie in anatomically adjacent compartments, and this makes a simultaneous resection of the lesions arising from these two sites technically feasible (3,4,6). The operation can be successfully carried out through thoracotomy or the thoracoscopic approach. In the past decade, video-assisted thoracoscopic surgery (VATS) has become a mature technique for the resection of both thymic and pulmonary diseases. There is mounting evidence suggesting that this new technique is superior to open thoracotomy in many aspects, like shorter hospital stay and duration of pleural drainage with similar or even improved oncological results (7-11). In light of these advantages, we prefer to choose the mini-invasive approach for patients with thymic or pulmonary lesions when surgical intervention is required, even for patients with synchronous diseases. Herein, we try to summarize our preliminary experience and results of the simultaneous thoracoscopic operation for this group of patients.
Thymoma has been found to be associated with an increased risk of synchronous or asynchronous malignancy, including lung cancer (1,2). The histologic diagnosis of the pulmonary lesions in our case series finally identified three cases of adenocarcinoma, three cases of squamous cell carcinoma and one case of indolent lymphoma. Only two cases were confirmed as benign pulmonary lesions. Among the seven patients with lung malignancies, four had thymic cyst, two had thymoma, and the other patient was diagnosed as thymic hyperplasia. Whether thymic cyst is associated with lung cancer is unknown. However, these results prompt us pay attention to this group of patients. In patients with pulmonary nodules and thymic abnormalities, no matter thymoma, thymic cyst or hyperplasia, the presence of synchronous lung cancer should be taken into account when making treatment decisions.
Surgery is the most preferred and effective treatment option for patients with thymic tumor (12). All the patients with thymic tumors should undergo en bloc resection of the tumor if there were no surgical or oncological contraindications. Surgical resection also provides the best chance to cure patients with NSCLC. Based on this, we considered surgery as a reasonable choice for patients with synchronous thymic and pulmonary neoplasm. The decision to perform simultaneous thoracoscopic resection of the two lesions was made after carefully assessing chest CT scan and patient’s general status. In most cases, thoracoscopic thymectomy can be accomplished through both the left and the right thoracic approach. As such, the location of the pulmonary lesion became a decisive factor for the choice of surgical approach. The operations were carried out on the ipsilateral side of the pulmonary lesions.
Another problem should be considered is the setup of surgical ports. The same as many centers, we apply different incisions for thoracoscopic lobectomy and thymectomy. Thymectomy is usually carried out with the patient placed in the semi-decubitus position to ease the operation while a lateral decubitus position is better for lung surgery. In addition, when performing VATS lung surgery, the distance between each port is longer than that for thymectomy. The ports of thoracoscopic thymectomy are all placed on the anterolateral chest wall. Therefore, a careful consideration upon the surgical approach is required for patients with concomitant pulmonary and thymic diseases before surgery. For this group of patients, the incisions were mainly decided according to the complexity of the surgical procedure. If a lobectomy was planned before surgery, we applied the ports of routine pulmonary resection. When pulmonary wedge resection was foreseen upon preoperative assessment, thymic incision was adopted. Pulmonary resection was carried out first in every patient, followed by intraoperative frozen section to confirm the diagnosis. The position of the patient was changed when performing different operations to get better exposure, so did the position of the surgeons.
The safety of the operation is always the primary concern. However, for the lack of clinical data, the application of simultaneous thoracoscopic operation for patients with synchronous pulmonary and thymic diseases remains undetermined. None of our patients suffered from severe operative complications, and no conversion to thoracotomy was required. Two patients had postoperative pneumonia without mortality. Both of the reported cases in the literature also had uneventful recovery after a simultaneous thoracoscopic operation (3,4). Additionally, this procedure may save the medical costs for these patients for both of the lesions were removed during a single-staged surgical procedure. However, a further comparative study is needed to confirm the advantages of this procedure.
Conclusions
In summary, although the management of coexisting thymic and pulmonary lesions occuring in a patient remains a challenge due to the lack surgical guidelines, our preliminary data show that simultaneous thoracoscopic resection of pulmonary and thymic lesions is safe and feasible for carefully selected patients. The decision of choosing an ideal surgical approach based on preoperative assessment is essential to ensure the safety of the operation.
Acknowledgements
The authors greatly appreciate the assistance of the staff of the Department of Thoracic Surgery, West China Hospital, Sichuan University, China, and thank them for their efforts.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Pan CC, Chen PC, Wang LS, et al. Thymoma is associated with an increased risk of second malignancy. Cancer 2001;92:2406-11. [PubMed]
- Welsh JS, Wilkins KB, Green R, et al. Association between thymoma and second neoplasms. JAMA 2000;283:1142-3. [PubMed]
- Xie D, Xie H, Zhu Y, et al. Simultaneous video-assisted thoracoscopic surgery sleeve lobectomy and thymectomy. Interact Cardiovasc Thorac Surg 2014;19:313-4. [PubMed]
- Dolci G, Dell'Amore A, Asadi N, et al. Synchronous thymoma and lung adenocarcinoma treated with a single mini-invasive approach. Heart Lung Circ 2015;24:e11-3. [PubMed]
- Patella M, Anile M, Vitolo D, et al. Synchronous B3 thymoma and lung bronchoalveolar carcinoma. Interact Cardiovasc Thorac Surg 2011;12:75-6. [PubMed]
- Liu L, Che G, Pu Q, et al. A new concept of endoscopic lung cancer resection: Single-direction thoracoscopic lobectomy. Surg Oncol 2010;19:e71-7. [PubMed]
- Cao C, Manganas C, Ang SC, et al. Video-assisted thoracic surgery versus open thoracotomy for non-small cell lung cancer: a meta-analysis of propensity score-matched patients. Interact Cardiovasc Thorac Surg 2013;16:244-9. [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [PubMed]
- Lee PC, Nasar A, Port JL, et al. Long-term survival after lobectomy for non-small cell lung cancer by video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg 2013;96:951-60; discussion 960-1. [PubMed]
- Maniscalco P, Tamburini N, Quarantotto F, et al. Long-term outcome for early stage thymoma: comparison between thoracoscopic and open approaches. Thorac Cardiovasc Surg 2015;63:201-5. [PubMed]
- Liu TJ, Lin MW, Hsieh MS, et al. Video-assisted thoracoscopic surgical thymectomy to treat early thymoma: a comparison with the conventional transsternal approach. Ann Surg Oncol 2014;21:322-8. [PubMed]
- Benveniste MF, Korst RJ, Rajan A, et al. A practical guide from the International Thymic Malignancy Interest Group (ITMIG) regarding the radiographic assessment of treatment response of thymic epithelial tumors using modified RECIST criteria. J Thorac Oncol 2014;9:S119-24. [PubMed]


