
Prevalence and characteristics of chronic obstructive pulmonary disease in China with a diagnostic criterion of FEV1/FVC less than the lower limit of normal—a reanalysis of Chinese epidemiological survey of COPD (CESCOPD) study
Introduction
Spirometry is still the recommended routine diagnostic procedure of choice for chronic obstructive pulmonary disease (COPD), which is characterized by air flow limitation (1,2). In the past ten years, the incidence of COPD among Chinese individuals over 40 years old has increased from 8.2% in 2002 (3) to 13.7% in 2012 with the criterion of FEV1/FVC <0.7 (4). However, numerous studies have demonstrated that regular changes in FEV1/FVC are seen with aging, which challenges the traditional fixed ratio of 0.7 (5,6). Thus, many scientists believe that the threshold of the lower limit of normal (LLN) of FEV1/FVC should be used to diagnose COPD (7,8). The age-related LLN of FEV1/FVC has been shown to reduce the increases in COPD prevalence seen among the older healthy population when using the fixed-ratio criterion (FEV1/FVC <0.7) and increased the diagnosis among younger patients (9-12). It seems challengeable to promote reference equations globally although the European Respiratory Society(ERS) Global Lung Function Initiative (GLI) have created continuous prediction equations and LLNs for spirometric values with adjustment of fixed ethnic conversion factors (13,14). Possible reasons might be the limited sample size and insufficient representative sample clusters. In 2017, a new age-related LLN reference equation was developed by the Guangzhou Institute of Respiratory Health (GIRH). For the first time, a unified and Chinese-suited LLN reference equation from Chinese healthy people was published through a large-sample and multicenter study (15). Further research has reported that this individual-dependent GIRH-LLN equation appears to perform better at detecting airflow limitations and reduces the risk of underdiagnosis for young adults and overdiagnosis for the elderly (12). Therefore, it is of great necessity to investigate the exact prevalence of COPD in China using this LLN reference equation. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-21-95).
Methods
We retrieved data from participants in the Chinese Epidemiological Survey of COPD (CESCOPD) study for COPD prevalence estimation in residents aged 40 to 80 years with the criterion of the GIRH-LLN. The CESCOPD study was a multicenter, randomized trial with the objective to obtain the COPD prevalence in China through a large-population, spirometry-based, cross-sectional survey of COPD from September 2002 through September 2004. Residents invited in our study were given individual interviews by our trained interviewers using a standardized questionnaire revised from the international BOLD study. All interviewers and spirometry operators had been well trained and accredited before the survey. Questionnaire data were coded and entered into the standardized Excel database (Microsoft, Redmond, WA) by two persons independently, with computer programs checking for out-of-range values and logic mistakes. Participants’ characteristics and prevalence of COPD with the GOLD 0.7 criterion have been published previously (3). Spirometry was conducted using portable spirometers (Micro Medical Ltd, Chatham, Kent, UK), along with the procedure recommended by the American Thoracic Society (ATS) (16). Subjects with airflow limitations defined by the GOLD 0.7 fixed ratio underwent postbronchodilator testing 15 to 20 minutes after inhaling a dose of 200 µg of salbutamol (Ventolin; GlaxoSmithKline, Middlesex, UK) through a 500 ml spacer. Before data collection, each spirometer was calibrated daily with a volume variation of less than 3% by a 3-L syringe. Spirometry results were sent every 2 weeks to Guangzhou for quality control. The results were double-checked by the principal investigator and fed back to each field worker. Subjects with unacceptable measurement were invited to receive a make-up test within 30 days. Spirometry results with grades A, B, or C were considered as acceptable operations. Spirometry and questionnaire-based interview were conducted at a convenient and accessible site or at home. Those residents temporarily out of reach were given a home interview on a later occasion. Interviewers for questionnaire were staff (doctors, nurses) and volunteers from local medical institutions, while pirometry was completed only by doctors and nurses. All interviewers and spirometry operators had been well trained and accredited before the survey. The GOLD 0.7 fixed ratio was used as the diagnostic criterion in the study design, and only participants with an FEV1/FVC <0.7 before a bronchodilator (including a small number of participants with FEV1/FVC around 71% to 70%) accepted the bronchodilation test. For a small group of patients who were underdiagnosed by the GOLD 0.7 fixed ratio (but lack of bronchodilation test), spirometry data collected before bronchodilation were used. Classification of airflow limitation severity in COPD was based on post-bronchodilator FEV1%pred according to the China revised 2002 reference equation [by applying conversion factors from the European Coal and Steel Community 1993 (ECSC93) FEV1 reference equation with males by 0.95 and females by 0.93] (17) and GIRH-LLN FEV1 reference equation.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University approved the study (approved No. 2013-37). All the participants were made fully aware of the purpose of study, and all participants gave informed consent.
