Dynamic obstruction induced by systolic anterior motion of the mitral valve in a volume-depleted left ventricle: an unexpected cause of acute heart failure in a patient with chronic obstructive pulmonary disease
Introduction
Left ventricular outflow tract (LVOT) dynamic obstruction (DO) resulting from systolic anterior motion (SAM) of the mitral valve (MV) is a typical feature of hypertrophic cardiomyopathy. However, this intriguing phenomenon can appear even in an apparently normal or near-normal heart under certain clinical conditions associated with hyperdynamic left ventricular (LV) contraction and/or LV volume depletion (1,2). In critically ill patients, the occurrence of LVOT DO caused by SAM of the MV is potentially serious, because it can significantly compromise cardiac output (2). Therefore, a clear understanding of intracardiac hemodynamics and early recognition of interplay between the MV and accelerated LVOT blood flow are of paramount importance.
Because of increased pulmonary vascular resistance, chronic obstructive pulmonary disease (COPD) can impair LV filling; and thus, a decrease in LV volume can occur even before the development of overt cor pulmonale (3). Here, we report a case of transient acute heart failure caused by LVOT DO resulting from SAM of the MV in a severely volume-depleted LV in a patient who suffered from acute exacerbation of COPD. In addition, a diagnostic process with echocardiography, which played a unique role in explaining complex cardiac functional issues, and a patient-specific consideration for proper management will be discussed.
Case report
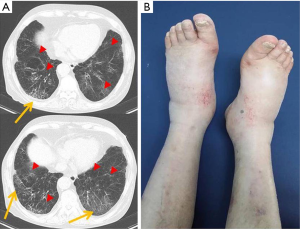
A 72-year-old Asian male with a prior history of COPD and emphysema presented at our emergency department complaining of recently aggravated shortness of breath and purulent sputum. On physical examination, tachycardia (heart rate: 110 beats/minute) and tachypnea (respiratory rate: 24 breaths/minute) were notable. The patient was agitated and showed cold, clammy skin, sweating, external jugular venous distension, and peripheral pitting edema (Figure 1). On auscultation, coarse breath sounds with rales were audible in both lower lung fields, and unexpectedly, systolic murmur (grade IV/VI) was prominent at the left sternal border. Twelve-lead electrocardiography showed sinus tachycardia and non-specific ST-segment/T-wave changes. Chest computed tomography depicted newly developed multifocal ground grass opacity in both lungs, suggesting pneumonia superimposed on preexisting extensive emphysema (Figure 1). Laboratory findings revealed hyponatremia (121 mEq/L) and elevated pro-brain natriuretic peptide (pro-BNP) level (2,515 pg/mL). Blood urea nitrogen was 28 mg/dL, serum creatinine was 1.6 mg/dL, serum protein was 7.4 g/dL, and serum albumin was 4.3 g/dL. Leukocytosis (white blood cells: 23,140/mm3, segment neutrophils: 93%) and elevated high sensitivity C-reactive protein (15.2 mg/dL) were also reported. Arterial blood gas analysis revealed respiratory alkalosis (pH: 7.49, PaCO2: 21 mmHg, PaO2: 76 mmHg, HCO3: 21, SaO2: 96%), which was apparently associated with tachypnea.
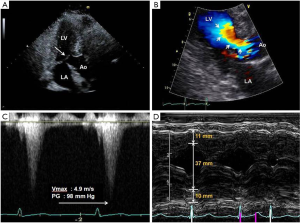
Transthoracic echocardiography was performed to evaluate the nature of the systolic murmur, and the results showed a small LV cavity (LV end-diastolic dimension, 37 mm) with vigorous LV contraction (LV ejection fraction, 80%) suggesting LV volume depletion and a hyperdynamic heart (Figure 2). The right ventricle was not dilated and there was no evidence of overt cor pulmonale. Most notably, SAM of the MV was observed and flow acceleration across the LVOT by color Doppler with a late-peaking flow profile by continuous Doppler was remarkable, all of which indicated LVOT DO (Figure 2).
Under a diagnosis of acute exacerbation of COPD due to pneumonia, oxygen therapy was started to relieve breathlessness and to reduce agitation, and an oral antibiotic (levofloxacin 500 mg daily) was prescribed. Tailored management of the coexisting acute heart failure resulting from LVOT DO was given to patient with specific consideration, and a cardio-selective beta-blocker (bisoprolol 5 mg daily) and intravenous crystalloid were administered to improve hyperdynamic LV contraction and left-heart oligemia, respectively. Two days after initiating treatments, major symptoms showed dramatic improvements and the systolic murmur was no longer audible. In follow-up echocardiography conducted after the initial treatment, SAM of the MV had completely disappeared and low velocity laminar LVOT blood flow was observed, suggesting that the LVOT DO had fully resolved (Figure 3). Laboratory findings supported this improvement; pro-BNP level had dropped to 369 pg/mL and plasma sodium level increased to 139 mEq/L.
