
Optimal aerobic exercise intensity and its influence on the effectiveness of exercise therapy in patients with pulmonary arterial hypertension: a systematic review
Introduction
Pulmonary arterial hypertension (PAH) is a rare and progressive disease characterized by the progressive development of dyspnea and fatigue with increasing deterioration of exercise tolerance (1,2). Treatment with medication is a first option to reduce mortality and to improve dyspnea (3). Exercise therapy has been suggested as a treatment option for patients with PAH since 2000, and the clinical evidence for this has been increasing (4).
An evidence-based randomized controlled study on exercise effects in patients with pulmonary hypertension was reported for the first time in 2006 (5), and a meta-analysis that compared the effects of exercise therapy was published in 2015 (6). Several studies (5,7-9) demonstrated that exercise therapy for PAH patients contributed to improved exercise capacity, quality of life (QOL), muscle strength, and respiratory muscle strength. The exercise types typically included aerobic exercise, resistance training, and respiratory muscle strength exercise (10).
Considering the safety and efficacy of exercise therapy for patients with PAH, optimal exercise intensity is an important factor to prevent adverse events and to increase the effectiveness of exercise therapy (11-13). High intensity exercise can cause severe adverse events including arrhythmias, syncope, and respiratory disease in 13% of these patients (11).
Exercise intensity was usually prescribed and monitored using heart rate (HR), pulse oxy-hemoglobin saturation (SpO2), and rating of perceived exertion (RPE) in PAH patients (12,14-17). Some criteria including HR below 120 bpm and SpO2 below 85% were used as termination criteria during exercise training in individuals with PAH (15,17-21).
However, the majority of review articles (6,7,10,13) have focused their investigations on the effectiveness of exercise interventions with respect to exercise capacity, muscle strength, and QOL. The improvement of exercise tolerance may be different according to the applied exercise intensity. Applying different exercise intensities is associated with different levels of effectiveness in endothelium-dependent vasodilation, depending on the interaction between the intensities of both exercises (22).
Therefore, the objective of this review was to investigate the effects of exercise-based cardiac rehabilitation programs according to exercise intensity to improve exercise capacity and QOL, and to describe the termination criteria used during exercise training in patients with World Health Organization (WHO) Group 1 of pulmonary arterial hypertension.
We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/jtd-20-3296).
Methods
Protocol and registration
The protocol was registered with PROSPERO (PROSPERO2020: CRD42020184937). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed.
Eligibility criteria
The following PICOS (Participants, Interventions, Comparison, Outcome, and Study Design) criteria were used to generate our research:
- Participants: patients with WHO Group 1 of PAH;
- Intervention: exercise training;
- Comparison: exercise intensity, termination criteria;
- Outcome: exercise capacity, QOL;
- Study design: randomized controlled trials (RCTs), prospective studies, and observational studies.
Search strategy
This literature review search was performed using the PubMed, EMBASE, and CINAHL databases, which were searched using the following terms: (“Exercise”[Mesh] or “Exercise Therapy”[Mesh] or “Cardiac Rehabilitation”[Mesh] or “Resistance Training”[Mesh]) and (“Hypertension, Pulmonary”[Mesh] or “Pulmonary Arterial Hypertension (PAH)”[Mesh]). The search included articles published between 1980 and June 2020, and all articles identified in the search were evaluated.
Criteria for inclusion
Studies were included if they met the following criteria: RCTs or prospective observational studies or case series with comparisons between before and after exercise therapy. The participants were diagnosed as WHO Group 1, defined as PAH. The studies with case reports and literature reviews and trials that included other WHO group of pulmonary hypertension groups were excluded. Articles written in languages other than English were also excluded.
Study selection
Two reviewers (YGS and SKO) independently reviewed the studies and extracted articles that met the inclusion criteria according to the review protocol. They screened the articles by checking titles and abstracts first, and then full texts. A third reviewer (JS) reviewed the full text of an article to determine whether it should be included in cases where the original two reviewers had disagreements about those articles.
Quality of selected articles
The quality of each study was assessed using Sackett’s level of evidence scale from the strongest (rating =1) to weakest (rating =5), where ranked RCTs are considered the highest level and case series or expert opinions are considered the lowest level (Table 1).

Full table
Statistical analysis
Due to the heterogeneity and non-uniformity of the data in the included studies, the results are summarized in a descriptive manner.