Statistical analysis
Multivariate logistic regression models were performed to analyze the odds ratios (ORs) and 95% confidence intervals (CIs) for COPD in relation to potential risk factors. Variables including geographic area, sex, age groups, body mass index (BMI), smoking status, occupational exposure to dusts/gases/fumes, exposure to biomass fuel for cooking or heating, ventilation in the kitchen, family history of respiratory disease, pulmonary problems in childhood, and education were forced into the multivariate logistic regression model. Factors with no statistical difference were removed from the final model. Before multivariate regression, univariate logistic regressions were performed for screening for statistically significant factors. Details of the definition of risk factors are given in the published literature (3). Categorical variables such as COPD stage differences and comparison of the distributions of clinical outcomes between the GIRH-LLN criterion and GOLD 0.7 fixed ratio were analyzed using chi-squared tests. A P value <0.05 was considered statistically significant. All analyses were performed using IBM SPSS 19.0.
Results
Among 20,245 participants who completed acceptable spirometry (grades A, B, or C) and questionnaires in the survey, 19,802 people aged 40 to 80 years were included in our reanalysis. A total of 443 participants older than 80 years were removed for lack of the expected reference value of FEV1/FVC (Figure 1).
COPD prevalence
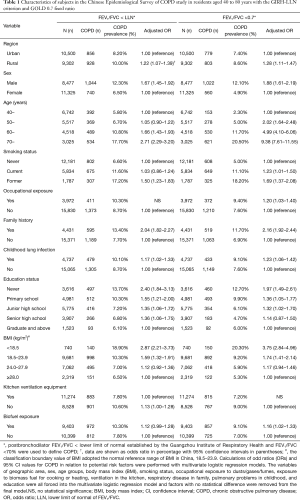
The COPD prevalence was 9.0% (1,784/19,802) among participants aged 40–80 years in China with the GIRH-LLN criterion, which was slightly higher than the GOLD 0.7 fixed ratio (8.0%). The COPD prevalence from different regions are shown in Figure 2. Shanghai had the lowest prevalence of 5.0%, while Chongqing had the highest prevalence of 14.6%. With the GIRH-LLN criterion, the COPD prevalence was higher in most regions than that of GOLD 0.7 fixed ratio, except for the rural areas of Shanghai, Guangzhou and Tianjin that showed lower prevalence. On the whole, the COPD prevalence was significantly higher in rural (10.0%) areas compared with urban areas (8.2%) (Table 1). More remarkably, the COPD prevalence in rural areas increased by 1.4 percentage points (from 8.6% to 10%), while in urban areas, it only increased by 0.8 percentage points (from 7.4% to 8.2%) when compared with the GOLD 0.7 fixed ratio. Great prevalence imparities were also observed in sex distribution. The COPD prevalence in females was 6.5%, which was1.6 percentage points higher than diagnosed by the GOLD 0.7 fixed ratio, but only 0.2 percentage points higher when compared with males (Table 1).

Full table
Risk factors
Multivariate logistic regression analyses showed that, consistent with the GOLD 0.7 fixed ratio, smoking, pulmonary problems in childhood, family history of respiratory diseases, male sex, low education level, aging, lower BMI, and occupational exposure (dusts/gases/fumes) are associated with COPD when the GIRH-LLN criterion was used. The adjusted ORs (95% CIs) of these potential risk factors are shown in Table 1. Significantly, COPD prevalence was higher in participants never smoked (6.6% for LLN vs. 5.0% for GOLD), and poor ventilation in the kitchen seems to be harmful to COPD (OR 1.13, 95% CI: 1.00–1.28). Age distribution showed a higher prevalence in people under 60 years of age but lower in participants over 60 years of age compared to the GOLD 0.7 fixed-ratio standard (Table 1).
