Endobronchial valve to treat large bulla at right middle lobe in chronic obstructive pulmonary disease patients
The large bulla is a complication of chronic obstructive pulmonary disease (COPD) that has been shown to have detrimental effects on lung function of COPD patients, such as decreased forced expiratory volume in 1 s (FEV1), increased total lung capacity (TLC) and functional residual capacity (FRC), and a reduction of diffusing capacity of the lung for carbon monoxide (DLCO) (1,2). Recently, in a prospective, non-randomised and single centre study, endobronchial treatment with one-way valve [Endobronchial valve (EBV), Zephyr®, Pulmonx, Inc., Palo Alto, Calif., USA] was showed to be a safe and effective alternative to treat severe bullous emphysema (3). However, in our previous case series of five COPD patients with bulla, only one had a right middle lobe (RML) bulla which showed sustained improvement in lung function up to six months after EBV treatment (4). To test the effectiveness of EBV to treat large RML bulla, we now present the clinical datum of three COPD patients with large RML bulla, who were treated using EBVs.
Clinical summaries
Patient 1
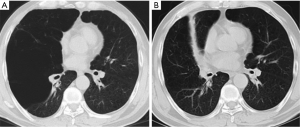
A 52-year-old male, who has a 35-pack-year smoking history, was presented to our respiratory department with worsening dyspnea for 5 years. He has compromised pulmonary function while FEV1 was 1.07 L (35.4% predicted) and residual volume (RV) was 5.37 L (215.8% predicted). The chest computed tomography (CT) revealed a large RML bulla and complete left major and minor fissure. One EBV (size 5.5 mm) was inserted in the RML bronchus. One month and 6 months after the treatment, the lung function tests showed that FEV1 improved to 1.27 L (38.9% predicted) and 1.75 L (57.7%), respectively. Chest CT revealed disappearance of the bulla and atelectasis of RML 6 months after EBV deployment (Figure 1).
Patient 2
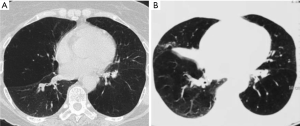
A 66-year-old female consulted at the COPD clinic because of shortness of breath with exertion for 6 years. She is an ex-smoker with a 20-pack-year smoking history. Her severe airflow limitation was manifested by reduced FEV1 (0.71 L, 38.3% predicted). CT of chest showed a large bulla and severe destruction of lung tissue associated with emphysema in RML. Airways leading to the RML were occluded using one valve (size 4.0 mm). At follow-up visits, lung function test revealed FEV1 rose to 1.01 L (54.0% predicted) 1 month after EBV treatment to 1.03 L (55.2% predicted) 6 months after EBV treatment. Chest CT showed disappearance of the bulla and atelectasis of RML (Figure 2).
Patient 3
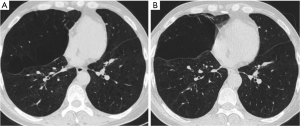
A 50-year-old male smoker was evaluated for chronic shortness of breath. He was diagnosed of COPD 15 years before, and in the last 2 years he has been hospitalized for 3 times to receive treatment for acute exacerbation of chronic obstructive pulmonary disease (AECOPD) and respiratory failure. Before the admission, FEV1 was 0.74 L (19.7% predicted). CT scan showed a large bulla at the position of RML. One valve was placed in RML attempting to close the bulla. The FEV1 has no significant alteration after EBV implantation, with FEV1 0.77 L (20.3%, predicted) and 0.83 L (21.9%, predicted), at 1 month and 6 months after EBV treatment, respectively. The volume of the bulla didn’t change (Figure 3).
Discussion
To our knowledge, this is the first report of usage of EBV to treat large RML bulla, although there were several studies of EBV treatment of bulla in COPD patients (3,5,6). In this study, the improvement of lung function was significant on two patients, whose lung parenchyma was preserved well in lobes other than RML. At the same time, right major and minor fissures were intact on these two patients, which were evidenced by the RML atelectasis after EBV treatment. On the third patient, whose lung function did not show improvement after EBV treatment, the parenchyma of bilateral lungs was destructed heavily by chronic inflammation of COPD, and the bulla of RML did not collapse because right major and/or minor fissures are incomplete.
As illustrated by the first two cases, the isolated large bulla of RML can exist when rest part of lung parenchyma conserved well. This imbalance of lung destruction between RML and rest part of the lung could be explained by the anatomy of right middle bronchus and pathophysiology of COPD: for the right middle bronchus is slimmer and longer than other bronchus, it may experience narrowing even partial collapse at the expiration, meaning that small air trap may exist in the RML. As a consequence, bulla developed in the RML with long-term air trap.
It is obvious that this study has several limitations. Firstly, the patient population is too small to make definite conclusion whether EBV is efficient to treat large RML bulla. Secondly, more detailed clinical data, such as exercise capacity [e.g., 6 minutes walking test (6MWT)] and quality of life [e.g., COPD assessment test (CAT) or ST-George Respiratory Questionnaire (SGRQ)], are of absence in this study.
In conclusion, EBV may be used to treat large RML bulla in selected patients, whose parenchyma of other parts of the lung was conserved well and right major and minor fissures are complete.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wade JF 3rd, Mortenson R, Irvin CG. Physiologic evaluation of bullous emphysema. Chest 1991;100:1151-4. [PubMed]
- Nickoladze GD. Functional results of surgery for bullous emphysema. Chest 1992;101:119-22. [PubMed]
- Santini M, Fiorelli A, Vicidomini G, et al. Endobronchial treatment of giant emphysematous bullae with one-way valves: a new approach for surgically unfit patients. Eur J Cardiothorac Surg 2011;40:1425-31. [PubMed]
- Tian Q, An Y, Xiao BB, et al. Treatment of giant emphysamous bulla with endobronchial valves in patients with chronic obstructive pulmonary disease: a case series. J Thorac Dis 2014;6:1674-80. [PubMed]
- Noppen M, Tellings JC, Dekeukeleire T, et al. Successful treatment of a giant emphysematous bulla by bronchoscopic placement of endobronchial valves. Chest 2006;130:1563-5. [PubMed]
- Santini M, Fiorello A, Di Crescenzo VG, et al. Use of unidirectional endobronchial valves for the treatment of giant emphysematous bulla. J Thorac Cardiovasc Surg 2010;139:224-6. [PubMed]