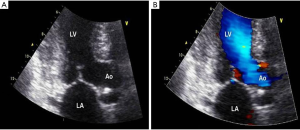
After 3 days of initial treatment targeting left-heart failure, intravenous hydration was stopped and diuretics (torsemide 10 mg daily) were prescribed to address the peripheral edema resulting from right-heart failure associated with COPD. However, two days later, dyspnea showed temporary deterioration, and an echocardiographic assessment revealed reappearance of SAM of the MV and LVOT DO. In addition, at this time plasma pro-BNP had increased to 620 pg/mL. Hence, the diuretic was discontinued and the patient was encouraged to maintain careful oral hydration. After several days of treatment, the patient was restabilized, the pneumonia superimposed on COPD improved, and the acute heart failure resulting from LVOT DO induced by LV volume depletion subsided. The patient was discharged on beta-blocker.
Discussion
Our patient had a unique presentation in that: (I) acute exacerbation of COPD was accompanied by transient acute heart failure; (II) the heart failure was induced by LVOT DO resulting from SAM of the MV in an apparently normal heart; and (III) left-heart volume decrement, resulting from LV filling impairment due to severe lung disease, generated the LVOT DO. This case provides a valuable experience regarding the treatment of patients with COPD who showed changes in intracardiac volume distribution and alterations in cardiac performance. From that perspective, timely performed echocardiographic evaluations were invaluable for accurate diagnosis of the unexpected left-heart problem, which might have contributed to the patient’s dyspnea, and provided us with helpful insight for better understanding of the patient’s clinical course in which we practiced a patient-specific management.
Barr et al. (3) conducted a population-based study using cardiac magnetic resonance imaging, and reported that emphysema was associated with smaller LV volume in the setting of COPD in the absence of clinical cardiovascular disease. Proposed mechanisms for this observation included loss of pulmonary vascular capacity resulting from parenchymal destruction, ventricular interdependence, hypoxic pulmonary arterial vasoconstriction, and pulmonary hyperinflation resulting in elevated intrathoracic pressure exceeding venous pressure (3). Our patient suffered from acute exacerbation of COPD, which might have caused a considerable increase in pulmonary vascular resistance, impaired LV filling, and eventually led to LV volume reduction. Sequentially, SAM of the MV and concomitant LVOT DO occurred in a volume-depleted but structurally normal LV. As was further evidenced by an elevated pro-BNP level, these phenomena caused transient acute heart failure superimposed on COPD in our patient. In fact, these events can occur in a structurally normal heart in association with severe dehydration, massive bleeding, catecholamine usage, sepsis, etc., which can induce hyperdynamic cardiac performance and changes in LV loading conditions (1,2).
Along with conventional management for COPD and pneumonia, we initiated tailored treatment for the unusual cardiac functional abnormality. After the administration of beta-blocker and careful hydration to relieve SAM of the MV, symptoms showed dramatic improvements, in particular, LVOT DO was absent, and notably, pro-BNP levels concomitantly decreased. More interestingly, when we prescribed diuretics to manage peripheral edema, breathlessness was temporarily aggravated, SAM of the MV reappeared and pro-BNP level re-increased. Plasma pro-BNP levels increase during volume- and/or pressure-overload of the heart (4). Briguori et al. (5) reported an association between LVOT pressure gradients and BNP plasma levels in hypertrophic cardiomyopathy patients, and added elevated LV systolic wall stress induced by LVOT DO appeared to be the principal stimulus for the secretion of the natriuretic peptide. Although the question as to whether BNP level is correlated with LVOT DO in subjects free from hypertrophic cardiomyopathy remains to be answered, the suggestions made by Briguori et al., could explain trends in plasma natriuretic peptide levels observed in our patient.
Acknowledgements
Funding: This work was supported by research grants from Gachon University Gil Medical Center, Republic of Korea (Grant number: 2013-10 and 2013-46, J.M.) and Boryung Pharmaceutical Company (J.M.).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chockalingam A, Tejwani L, Aggarwal K, et al. Dynamic left ventricular outflow tract obstruction in acute myocardial infarction with shock: cause, effect, and coincidence. Circulation 2007;116:e110-3. [PubMed]
- Kruppa J, You EJ, Suh SY, et al. Cardiogenic shock induced by basal septal hypertrophy and left ventricular outflow tract dynamic obstruction in a critically ill patient with sepsis. Int J Cardiol 2012;156:338-40. [PubMed]
- Barr RG, Bluemke DA, Ahmed FS, et al. Percent emphysema, airflow obstruction, and impaired left ventricular filling. N Engl J Med 2010;362:217-27. [PubMed]
- Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol 2007;50:2357-68. [PubMed]
- Briguori C, Betocchi S, Manganelli F, et al. Determinants and clinical significance of natriuretic peptides and hypertrophic cardiomyopathy. Eur Heart J 2001;22:1328-36. [PubMed]