Symptoms and severity distribution
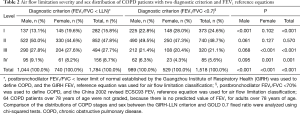
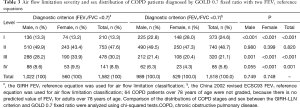
Under the GIRD-LLN reference equation for the FEV1 expected value, the percentage of COPD in stages I (mild), II (moderate), III (severe), and IV (very severe) were 15.8%, 47.8%, 27.7%, and 8.7%, respectively. The COPD percentage in stage I classified by the GIRH-LLN reference equation was obviously lower than that classified by the China revised ECSC1993 equation (15.8% vs. 24.6%, P<0.001), while patients in stages III and IV were relatively higher than that classified by the China revised ECSC1993 equation (27.7% vs. 21.1%, P<0.001 for stage III; 8.7% vs. 5.6%, P=0.001 for stage IV, Table 2). This kind of similar phenomenon can also be found in COPD patients diagnosed by FEV1/FVC less than 70%, but the GIRH-LLN FEV1 reference equation was used (P<0.001, for stage I; P<0.001, for stage III; P=0.001, for stage IV) (Table 3).
Full table
Full table
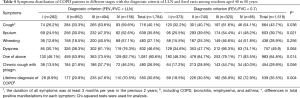
The prevalence of respiratory symptoms, such as cough, sputum, wheezing, and dyspnea in patients with COPD was 40.1%, 35.8%, 27.1%, and 46.6%, respectively (Table 4). A total of 60.6% of COPD patients had at least one of the above respiratory symptoms, which was slightly lower than that of the GOLD 0.7 fixed-ratio criterion (64.8%, P=0.014), reflecting that a higher proportion of patients with COPD were asymptomatic (39.4%). Patients with respiratory symptoms gradually increased with the aggravation of airflow limitation. Notably, with GIRD-LLN FEV1 reference equation, only 30.8% of patients with COPD had ever been “diagnosed” with emphysema, asthma, bronchitis, or COPD, which was lower than that of the GOLD 0.7 fixed-ratio with China 2002 revised equation (35.5%, P=0.004), especially in stage I–II (9.9% vs. 18.5% for stage I, and 20.8% vs. 30.5% for stage II, Table 4).
Full table
Discussion
As a noninvasive and readily available test, spirometry is the most reproducible and objective diagnostic measurement of airflow limitation. The COPD prevalence varied among different criteria, such as the fixed-ratio and GIRH-LLN. In our study, a higher total morbidity but younger incidence, more female patients, and increased severe patient proportion were detected with the GIRH-LLN criterion than with the GOLD 0.7 fixed ratio.
With the GIRH-LLN criterion, the COPD prevalence was 1.0% higher than that of the GOLD 0.7 fixed ratio (8.0%) among participants aged 40–80 years in China, especially the higher prevalence in women. This was consistent with another large study conducted in China, which GLI2012 LLN was used (18). Of which, airflow obstruction prevalence defined as FEV1/FVC <0.7 was 4.0% in females and 5.1% in males, and 5.9%, 5.2% respectively when FEV1/FVC < LLN was used (spirometry data of pre-bronchodilator was used). COPD prevalence was 1.9 percentage points higher than the GOLD 0.7 fixed ratio for females, but only 0.1 percentage points higher with males. A recent study reported that the overall prevalence of spirometry-defined COPD was 8.6% (95% CI: 7.5–9.9), accounting for 99.9 (95% CI: 76.3–135.7) million people with COPD in China. In people aged 40 years or older, the COPD prevalence was increased to 13.7% (12.1–15.5) (4). COPD patients would be even higher if the GIRH-LLN criterion was used because of China's large population base. In particular, it is of great significance in improving early diagnosis and prevention in patients underdiagnosed by GOLD, because of their impaired ventilation and faster lung function decline (12).