Results
Study selection
In total, 1,452 articles were found according to the process of this study, and the results are as follows. The numbers of article types (RCTs, prospective studies, case series) found in PubMed, EMBASE, and CINAHL were 637, 684, and 131, respectively. Eight articles from the 1,452 were selected. Three were RCTs, 3 were prospective studies, and 2 were case series (Figure 1).
Study characteristics
The most common types of PAH were idiopathic and connective tissue disease. Most of the patients had functional classifications from II to III, and only three trials (9,14,16) included patients with functional classification IV. A summary of the included studies has been provided in Table 2. The common inclusion criteria were adults aged 18 and older, medically stable condition, and no change in medication therapy for 3 months before participation.

Full table
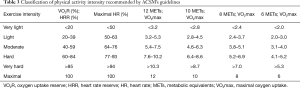
Classification of aerobic exercise intensity
Heart rate domains were used in the majority of studies to prescribe target exercise intensity, and %peak oxygen uptake (peak VO2) was used in one study (19). Aerobic exercise intensity ranged from 50% to 80% of %heart rate reserve (HRR) or %maximal heart rate (HRmax) or %peak VO2. For the purposes of this review article, exercise intensity was categorized into 3 different groups according to American College of Sports Medicine (ACSM) guidelines (Table 3) (23); the low-intensity exercise group required less than 120 bpm or a rating perceived exertion (RPE) of 13 to perform (18,20), the moderate to vigorous-intensity exercise group required 60–80% of HRmax or 50–70% of peak VO2 (9,12,19,21), and the vigorous-intensity exercise group required 70–80% of HRR (14,16) to perform.
Full table
Exercise capacity
The six-minute walk test (6MWD) and cardiopulmonary exercise test (CPET) are conducted to evaluate exercise capacity. All studies reported the results of the 6MWD, while the CPET was not conducted in two trials (9,12). The baseline 6MWD was reported to range from 375±92 to 496±108 m in the reviewed articles. The improvement seen in the 6MWD ranged from 37 to 81 m, and the median value was 56 m. In the low intensity group, one study did show non-significant change (18) and others reported an improvement of 39 m (20). The moderate to vigorous group reported improvements in the 6MWD of 37 m (19), 71 m (21), 81 m (9), and 67 m (12). Changes in the vigorous-intensity group were 56 m (14) and 53 m (16). The CPET was conducted with a treadmill in three studies and with a cycling ergometer in another three studies. At baseline, maximal oxygen uptake ranged from the lowest level of 11.4±2.2 mL/kg/min (12) to the highest level of 17.6 mL/kg/min (14). The improvement in peak VO2 showed a range from 0.3 to 2.3 mL/kg/min, and the highest improvement of 14% was reported in the study conducted by Grünig et al. (21). Two trials (9,20) did not conduct the CPET, and one trial did not report the results of post-intervention evaluations (Table 4).

Full table
QOL
The 36-Item Short Form Health Survey (SF-36) and the Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR) questionnaire were used to evaluate QOL in the reviewed articles. Of two studies in the low-intensity group, one did not evaluate QOL and the other showed no significant difference in the SF-36 domains. In the moderate to vigorous-intensity group, three studies (12,19,21) reported the results of QOL, but one trial (9) did not measure QOL. Of these articles, one article (12) showed a significant improvement in the bodily pain domain (P=0.05). A study reported by Grünig et al. (21) showed that the SF-36 domains including physical function, general health, vitality, social function, and mental health demonstrated significant improvements. Another study (10) did not report a significant difference after an intervention of 10 weeks. In the vigorous-intensity group, one trial (14) of two articles reported a significant improvement in SF-36 domains including physical function, role physical, general health, vitality, social function, and mental health and the other study did not conduct an evaluation of QOL (16). The CAMPHOR questionnaire was only used in a study conducted by Chan et al. (14), who reported an improvement in the domains of QOL, symptoms, and energy. Mental domains showed greater improvement when compared to the physical domains for the SF-36 questionnaire (12,14,21).
Criteria for terminating exercise
For safety in exercise training, four of the eight reviewed articles suggested the criteria for terminating exercise as heart rates more than 120 bpm (18,20) or 130 bpm (9), less than 85% (9,18,20) of SpO2, or >6 on the Borg scale (20).
