Acute respiratory distress syndrome in one patient with gout complicated by severe pulmonary tuberculosis: report of one case and literature review
Introduction
The prevalence of tuberculosis (TB) infection has increased in recent years. Meanwhile, due to reasons including the presence of concomitant chronic diseases and immune dysfunction and the irregular application of anti-TB therapies, an increasing number of atypical and severe TB infection cases have been reported. Recently, a patient who had received long-term analgesic and hormone-based therapies for his gout was admitted in our hospital due to dyspnea. His condition was initially diagnosed as bacterial or viral infection because of the short duration and rapid progression, but ultimately proved to be tubercle bacillus infection. The patient died 63 hrs after emergency treatment.
Case report
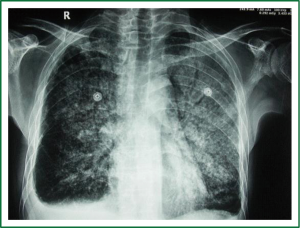
A 38-year-old male admitted to our hospital due to “fever, cough, expectoration, chest distress, and shortness of breath”. He had a history of gout and long-term irregular use of analgesic and hormonal drugs. The patient denied of any history of allergy to food or drugs. Seven days ago, the patient developed fever, cough, expectoration, chest distress and shortness of breath of no apparent cause. Four days prior to admission, the patient had a fever up to 39.5 °C at night, with thick sticky phlegm that was difficult to expectorate; meanwhile, the shortness of breath also made the patient unable to be kept in a supine position. Physical examination on admission showed body temperature 37.3 °C, heart rate 121 times/min, respiration 28 times/min, blood pressure 94/60 mmHg and blood oxygen 60%. He also had apparent orthopnea and cyanosis of the lips, symmetrical bilateral lung breath sounds, moist rales, and phlegm rales. Chest X-ray showed “diffuse bilateral lung disease, pulmonary edema?” (Figure 1). Routine blood test showed white blood cell count (WBC) 4.11×109/L, neutrophils (GRAN) 90.3%, lymphocytes (LYM) 7.33%, mono-cytes (MONO) 1.78%, Hb 127 g/L, PLT 94.6×109/L. Blood gas tests showed pH 7.27, PaO2 43 mmHg, PaCO2 42 mmHg, SO2 72.1%, oxygenation index PaO2/FIO2 86. Other findings included AST 343 U/L, CREA 91 μmol/L, CRP 201 mg/L, PCT 34.5 ng/mL, and CTNI 0.09 μg/L. After having been transferred to the intensive care unit (ICU), the patient received tracheal intubation and mechanical ventilation. Fibreoptic bronchoscopy showed a large quantity of sputum in the airway. Then the patient’s sputum specimen was sent for laboratory tests and the patient received empiric antibiotic therapy (initially piperacillin-tazobactam and then changed to imipenem-cilastatin, teicoplanin and ribavirin therapy). Twenty-four hours after admission, the disease was not improved and the transcutaneous blood oxygen was maintained at 75-80%; other measurements included CVP 20 cm H2O, CI 4.0 L/min/m2, CO 7 L/min, and SVR 747 dynes-sec-cm-5 under ventilator support (A/C, VT 350 mL, FIO2 65%, and PEEP 15 cm H2O). The patient was given pressor agents to maintain blood pressure, with a urine output <0.5 mL/kg/hr. The bedside CRRT was applied. Then, the test results were WBC 1.88×109 /L, Hb 118 g/L, PLT 66×109/L, AST 1,224 U/L, TBIL 65.5 mmol/L, hepatitis B surface antigen negative, HIV antigen negative, influenza A negative. Chest radiography was re-performed (Figure 2). Cardiac ultrasound showed AO 27 mm, PA 21mm, PAV 90 cm/S, LVPWD 9 mm, and EF 80%. Forty-eight hours after admission, the patient was in a coma, with body temperature of 36.5 °C, heart rate 140 beats/min, blood pressure 78/54 mmHg, blood oxygen undetectable. CVP 23 cm H2O, CI 2.1 L/min/m2, CO 3.4 L/min, SVR 1,809 dynes-sec-cm-5. Blood gas pH 7.26, PaO2 60 mmHg, PaCO2 51 mmHg, SO2 86%, oxgenation index 60. WBC 2.61×109/L, Hb 115 g/L, PLT 39.5×109/L. AST 1,800 U/L, CK 1044 U/L, CTNI 0.44 μg/L. Widal test and Weil-Felix Test (–), (1-3)-β-D-glucan <10 pg/mL (normal range, 0-10 pg/mL). Anti-“O” and rheumatoid factors were normal. Three consecutive sputum samples showed acid-fast bacilli. The patient was also given isoniazid, rifampicin, streptomycin and pyrazinamide as anti-TB treatment. Sadly, the patient died 63 hrs after transfer to the ICU. Sputum culture and blood culture showed no bacterial growth. The final diagnosis is severe pulmonary TB, acute respiratory distress syndrome (ARDS), and multiple organ dysfunction syndrome.

