Analysis of pulmonary function test results in a health check-up population
Introduction
The morbidity and mortality of chronic obstructive pulmonary disease (COPD) have constantly increased along with the environmental pollution due to extensive and rapid economic development in China and with the increase of smoking rate, imposing serious threats to public health (1-4). However, few epidemiological studies on COPD have been carried out in China (5). In health check-up populations, subjects with the clinical features and/or risk factors of COPD and those who have obstructive ventilator dysfunction and/or obstructive small airway disease but have not reached the diagnostic criteria of COPD are more common (6,7). In our current study, we carried out a research on the incidences and risk factors of COPD and it relevant lung function changes in this population, with an attempt to inform the early prevention and treatment of COPD.
Subjects and methods
Subjects
Subjects who aged 20 years and older and received health check-up in the Health Management Center, Third Xiangya Hospital, Central South University from June 2013 to June 2015 were enrolled in this study. Subjects who did not cooperate in lung function test or those who had other conditions (e.g., bronchiectasis, pulmonary tuberculosis, lung cancer, and congestive heart failure) that might affect the results of lung function test were excluded. Finally 6,811 subjects (5,438 men and 1,373 women) were enrolled. The male-to-female ratio was 4.0:1. The subjects aged 20-79 years (mean: 44.4±9.2 years).
Survey methods
Questionnaire-based survey
A uniform questionnaire was designed and applied. The main items included the general data, previous disease history, medication history, allergy history, family history, lifestyle habits (smoking status). Specially trained doctors were assigned as the survey interviewers.
Physical examination
The subjects’ body weight and height were recorded, and the body mass index (BMI) was calculated [BMI = body weight (kg)/body height (m2)].
Pulmonary function test
The test was uniformly performed using Medikro SpiroStar device in strict accordance with the American Thoracic Society (ATS) quality control standards. During the lung function test, the forced vital capacity (FVC) and the forced expiratory volume in 1.0 s (FEV1) were measured 3 times, and the maximum values were used; furthermore, the differences between maximum and minimum values were smaller than 5% or 150 mL. All the staff involved in lung function test were qualified professionals who had received special training.
Diagnostic criteria
Diagnostic criteria of COPD
FEV1/FVC decreases (below 70% of the predicted normal value) after bronchodilator test (inhalation of salbutamol 200 µg for at least 15 min).
Diagnostic criteria of obstructive ventilator dysfunction
FEV1/FVC decreases (below 90% of predicted) along with the decrease of max voluntary ventilation (MVV) or FEV1 (below 80% of predicted).
Diagnostic criteria of obstructive small airway disease
Two of three criteria including maximal mid-expiratory flow curve (MMEF), forced expiratory flow at 50% of FVC (FEF 50%), and forced expiratory flow at 75% of FVC (FEF 75%) are below 65% of predicted.
Criteria of the risk factors of COPD
Lower respiratory tract infections during childhood
Any of the following respiratory diseases before 14 years is regarded as lower respiratory tract infections during childhood: measles, bronchitis, pneumonia, and whooping cough.
Occupational exposure
A work experience in a workplace (e.g., mining or quarrying, cement, grain processing, casting, textile, paint, and chemical industry) that requires the subjects to be exposed to dust or harmful gases is regarded as occupational exposure.
Bioaerosol exposure
Use of bioaerosols (e.g., wood, grass, and straw) in home cooking in the past decade.
Family history of COPD
The first-degree relative(s) of the subject had a history of COPD.
Among these four items, the positive result(s) of one or more items are defined as the presence of COPD risk factor.
Statistical analysis
The data were collected and then entered by double data entry in Epidata 3.1 software by specially assigned personnel before logic error checking and consistency checking. Statistical analysis was performed using the SPSS 17.0 software, and a value of P<0.05 was considered statistically significant.
Results
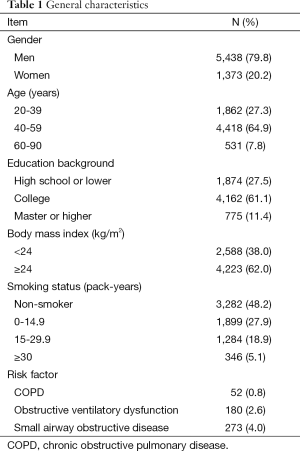
A total of 6,811 subjects [5,438 men (79.8%) and 1,373 women (20.2%)] were enrolled in this study. The detection rate of COPD, obstructive ventilatory dysfunction, and obstructive small airway disease was 0.8%, 2.6%, and 4.0% in this population (Table 1).
Full table
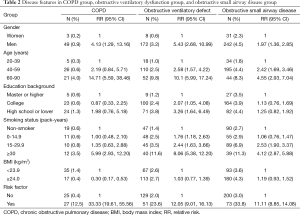
In this health check-up population, the disease features differed among these three groups in terms of gender, age, education background, smoking status, BMI, and risk factors (Table 2). Male subjects with older age (range, 60-79), smoking index ≥30 pack-years, and presence of risk factor had higher risk for COPD; male subjects with an age of 40-60, an education background of college or lower, smoking history, presence of risk factors had higher risk for obstructive ventilatory dysfunction; and male subjects with an age of 40-60 years, smoking index ≥15 pack-years, and presence of risk factor had higher risk for obstructive small airway disease.