Discussion
This study showed that moderate or higher intensity aerobic exercise was associated with an improvement in exercise capacity and QOL and that HR and SpO2 were most commonly used for the termination criteria.
Classification of aerobic exercise intensity
A proper definition of aerobic exercise intensity is important to enhance the effectiveness of exercise therapy and to prevent the occurrence of adverse events during exercise (24). Cardiovascular adaptations to training are intensity-dependent, and exercise intensity has emerged as an important variable in clinical investigations (22,25). Exercise intensity domains for aerobic exercise include %HRmax, %HRR, %peak VO2, and %VO2max (26). Some systematic review articles reported that recommended aerobic exercise intensity is 60 to 80%peak VO2 or %HRR (7,13). In this study, the common domains used for exercise intensity were %peak VO2, %HRmax, and %HRR. According to ACSM guidelines (23), exercise intensity is classified into low-intensity physical activity at 20–39%, moderate-intensity activity at 40–59%, and high-intensity activity at 60–84% of peak VO2 or HRR. When expressed as a percentage of the HRmax, low-intensity activity is 40–63%, moderate-intensity activity is 64–76%, and vigorous-intensity activity is 76–90%. We classified these reviewed articles into 3 different groups based on ACSM guidelines: a low-intensity group, a moderate to vigorous-intensity group, and a vigorous-intensity group. In the low-intensity group, the exercise capacity and QOL did not show significant improvement after the exercise intervention. The results in the moderate to vigorous-intensity group were similar to those in the vigorous-intensity group. This finding differs from previous studies (5,27) that recommended low-intensity exercise might be a beneficial intervention to improve clinical outcomes in PAH patients. Therefore, further study with high quality RCTs is required to confirm the effects of different exercise intensities on exercise tolerance and QOL in patients diagnosed with PAH.
Exercise capacity
The six-minute walk test in PAH patients has been widely used to measure exercise capacity and to predict prognoses (28). In the reviewed articles, the 6MWD was reported in all trials, and the highest improvement was shown to be 81 m in the moderate to vigorous-group. The range of improvement in the 6MWD was 31 to 81 m; this is similar to the result of a systematic review, which reported an improvement range from 17 to 96 m in patients with PAH (7). The mean improvement of 6MWD was 57.7 m in this study, a greater improvement than that reported in a previous study, which was a mean improvement of 33.8 m for those in WHO Group 1 (29). Another previous study reported that an increase in 6MWD of over 41 m may be the minimally important distance for clinical significance (30). On the basis of this report, two studies in the low-intensity group and one in the moderate to vigorous-intensity group did not achieve the improvement of a clinically significant distance of ≥41 m. Two RCT studies in the vigorous-intensity group showed increases in the 6MWD of over 41 m. The differences among the groups might be explained by the different exercise durations and frequencies applied in each study, which may have affected the results. An RCT applying the same exercise duration and frequency is required to confirm differences between groups according to different exercise intensities. Another clinical outcome regarding exercise capacity is the maximal oxygen uptake measured by CPET, and the improvement, in the present study, is similar to the results (1.1 to 2.1 mL/kg/min) reported by Babu et al. (7). Of the reviewed articles, we were not able to compare the results between three trials, because two trials did not conduct the CPET and one did not report post intervention results (18). In the low-intensity group, maximal oxygen uptake was not reported. The highest change (2.3 mL/kg/min) in peak VO2 was revealed in the moderate to vigorous-intensity group with 60–80% of HRmax, and the mean improvement was 7% in three studies. The vigorous-intensity group showed a mean increase of 4.5%. The mean value was higher in the moderate to vigorous-intensity group than in the other intensity groups and the reason for this needs to be investigated in future studies.
QOL
Patients with PAH have anxiety and depression, and this could lead to a decrease in QOL (31). The generic SF-36 questionnaire was used in most of the studies, and CAMPHOR was used for measuring disease-specific conditions (32). A decreased QOL is associated with an increased mortality in patients with PAH (33). In the reviewed articles, the generic SF-36 was commonly used to measure QOL and only one study used a disease-specific CAMPHOR questionnaire. In particular, PAH patients report a reduced QOL in the physical components of the SF-36 domains (34,35). This review study showed that the physical components score was lower than the mental health components score.
