A randomized controlled trial evaluating airway inspection effectiveness during endobronchial ultrasound bronchoscopy
Introduction
Endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) has rapidly established itself as the first line procedure for the biopsy of mediastinal and hilar lymph nodes (1). The high diagnostic yield (2) and excellent safety profile (3,4) have established EBUS as the initial procedure of choice for the staging and diagnosis of lung cancer (5,6). A limitation of conventional endobronchial ultrasound (C-EBUS) scopes lies in their inability to provide all of the necessary functions afforded by conventional bronchoscopes during a staging bronchoscopy.
The 35-degree forward oblique viewing field on the first generation C-EBUS scopes was a design function needed to allow placement of the ultrasound transducer at the distal tip of the EBUS bronchoscope. The result of this design limits the ability to maneuver the bronchoscope compared to conventional bronchoscopes. The transducer position obstructs the user from achieving ideal maneuverability and visualization of the airway and presents an additional technical challenge for new EBUS users. This limitation, combined with a larger external diameter than most other bronchoscopes inhibits the user’s ability to perform a full airway examination and routinely requires the use of a second conventional white light bronchoscopy (WLB) for airway inspection and procedures involving sampling of the peripheral airways.
Recently, a new hybrid endobronchial ultrasound (H-EBUS) bronchoscope has been introduced which is considered a hybrid as it aims to combine the functionality of an EBUS scope with the maneuverability and high definition optics of a modern conventional bronchoscope (7). This H-EBUS scope features a 10-degree forward oblique viewing field, a narrower external insertion diameter (6.7 vs. 6.9 mm) and 130 degree flexion when compared to the C-EBUS which has a 35-degree forward oblique view and 120 degree scope head flexion (Figure 1).

We conducted a prospective randomized controlled clinical trial comparing H-EBUS to C-EBUS and the impact on performing a complete airway inspection, scope maneuverability, number of bronchoscopes used per procedure, specimen adequacy and diagnostic yield.
Methods and materials
Subjects
All patients undergoing bronchoscopy over the age of 18 involving the use of an EBUS bronchoscope in the endoscopy suite over the course of the study period were eligible for enrollment and no additional procedures were performed outside the scope of standard practice. Patients not able to safely undergo bronchoscopy as judged by the interventional pulmonary service and anesthesia were excluded. The study was performed at the Johns Hopkins Hospital and approved by the Johns Hopkins University Institutional Review Board (NA_00081049) and was registered on Clinicaltrials.gov (NCT02360306). Written informed consent was obtained prior to the enrollment and randomization of all patients.
Study design
A prospective, randomized controlled trial was performed to evaluate the differences between H-EBUS (Fujinon, Japan) and C-EBUS (Olympus, Center Valley, PA, USA) bronchoscopes for airway inspection and the diagnosis and staging of lung cancer. The primary outcome was airway segment visualization in each lobe. Secondary outcomes included the number of bronchoscopes used per procedure, procedure length, specimen adequacy (defined by the presence of lymphocytes or a definitive diagnosis) and diagnostic yield (e.g., malignancy, granuloma). Randomization of all subjects prior to bronchoscopy to either a C-EBUS group or H-EBUS groups was performed using a 1:1 random number generator. Randomization results were made available to the study personnel prior to the procedure to allow the appropriate EBUS bronchoscope to be prepared. The onsite cytotechnologist, dedicated lung pathologist and patient were blinded to scope assignment. All EBUS procedures were performed under deep sedation. A board certified anesthesiologist or certified registered nurse anesthetist (CRNA) independently assessed each patient prior to the start of the procedure and sedation was induced with Propofol prior to the