Significantly, those newly diagnosed patients by LLN were not found to have higher smoking rates, but were predominantly rural and females, with high rates of biofuel explosion and poor kitchen conditions (Table 1). Biofuels are still the most important source of fuel in Chinese vast rural areas, especially over the past 20 years. As the primary undertakers of kitchen work, women are the main demographic who come into contact with biofuels. Biofuel smoke exposure has been found to be associated with COPD in rural and urban women (19). Moreover, these exposed residents always tend to have poor kitchen ventilation (20), as shown in our past studies. In addition, some other insights from the study of patients with COPD without a major causal factor are likely to provide insights into factors that contribute to endogenous immunological mechanisms. Many of them tended to be elderly women with a history of organ specific autoimmune disease and peripheral blood lymphopenia (21). More common in men many years ago, COPD now affects men and women almost equally (22). In Norway, the prevalence declined in men but not in women from 1995–1997 and 2006–2008 (23).
There are differences in COPD severity classification between these two criteria. The COPD percentage in stage I classified by the GIRH-LLN reference equation was obviously lower, while patients in stages III and IV were relatively higher than that classified by the ECSC1993 equation. What we have proved is that the GOLD criterion has caused a portion of the patients to be misdiagnosed as having COPD (12). These patients tend to be of a relatively high age, with lung function above the predicted value of 80%. Actually, lung function in these patients is a part of the normal evolution of the population (24-26), which may result in the lower stage I incidence, when they were excluded by the GIRH-LLN criterion. In contrast, the increased female patients, especially rural women patients, were the major contributors to the increased prevalence of COPD with the GIRH-LLN criterion, and many of them had a FEV1%pred less than 80%. These subjects accounted for the higher proportion of patients with COPD stage II and above to a certain extent. Meanwhile, in the CESCOPD, we have used the adjusted ECSC93 FEV1 predicted value by applying conversion factors (males by 0.95 and females by 0.93) for the assessment of COPD severity (China revised 2002 reference equation), and it was established by collecting lung function data (4,773 subjects) in 1996–2002. While the new GIRH-LLN FEV1 reference equation was established ten years later with a larger sample size, stricter random sampling and better quality spirometry would be much individualized. Moreover, in the past 20 years, the overall nutritional status of people in China has been significantly improved, and they are physically stronger and taller than before (27,28), which may have narrowed the gap of lung function with the Europeans. All these things may lead to some bias in the estimation of the FEV1 predicted value with the China revised 2002 reference equation. Nevertheless, because there is no predicted value of FEV1 for adults over 78 years of age, 64 COPD patients could not be further identified by the ECSC93 criterion, as did the China revised 2002 reference equation.
The higher proportion of asymptomatic COPD patients and lower diagnosis with GIRH-LLN criterion, suggesting that less attention may be paid to their bodies. For symptoms are the main motivator for hospital visits and recommendation for spirometry by GOLD. Studies have shown that subjects in stages I and II followed a trajectory of rapidly declining FEV1 (29). Meanwhile, these subjects had poorer exercise tolerance than healthy controls upon exertion, and a significant proportion of them had dynamic hyperinflation (30) though few of them presented chronic symptoms. These subjects may, therefore, deserve further attention and may warrant regular follow-up.
Overall, our study findings have important public health implications. First, we have almost accurately evaluated the prevalence of COPD under the criterion of GIRH-LLN from a national wide, randomized, cross-sectional and multi-center survey. Increased prevalences were detected in rural areas and female residents. Indicating sufficient attention should be taken by the government, and possible etiology and related mechanisms should be actively explored. And then, for the first time, we found significant differences between different FEV1 reference equations on COPD severity classification. Results showed that airflow limitation severity determining will be even worse when GIRH FEV1 reference equation was used. The GIRH-LLN we have chosen was established through a large-sample, multicenter and all Chinese originated study. Further research has evidenced its advantages on detecting airflow limitations to reduce the risk of underdiagnosis for young adults and overdiagnosis for the elderly. It seems more Chinese-suitable and convincing to be recommended nationwide. Moreover, the CESCOPD study was a rare large-sample multicenter epidemiological investigation with strict random sampling and data quality control in China. It is of great representative for assessing COPD prevalence among people over 40 years of age.