One study in the low-intensity group (20) did not show a significant change after an exercise intervention of 12 weeks. Additionally, a study (19) conducted for 8 weeks with a moderate to vigorous-intensity of 50–70% of peak VO2 showed no significant difference in QOL pre- post-training. The exercise frequency in the two studies was 3 times per week, and this frequency was lower than other studies (14,21) that demonstrated a significant difference in QOL pre- post-training. Three of the eight studies showed a statistically significant difference in SF-36 domains including bodily pain, physical function, general health, vitality, social function, and mental health pre- post-training. The studies had different levels of improvement in 6MWD, and the study conducted by Grünig et al. (21) reported an increase of 71 m after the exercise intervention. Another study (21) also showed the highest significant improvement in the SF-36 domains, while one study with an RCT with the lowest improvement in 6MWD (37 m) showed no significant difference in QOL scores pre- post-training. The difference among the moderate to vigorous intensity-groups may be explained by the correlation between the 6MWD and QOL. That is, improvement in the 6MWD is associated with increased QOL in individuals with PAH (36,37). Study design also should be considered as a reason for this difference, because the prospective study and RCT showed different results despite applying the same exercise intensity. For the vigorous-intensity groups included in two studies, one study reported a significant change in the SF-36 domains including physical function, role physical, general health, vitality, social function, and mental health. Two studies were showed similar results for the 6MWD, but two results could not be compared among the studies, because one study did not evaluate QOL.
The CAMPHOR questionnaire is a disease-related questionnaire for patients with PAH and has superior psychometric properties, compared with the SF-36 (38). The specific disease-related CAMPHOR was only reported in a study conducted by Chan et al. (14) of our reviewed articles. Therefore, further study is needed to measure QOL using the CAMPHOR questionnaire in PAH patients to confirm the relationship between the disease-specific questionnaire and QOL.
Termination criteria
Timing for exercise termination is an important factor to consider to prevent adverse events due to participation in an exercise program (11,12). Some adverse events that included respiratory and gastrointestinal infections were reported in the reviewed articles (12,21). Several parameters such as HR, SpO2, and RPE were used to monitor patient state in four studies (9,15,18,20). The criterion for an HR upper limit of 120 bpm has commonly been used as an indication for termination, and it was also recommended as a target HR for inpatient cardiac patients (22). Hypoxemia may contribute to a sensation of dyspnea by predisposing the respiratory muscles to fatigue (39). Portable pulse oximetry is commonly used to measure oxygen saturation during exercise. The termination criterion with respect to SpO2 was defined as when the SpO2 dropped to less than 85% or 88% in several studies (9,15,18,20). Oxygen saturation ≤88% is referred to as resting hypoxemia, and maintaining this criterion is thought to be an important part of exercise in PAH patients (40). Another termination criterion was Borg’s scale (10-point scale) for RPE, and dyspnea ratings between 3 and 5 have been recommended as the proper exercise intensity in patients with COPD (40). In this review study, only one study by Butāne et al. (20) used Borg’s scale to monitor the severity of dyspnea and recommended a rating of more than 6 as a termination criterion. However, the majority of the reviewed studies did not suggest termination criteria, and there was no consensus among the studies on what such criteria should consist of. Therefore, more strict termination criteria are needed to prevent adverse events or for safety during exercise training in patients from WHO Group 1.
Limitations
There are several limitations in this review article. First, only 3 large databases, PubMed, EMBASE, and CINAHL, were searched, despite the existence of some other large and relevant databases such as CENTRAL and PEDRo. Second, the subjects enrolled in the present study were patients in WHO Group 1. In addition, there were lack studies on low intensity exercise in reviewed articles since only WHO group 1 in pulmonary hypertension is included. Therefore, it is not suitable to apply the results of this trial to other PH groups. A future study is needed to confirm differences in the effects of different exercise intensities in each PH group. Third, the reviewed articles did not include sufficient RCTs. That is, the evidence level is poor with respect to confirming the effectiveness of different exercise intensities in individuals with PAH. Large clinical trials designed as RCTs with long-term follow up are required to determine the role of exercise intensity in exercise programs for PAH patients.