Full table
Discussion
COPD, featured by the incomplete reversibility of airflow obstruction, is a progressive pulmonary disease. It has certain association with the lung’s abnormal inflammatory response to harmful gas or particles such as tobacco smoke. In patients with end-stage COPD, the treatment becomes less effective and each acute exacerbation can be potentially life-threatening. The past decades have witnessed the constant increase of COPD morbidity and mortality (8). Globally, the COPD case-fatality has risen from fourth place in 2000 to third place in 2012 (9). In addition, COPD and its complications have dramatically increased the medical costs (10). The heavy burden of COPD has made it an important public health problem.
Early detection and early intervention are key strategies in lowering the incidence of COPD, improving its prognosis, and thus decreasing the burdens of patients, families, and society and improving the patients’ quality of life. Patients may have no or few symptoms at the early stage of COPD, or the mild symptoms are often regarded as the natural manifestations of aging. However, testing for lung function may reveal specific changes, and prompt intervention at this stage can control this condition before it become irreversible. Therefore, routine lung function test and enhanced epidemiological studies on COPD will be particularly helpful for the prevention and treatment of COPD.
In the current study, the detection rate of COPD, obstructive ventilatory dysfunction, and obstructive small airway disease was 0.8%, 2.6%, and 4.0%, respectively in a health check-up population. Globally, the population characteristics, investigation methods, and COPD definitions were different among different epidemiological studies on COPD. For instance, the clinical symptoms, signs, and lung function test results may be separately used as the basis for judging COPD in different studies. Furthermore, the diagnostic criteria of COPD also differ among ATS, British Thoracic Society (BTS), European Respiratory Society (ERS), and Global Initiative for COPD. As a result, the global COPD incidences dramatically differs from 0.2% in Japan to 37% in the United States (11,12). In China, the incidence of COPD also ranged from 5% to 13% in different areas (13). The lower incidence of COPD in our population may be due to the following reasons: (I) most of our subjects are young or mid-aged adults, with a low proportion of elderly people. Since the incidence of COPD increases along with age, the incidence of COPD was thus lower in our population; (II) most of our subjects were white-collar workers who had good economic status and had lower chances to be exposed to biofuels, occupational dust, and the risk of childhood lower respiratory tract infection; (III) the health check-up populations are often composed of healthy and sub-healthy individuals or patients with well-controlled chronic diseases. Patients with severe diseases or requiring repeated outpatient treatment or admission (e.g., patients with advanced COPD) often do not require routine health check-up. Notably, in our current population, the overall incidence of obstructive ventilatory dysfunction and obstructive small airway disease reached 6.6%; disease may progress to COPD if the changeable risk factors (e.g., smoking) are not interrupted timely. Therefore, timely identification of these individuals and early intervention are particularly valuable.
The detection rates of COPD, obstructive ventilatory dysfunction, and obstructive small airway disease were higher in men than in women. Epidemiological studies have shown that the detection rate of COPD is higher in men than in women due to smoking. In recent years, however, the morbidity and mortality of COPD in females have increased annually due to changes in gender distribution of smokers and the higher sensitivity of females’ to tobacco (14). Therefore, prevention and control of COPD and its relevant early conditions should also be enhanced in females. As shown in our study, the detection rates of obstructive ventilatory dysfunction and obstructive small airway disease increased with age, and the detection rate of COPD was higher in the 6-79 years old group than in the 20-59 years old group. Aging is a risk factor of COPD, and the incidence of COPD increases along with age (15). Thus, special attention should be paid for the screening of COPD, obstructive ventilatory dysfunction, and obstructive small airway disease in mid-aged and elderly populations.
The detection rate of obstructive ventilatory dysfunction increased along with the decrease of education background. Epidemiological studies both in China and abroad have shown that socioeconomic status is a risk factor of COPD and the incidence of COPD increases along with the decrease of socioeconomic status and education background (16). Populations with low socioeconomic status and/or education background are more possible to be exposed to occupational dust, tobacco, biofuels, and other risk factors of COPD. Meanwhile, poor living environment and malnutrition also increase the risk of infections and bronchitis in these populations and thus increase the risk of COPD onset.
According to World Health Organization (WHO) Report on the Global Tobacco Epidemic 2008, 5.4 million people die each year from tobacco-related diseases. In our current study, subjects with a high smoking index (≥30 pack-years) had a higher risk of COPD than non-smokers. The risk of obstructive ventilatory dysfunction was higher in smokers than non-smokers and increased along with the increase of number of cigarettes smoked. Also, subjects with a smoking index of ≥15 pack-years had a higher risk of obstructive small airway disease, which rose along with the increase of number of cigarettes smoked. The incidence of COPD is remarkably higher in smokers than non-smokers (17). Smoking is the main risk factor of COPD. In developing countries, about 90% of COPD deaths were associated with smoking, and smoking intensity is significantly associated with COPD (18,19). Furthermore, smoking is avoidable and controllable. Therefore, as a global joint effort, effective measures should be taken to lower the smoking rate, eliminate the hazard of tobacco, and maintain and promote human health.