Discussion
Today, the world still faces an annual toll of 9 million new TB cases and 2 million TB deaths. According to the World Health Organization (WHO), 9.27 million new TB cases were identified in 2007, including about 1.3 million in China, secondary only to India (1). Results of the 4th National TB Epidemiological Survey in China suggested that the number of patients infected by tubercle bacillus was larger than 7.9 million (2). According to current diagnostic criteria of ARDS (3) (pulmonary exudative lesions; non-cardiogenic pulmonary edema; oxygenation index PaO2/FIO2<200), Sharma et al. (4) reported that among the 2,733 cases of TB, only 29 cases (1%) developed ARDS; in China, however, the percentage was reported to be 5% (5), indicating that cases with TB-induced ARDS infection is uncommon. It has been suggested that a history of chronic diseases, miliary TB, low lymphocyte count and liver dysfunction are high risk factors of ARDS (4). When the disease condition becomes worse and the nutritional status such as albumin and hemoglobin levels can not be well maintained, the prognosis can be poor (6). According to Sun et al. (7) the prognostic factors of death in critically ill TB patients included fungal infection (HR=3.44, 95% CI: 1.23-9.62), type II respiratory failure (HR=4.03, 95% CI: 1.56-10.38), liver damage (HR=3.96, 95% CI: 1.30-12.10), and high APACHEII score (>25) (HR=4.91, 95% CI: 1.99-12.11). In patients with delayed diagnosis and significantly deteriorating treatment, Greenaway et al. (8) found that the overall mortality rate was 12%, but reached 40-50% among those who were transferred to ICU, which was considered to be due to delayed diagnosis and treatment. A recent study has concluded that the condition of systemic organ function in ARDS (SOFA score) is correlated with a patient’ prognosis (OR 0.809, 95% CI: 0.691-0.946, P=0.008) (9). The prognosis of patients with ARDS is not only affected by high risk factors, but also related to treatment time and treatment conditions, resulting in significant discrepancies in the mortality rate of patients in corresponding studies. For instance, Agarwal et al. (10) found that among 187 ARDS patients, 9 had TB infection including 8 miliary TB; after treatment, 7 patients (78%) were cured and only 2 (22%) died. However, some other studies showed higher mortality rates. According to Erbes et al. (11), 50% of patients died in 32 days. In another case-series study, the ICU and hospital mortality rates of critically ill patients were 58% and 63%, respectively (9). In our current case, the patient had a history of gout and long-term use of analgesics and hormone-based drugs. Many studies have confirmed that the long-term use of hormones can impair the immune defense (such as T lymphocytes and macrophage function suppression) and are likely to lead to tubercle bacillus infection and spread in human tissue (12,13). It can be speculated that the patient’s disease was overlooked by himself and his family members due to the atypical infection symptoms. The patient was sent to our hospital until his condition became worse. Soon after admission, the patient developed acute respiratory distress symptoms and multiple organ dysfunction, which were not improved after potent anti-infection or TB treatment. Ultimately, all efforts to revive him were futile. The patient did not receive CT examination and his family members refused an autopsy after his death, so we are unable to further clarify whether there was an infection of extrapulmonary TB. As for critically ill patients, in addition to complex treatment combining anti-TB medication and ventilatory support, hormone treatment might be feasible for patients with severe TB (14). It has recently been reported that patients with severe TB complicated by ARDS can be rescued by extracorporeal membrane oxygenation (ECMO), but its indications and risks need further clarification (15).