There also exists some limitations in our study. One hundred and fifty-eight patients underdiagnosed by the GOLD 0.7 fixed ratio used spirometry data collected before bronchodilation, which may lead to a slightly higher prevalence of COPD. Consistent with the findings (3.1%) of Johannessen and colleagues (31), our published article reported 3.3% of the population had a low ratio of FEV1/FVC (<70%) before bronchodilation and a normal ratio (FEV1/FVC ≥70%) after bronchodilation in the present study (3). However, there was no statistically significant difference in diagnostic property when using pre- or postbronchodilator FEV1/FVC among people with respiratory symptoms in the studies by Mohamed and Kato (32,33). On the other hand, it is difficult to define patients newly diagnosed by LLN as COPD precisely (34), for a few of them may possibly have small lungs (35). The same is true for GOLD. Another situation, they do have respiratory impairment. Whether these populations are pre-COPD or early-stage COPD is controversial. Our previous study has demonstrated that the underdiagnosed participants (by GOLD) showed more symptoms, impaired ventilation and faster lung function decline through a two-year longitudinal follow-up research compared with normal participants (12), prefer to support a think of early stage of COPD. Certainly, longer-term follow-up of these populations may be more helpful to assess their health status.
Conclusions
In conclusion, the COPD prevalence with the GIRH-LLN criterion was slightly higher than with the GOLD 0.7 fixed-ratio criterion, especially in women and rural participants. These residents always showed little symptoms and low diagnosis, suggesting serious attention should be paid to them.
Acknowledgments
Funding: The study was funded by National natural science foundation of China (81900044, to Dr. S Liu) for project implementation, data acquisition, draft and Statistical analysis; by National 13th Five-Year Key RESEARCH and development plan (2016YFC1304101, to Prof. P Ran) for project implementation and data acquisition, article processing charges and open access fee; by the key project of Hunan Provincial Health Commission (20201922, to Prof. X Tan) for project implementation, data acquisition; by Natural Science Foundation of Guangdong, China (2020A1515010264, to Dr. W. Zou) for data acquisition.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-21-95
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-21-95
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-21-95). All authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University approved the study (approved No.2013-37). All the participants were made fully aware of the purpose of study, and all participants gave informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med 2017;195:557-82. [Crossref] [PubMed]
- Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease (2021 reports). Available online: https://goldcopd.org/2021-gold-reports/
- Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med 2007;176:753-60. [Crossref] [PubMed]
- Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health CPH study): a national cross-sectional study. Lancet 2018;391:1706-17. [Crossref] [PubMed]
- Culver BH. How should the lower limit of the normal range be defined? Respir Care 2012;57:136-45, 143-5.
- Stanojevic S, Wade A, Stocks J, et al. Reference ranges for spirometry across all ages: a new approach. Am J Respir Crit Care Med 2008;177:253-60. [Crossref] [PubMed]
- Cerveri I, Corsico AG, Accordini S, et al. Underestimation of airflow obstruction among young adults using FEV1/FVC <70% as a fixed cut-off: a longitudinal evaluation of clinical and functional outcomes. Thorax 2008;63:1040-5. [Crossref] [PubMed]
- Vaz Fragoso CA, Concato J, McAvay G, et al. The ratio of FEV1 to FVC as a basis for establishing chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010;181:446-51. [Crossref] [PubMed]
- Vollmer WM, Gislason T, Burney P, et al. Comparison of spirometry criteria for the diagnosis of COPD: results from the BOLD study. Eur Respir J 2009;34:588-97. [Crossref] [PubMed]
- Luoto JA, Elmstahl S, Wollmer P, et al. Incidence of airflow limitation in subjects 65-100 years of age. Eur Respir J 2016;47:461-72. [Crossref] [PubMed]
- Güder G, Brenner S, Angermann CE, et al. GOLD or lower limit of normal definition? A comparison with expert-based diagnosis of chronic obstructive pulmonary disease in a prospective cohort-study. Respir Res 2012;13:13. [Crossref] [PubMed]
- Liu S, Zhou Y, Liu S, et al. Clinical impact of the lower limit of normal of FEV1/FVC on detecting chronic obstructive pulmonary disease: A follow-up study based on cross-sectional data. Respir Med 2018;139:27-33. [Crossref] [PubMed]
- Ben Saad H, El AM, Hadj MK, et al. The recent multi-ethnic global lung initiative 2012 (GLI2012) reference values don't reflect contemporary adult's North African spirometry. Respir Med 2013;107:2000-8. [Crossref] [PubMed]
- Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J 2012;40:1324-43. [Crossref] [PubMed]
- Jian W, Gao Y, Hao C, et al. Reference values for spirometry in Chinese aged 4-80 years. J Thorac Dis 2017;9:4538-49. [Crossref] [PubMed]
- Standardization of Spirometry. 1994 Update. American Thoracic Society. Am J Respir Crit Care Med 1995;152:1107-36. [Crossref] [PubMed]
- Zheng J, Zhong N. Normative values of pulmonary function testing in Chinese adults. Chin Med J (Engl) 2002;115:50-4. [PubMed]
- Smith M, Li L, Augustyn M, et al. Prevalence and correlates of airflow obstruction in ~317 000 never-smokers in China. Eur Respir J 2014;44:66-77. [Crossref] [PubMed]
- Sana A, Somda S, Meda N, et al. Chronic obstructive pulmonary disease associated with biomass fuel use in women: a systematic review and meta-analysis. BMJ Open Respir Res 2018;5:e000246 [Crossref] [PubMed]
- Zhou Y, Wang C, Yao W, et al. COPD in Chinese nonsmokers. Eur Respir J 2009;33:509-18. [Crossref] [PubMed]
- Pavord ID, Yousaf N, Birring SS. Chronic obstructive pulmonary disease in non-smokers. Lancet 2009;374:1964, 1965-66.