The detection rate of COPD, obstructive ventilatory dysfunction, and obstructive small airway disease was not significantly different among subjects with different BMI. An epidemiological study in China had indicated that low BMI might increase the risk of COPD, especially in elderly (60 years and over) populations (20). However, the relationship between BMI and COPD still require further verification in more epidemiological studies with larger sample sizes. Subjects with a history of childhood lower respiratory tract infection, occupational exposure, family history of COPD, and/or fuel exposure, the detection rates of COPD, obstructive ventilatory dysfunction, and obstructive small airway disease were significantly higher thank those in the control groups. Thus, screening and control of COPD should be enhanced in populations with COPD risk factors.
In conclusion, the detection rate of COPD is markedly lower in the health check-up population. However, there are high detection rates of obstructive ventilatory dysfunction and obstructive small airway disease; without prompt intervention, these conditions can gradually progress into COPD. Therefore, routine lung function test should be performed in the health check-up populations, and appropriate interventions should be provided to individuals with abnormal findings, so as to reduce the risk of COPD and thus decrease the familial and socioeconomic burdens and improve the individuals’ quality of life.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shaw JG, Vaughan A, Dent AG, et al. Biomarkers of progression of chronic obstructive pulmonary disease (COPD). J Thorac Dis 2014;6:1532-47. [PubMed]
- Gulati S, Mulshine JL. Lung cancer screening guidelines: common ground and differences. Transl Lung Cancer Res 2014;3:131-8. [PubMed]
- Kuo SJ. To establish continuous improvement mechanism for healthcare-sharing experiences of Changhua Christian Hospital. Ann Transl Med 2014;2:34. [PubMed]
- Lewis G, Hoey ET, Reynolds JH, et al. Multi-detector CT assessment in pulmonary hypertension: techniques, systematic approach to interpretation and key findings. Quant Imaging Med Surg 2015;5:423-32. [PubMed]
- Gao J, Prasad N. Chronic obstructive pulmonary disease in China: the potential role of indacaterol. J Thorac Dis 2013;5:549-58. [PubMed]
- Philip F, Becker M, Galla J, et al. Transient post-operative atrial fibrillation predicts short and long term adverse events following CABG. Cardiovasc Diagn Ther 2014;4:365-72. [PubMed]
- Thiem U, Kállay E, Borchhardt K. Is quarterly bolus vitamin D3 supplementation adequate to prevent childhood pneumonia? Transl Pediatr 2012;1:118-9.
- Johns DP, Walters JA, Walters EH. Diagnosis and early detection of COPD using spirometry. J Thorac Dis 2014;6:1557-69. [PubMed]
- World Health Organization. The 10 leading causes of death in the world, 2000 and 2012. Accessed May 20, 2014. Available online: http://www.who.int/mediacentre/factsheets/fs310/en/
- Mannino DM, Higuchi K, Yu TC, et al. Economic Burden of COPD in the Presence of Comorbidities. Chest 2015;148:138-50. [PubMed]
- Rycroft CE, Heyes A, Lanza L, et al. Epidemiology of chronic obstructive pulmonary disease: a literature review. Int J Chron Obstruct Pulmon Dis 2012;7:457-94. [PubMed]
- Atsou K, Chouaid C, Hejblum G. Variability of the chronic obstructive pulmonary disease key epidemiological data in Europe: systematic review. BMC Med 2011;9:7. [PubMed]
- Fang X, Wang X, Bai C. COPD in China: the burden and importance of proper management. Chest 2011;139:920-9. [PubMed]
- Aryal S, Diaz-Guzman E, Mannino DM. Influence of sex on chronic obstructive pulmonary disease risk and treatment outcomes. Int J Chron Obstruct Pulmon Dis 2014;9:1145-54. [PubMed]
- Landis SH, Muellerova H, Mannino DM, et al. Continuing to Confront COPD International Patient Survey: methods, COPD prevalence, and disease burden in 2012-2013. Int J Chron Obstruct Pulmon Dis 2014;9:597-611. [PubMed]
- Yin P, Zhang M, Li Y, et al. Prevalence of COPD and its association with socioeconomic status in China: findings from China Chronic Disease Risk Factor Surveillance 2007. BMC Public Health 2011;11:586. [PubMed]
- Hou G, Yi Y, Sun L, et al. A study on epidemiological morbidity and risk factors for chronic obstructive pulmonary disease in the populations higher than 35 in communities. Chin Gen Pract 2012;16:1831-3.
- Forey BA, Thornton AJ, Lee PN. Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema. BMC Pulm Med 2011;11:36. [PubMed]
- Zhou Y, Chen R. Risk factors and intervention for chronic obstructive pulmonary disease in China. Respirology 2013;18 Suppl 3:4-9. [PubMed]
- Jiazina T, Hu X, Zhao S, et al. Epidemiologic analysis aged over 60 years people of Uygurs of chronic obstructive pulmonary disease in rural of Xinjiang. J Xinjiang Med Univ 2010;9:1017-20.