Conclusions
The mortality rate of severe TB with ARDS remains high, although this condition is often neglected. Early diagnosis and treatment can help improve the prognosis. In clinical practice, infection with tubercle bacillus should be carefully excluded in pulmonary infection patients accompanied with immune dysfunction or chronic diseases. Severe patients should be consolidated with anti-TB therapy and supportive therapy and the effectiveness of hormone and ECMO treatment should be further investigated.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Global tuberculosis control: epidemiology, strategy, financing: WHO report 2009 (Publication no. WHO/HTM/TB/2009.411.). Geneva: World Health Organization, 2009.
- National Technic Steering Group Of The Epidemiological Sampling Survey For Tuberculosis, Duanmu H. Report on fourth national epidemiological sampling survey of tuberculosis. Zhonghua Jie He He Hu Xi Za Zhi 2002;25:3-7.
- Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:818-24.
- Sharma SK, Mohan A, Banga A, et al. Predictors of development and outcome in patients with acute respiratory distress syndrome due to tuberculosis. Int J Tuberc Lung Dis 2006;10:429-35.
- Zhang J, Xi X, Han F, et al. Multivariate analysis of acute respiratory distress syndrome in patients with pulmonary tuberculosis. The journal of the Chinese antituberculosis association 2008;30:48-52.
- Mehta JB, Fields CL, Byrd RP Jr, et al. Nutritional status and mortality in respiratory failure caused by tuberculosis. Tenn Med 1996;89:369-71.
- Sun J, Fang K, Ren DH, et al. A study of the prognostic factors associated with mortality in critically ill patients with tuberculous. Zhonghua Jie He He Hu Xi Za Zhi 2011;34:39-42.
- Greenaway C, Menzies D, Fanning A, et al. Delay in diagnosis among hospitalized patients with active tuberculosis--predictors and outcomes. Am J Respir Crit Care Med 2002;165:927-33.
- Lee K, Kim JH, Lee JH, et al. Acute respiratory distress syndrome caused by military tuberculosis: a multicentre survey in South Korea. Int J Tuberc Lung Dis 2011;15:1099-103.
- Agarwal R, Gupta D, Aggarwal AN, et al. Experience with ARDS caused by tuberculosis in a respiratory intensive care unit. Intensive Care Med 2005;31:1284-7.
- Erbes R, Oettel K, Raffenberg M, et al. Characteristics and outcome of patients with active pulmonary tuberculosis requiring intensive care. Eur Respir J 2006;27:1223-8.
- Targeted tuberculin testing and treatment of latent tuberculosis infection. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. This is a Joint Statement of the American Thoracic Society (ATS) and the Centers for Disease Control and Prevention (CDC). This statement was endorsed by the Council of the Infectious Diseases Society of America. (IDSA), September 1999, and the sections of this statement. Am J Respir Crit Care Med 2000;161:S221-47.
- Jick SS, Lieberman ES, Rahman MU, et al. Glucocorticoid use, other associated factors, and the risk of tuberculosis. Arthritis Rheum 2006;55:19-26.
- Kim YJ, Pack KM, Jeong E, et al. Pulmonary tuberculosis with acute respiratory failure. Eur Respir J 2008;32:1625-30.
- Mauri T, Foti G, Zanella A, et al. Long-term extracorporeal membrane oxygenation with minimal ventilator support: a new paradigm for severe ARDS? Minerva Anestesiol 2012;78:385-9.