Conclusions
The main findings in this study suggest that aerobic exercise at moderate or higher intensity is needed to improve exercise tolerance and QOL in PAH patients, but the quality of evidence is low. Additional RCTs are needed to compare the effects of different exercise intensities, and strict termination criteria are warranted in individuals diagnosed with WHO Group 1 of PAH.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/jtd-20-3296
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure (available at https://dx.doi.org/10.21037/jtd-20-3296). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hoeper MM, Bogaard HJ, Condliffe R, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol 2013;62:D42-D50. [Crossref] [PubMed]
- Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2013;62:D34-41. Erratum in: J Am Coll Cardiol 2014;63:746. [Crossref] [PubMed]
- Galiè N, Corris PA, Frost A, et al. Updated treatment algorithm of pulmonary arterial hypertension. JACC 2013;62:D60-72. [Crossref] [PubMed]
- Richter MJ, Grimminger J, Kruger B, et al. Effects of exercise training on pulmonary hemodynamics, functional capacity and inflammation in pulmonary hypertension. Pulm Circ 2017;7:20-37. [Crossref] [PubMed]
- Mereles D, Ehlken N, Kreuscher S, et al. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation 2006;114:1482-9. [Crossref] [PubMed]
- Yuan P, Yuan XT, Sun XY, et al. Exercise training for pulmonary hypertension: a systematic review and meta-analysis. Int J Cardiol 2015;178:142-6. [Crossref] [PubMed]
- Babu AS, Padmakumar R, Maiya AG, et al. Effects of Exercise Training on Exercise Capacity in Pulmonary Arterial Hypertension: A Systematic Review of Clinical Trials. Heart Lung Circ 2016;25:333-41. [Crossref] [PubMed]
- Chan L, Chin LM, Kennedy M, et al. Benefits of intensive treadmill exercise training on cardiorespiratory function and quality of life in patients with pulmonary hypertension. Chest 2013;143:333-43. [Crossref] [PubMed]
- Kabitz HJ, Bremer HC, Schwoerer A, et al. The combination of exercise and respiratory training improves respiratory muscle function in pulmonary hypertension. Lung 2014;192:321-8. [Crossref] [PubMed]
- Nogueira-Ferreira R, Moreira-Gonçalves D, Santos M, et al. Mechanisms underlying the impact of exercise training in pulmonary arterial hypertension. Respir Med 2018;134:70-8. [Crossref] [PubMed]
- Grünig E, Lichtblau M, Ehlken N, et al. Safety and efficacy of exercise training in various forms of pulmonary hypertension. Eur Respir J 2012;40:84-92. [Crossref] [PubMed]
- Becker-Grünig T, Klose H, Ehlken N, et al. Efficacy of exercise training in pulmonary arterial hypertension associated with congenital heart disease. Int J Cardiol 2013;168:375-81. [Crossref] [PubMed]
- Dalla Vecchia LA, Bussotti M. Exercise training in pulmonary arterial hypertension. J Thorac Dis 2018;10:508-21. [Crossref] [PubMed]
- Chan L, Chin LMK, Kennedy M, et al. Benefits of intensive treadmill exercise training on cardiorespiratory function and quality of life in patients with pulmonary hypertension. Chest 2013;143:333-43. [Crossref] [PubMed]
- Chia KS, Faux SG, Wong PK, et al. Randomised controlled trial examining the effect of an outpatient exercise training programme on haemodynamics and cardiac MR parameters of right ventricular function in patients with pulmonary arterial hypertension: the ExPAH study protocol. BMJ Open 2017;7:e014037 [Crossref] [PubMed]
- Weinstein AA, Chin LM, Keyser RE, et al. Effect of aerobic exercise training on fatigue and physical activity in patients with pulmonary arterial hypertension. Respir Med 2013;107:778-84. [Crossref] [PubMed]
- Ganderton L, Jenkins S, Gain K, et al. Short term effects of exercise training on exercise capacity and quality of life in patients with pulmonary arterial hypertension: protocol for a randomised controlled trial. BMC Pulm Med 2011;11:25. [Crossref] [PubMed]
- de Man FS, Handoko ML, Groepenhoff H, et al. Effects of exercise training in patients with idiopathic pulmonary arterial hypertension. Eur Respir J 2009;34:669-75. [Crossref] [PubMed]
- Karapolat H, Çınar ME, Tanıgör G, et al. Effects of cardiopulmonary rehabilitation on pulmonary arterial hypertension: A prospective, randomized study. Turk J Phys Med Rehabil 2019;65:278-86. [Crossref] [PubMed]
- Butāne L, Smite D, Sablinskis M, et al. Individualized home-based exercise program for idiopathic pulmonary arterial hypertension patients: a preliminary study. Cor Vasa 2019;61:e403-e410. [Crossref]
- Grünig E, Maier F, Ehlken N, et al. Exercise training in pulmonary arterial hypertension associated with connective tissue diseases. Arthritis Res Ther 2012;14:R148. [Crossref] [PubMed]
- Goto C, Higashi Y, Kimura M, et al. Effect of different intensity of exercise on endothelium-dependent vasodilation in human: Role of endothelium-dependent nitric oxide and oxidative stress. Circulation 2003;108:530-5. [Crossref] [PubMed]
- ACSM. Chapter 7: ACSM’s guidelines for exercise testing and prescription. 8ed.Lippincott Williams & Wilkins. 2010.