- World Health Organisation. Chronic obstructive pulmonary disease (COPD). 2016. Available online: http://www.who.int/mediacentre/factsheets/fs315/en/ (accessed 15 Jun 2017)
- Bhatta L, Leivseth L, Mai XM, et al. Prevalence and trend of COPD from 1995-1997 to 2006-2008: The HUNT study, Norway. Respir Med 2018;138:50-6. [Crossref] [PubMed]
- Akkermans RP, Biermans M, Robberts B, et al. COPD prognosis in relation to diagnostic criteria for airflow obstruction in smokers. Eur Respir J 2014;43:54-63. [Crossref] [PubMed]
- Akkermans RP, Berrevoets MA, Smeele IJ, et al. Lung function decline in relation to diagnostic criteria for airflow obstruction in respiratory symptomatic subjects. BMC Pulm Med 2012;12:12. [Crossref] [PubMed]
- Sator L, Horner A, Studnicka M, et al. Overdiagnosis of COPD in Subjects With Unobstructed Spirometry: A BOLD Analysis. Chest 2019;156:277-88. [Crossref] [PubMed]
- Yang XG, Li YP, Ma GS, et al. Study on weight and height of the Chinese people and the differences between 1992 and 2002. Zhonghua Liu Xing Bing Xue Za Zhi 2005;26:489-93. [PubMed]
- Song Y, Hu PJ, Zhang B, et al. Secular trends of height among Chinese students aged 17 in 18 ethnic minorities from 1985 to 2010. Beijing Da Xue Xue Bao Yi Xue Ban 2015;47:414-9. [PubMed]
- Lange P, Celli B, Agusti A, et al. Lung-Function Trajectories Leading to Chronic Obstructive Pulmonary Disease. N Engl J Med 2015;373:111-22. [Crossref] [PubMed]
- Soumagne T, Laveneziana P, Veil-Picard M, et al. Asymptomatic subjects with airway obstruction have significant impairment at exercise. Thorax 2016;71:804-11. [Crossref] [PubMed]
- Watz H, Tetzlaff K, Magnussen H, et al. Spirometric changes during exacerbations of COPD: a post hoc analysis of the WISDOM trial. Respir Res 2018;19:251. [Crossref] [PubMed]
- Mohamed Hoesein FA, Zanen P, Sachs AP, et al. Spirometric thresholds for diagnosing COPD: 0.70 or LLN, pre- or post-dilator values? COPD 2012;9:338-43. [Crossref] [PubMed]
- Kato B, Gulsvik A, Vollmer W, et al. Can spirometric norms be set using pre- or post- bronchodilator test results in older people? Respir Res 2012;13:102. [Crossref] [PubMed]
- Schermer TR, Robberts B, Crockett AJ, et al. Should the diagnosis of COPD be based on a single spirometry test? NPJ Prim Care Respir Med 2016;26:16059. [Crossref] [PubMed]
- Postma DS, Bush A, van den Berge M. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet 2015;385:899-909. [Crossref] [PubMed]