- Hansen D, Stevens A, Eijnde BO, et al. Endurance exercise intensity determination in the rehabilitation of coronary artery disease patients: a critical re-appraisal of current evidence. Sports Med 2012;42:11-30. [Crossref] [PubMed]
- Kemi OJ, Haram PM, Loennechen JP, et al. Moderate vs. high exercise intensity: differential effects on aerobic fitness, cardiomyocyte contractility, and endothelial function. Cardiovasc Res 2005;67:161-72. [Crossref] [PubMed]
- Hansen D, Bonné K, Alders T, et al. Exercise training intensity determination in cardiovascular rehabilitation: Should the guidelines be reconsidered?. Eur J Prev Cardiol 2019;26:1921-8. [Crossref] [PubMed]
- Rigatto K, Bós DSG, Fernandes R, et al. Only low intensity of aerobic exercise improves respiratory compliance in pulmonary hypertensive rats. J Cardiol Cardiovasc Med 2019;4:205-9. [Crossref]
- Salzman SH. The 6-min walk test: clinical and research role, technique, coding, and reimbursement. Chest 2009;135:1345-52. [Crossref] [PubMed]
- Babu AS, Holland AE, Morris NR. Exercise-based rehabilitation to improve exercise capacity and quality of life in pulmonary arterial hypertension. Phys Ther 2019;99:1126-31. [Crossref] [PubMed]
- Gilbert C, Brown MCJ, Cappelleri JC, et al. Estimating a minimally important difference in pulmonary arterial hypertension following treatment with sildenafil. Chest 2009;135:137-42. [Crossref] [PubMed]
- Guillevin L, Armstrong I, Aldrighetti R, et al. Understanding the impact of pulmonary arterial hypertension on patients’ and carers’ lives. Eur Respir Rev 2013;22:535-42. [Crossref] [PubMed]
- Gu S, Hu H, Dong H. Systematic review of health-related quality of life in patients with pulmonary arterial hypertension. Pharmacoeconomics 2016;34:751-70. [Crossref] [PubMed]
- Post MC, Mager JJ. Quality of life in pulmonary arterial hypertension. Neth Heart J 2015;23:275-7. [Crossref] [PubMed]
- Ihie F, Baezner C, Meis T, et al. Health-related quality of life in patients with pulmonary arterial hypertension. European Respiratory 2011;38:02335.
- Taichman DB, Shin J, Hud L, et al. Health-related quality of life in patients with pulmonary arterial hypertension. Respir Res 2005;6:92. [Crossref] [PubMed]
- Meñaca AM, Ines Fernandez-Cuesta Peñafiel, et al. Correlation between perceived quality of life among patients with pulmonary arterial hypertension, the 6-minute walking test and the risk stratification. European Respiratory 2019;54:PA5470.
- Reis A, Santos M, Vicente M, et al. Health-Related Quality of Life in Pulmonary Hypertension and Its Clinical Correlates: A Cross-Sectional Study. Biomed Res Int 2018;2018:3924517 [Crossref] [PubMed]
- Twiss J, McKenna S, Ganderton L, et al. Psychometric performance of the CAMPHOR and SF-36 in pulmonary hypertension. BMC Pulm Med 2013;13:45. [Crossref] [PubMed]
- Khirfan G, Naai T, Abuhalimeh B, et al. Hypoxemia in patients with idiopathic or heritable pulmonary arterial hypertension. PLoS One 2018;13:e0191869 [Crossref] [PubMed]
- Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med 2011;155:179-91. [Crossref] [PubMed]