placement of a laryngeal mask airway. All procedures were carried out in a single bronchoscopy suite by one of three Interventional Pulmonologists (LBY, DFK, HJL). Rapid on site cytology was available for all procedures. The EBUS scope was advanced and 1% Lidocaine was used for topical anesthesia. Prior to lymph node sampling, a full airway examination was attempted utilizing either the H-EBUS or the C-EBUS. Adequate airway examination was defined by the bronchoscopist’s ability to have clear visualization of the upper airway, vocal cords, trachea, carina and all segments of the bronchial tree. In order for an airway examination to be considered adequate it was determined a priori that there had to be independent agreement consensus between at least two bronchoscopists during the procedure. If any bronchoscopist did not feel there was adequate visualization, the exam was to be considered inadequate for that specific segment. If a full anatomic airway inspection was deemed inadequate, the EBUS scope was removed, a standard bronchoscope was introduced and a full airway examination was completed prior to initiation of the EBUS portion of the procedure. EBUS-TBNA was then performed at all clinically relevant mediastinal and hilar lymph nodes (defined as a LN >5 mm in short axis by ultrasound) using a 21 gauge needle (Olympus NA-201SX, Center Valley, PA, USA). After completion of the EBUS lymph node sampling, additional procedures, such as bronchoalveolar lavage (BAL), brushing, transbronchial biopsy (TBBx), and radial endobronchial ultrasound (R-EBUS) were performed if clinically indicated and as able with the EBUS scope. If these procedures could not be completed with the EBUS scope or visualization was not adequate, the EBUS scope was removed and the conventional bronchoscope was reintroduced to complete the sampling procedure. The number of visualized airway segments, procedure timing (total in room time and scope in/out time) and conversion rates requiring the use of a standard bronchoscope were recorded for comparison.
Statistical analysis
The primary outcome was the airway segment visualization in each lobe using an EBUS bronchoscope. Utilizing Bayesian analysis, a sample size of 30 patients per study group will provide 90% power to detect a 10% difference in airway inspection outcomes comparing the two groups. Secondary outcomes included the number of bronchoscopes used per procedure, procedure length, diagnostic yield and specimen adequacy. Descriptive statistics were used to summarize procedural characteristics using proportions for categorical variables, means ± standard deviations for normally distributed and median with interquartile range for non-normally distributed variables respectively. Unadjusted evaluation of the number of bronchoscopes used and ability to visualize airway segments comparing brands was performed using Fisher’s exact testing. Univariate analysis of cost of procedure by brand and number of scopes used was performed using logistic regression. We defined statistical significance as a two-sided P<0.05. All analyses were performed using STATA version 12 (College Station, TX, USA).
Results
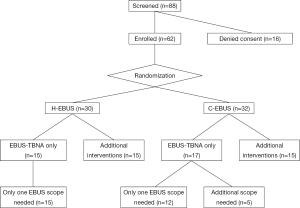
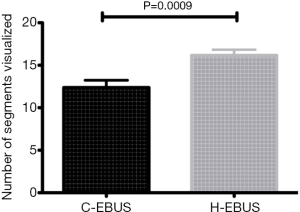
Between November 2013 and January 2014, 88 consecutive patients met inclusion criteria and were approached for consent. Sixty-two consecutive patients undergoing EBUS-TBNA as their primary procedure were consented and were randomized to H-EBUS (n=30) or C-EBUS (n=32). Sixteen patients declined enrollment in the study (Figure 2). When evaluating the ability to perform an adequate airway inspection, segmental visibility was evaluated on a per lobe basis. Overall segmental visualization was superior with the H-EBUS when compared to C-EBUS (P=0.0009) (Figure 3).
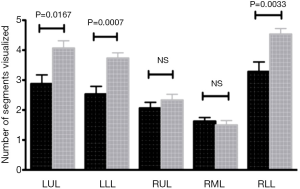
Significantly better segmental visualization was seen in the left upper, left lower, and right lower lobes (RLLs) when using H-EBUS compared to C-EBUS (P<0.01) (Figure 4). No difference in the ability to visualize segments of the right upper or middle lobes were noted (Table 1).
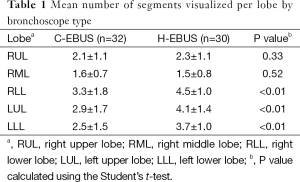
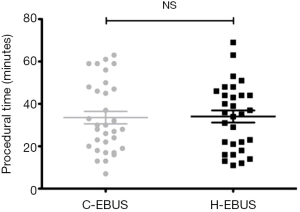
Full table
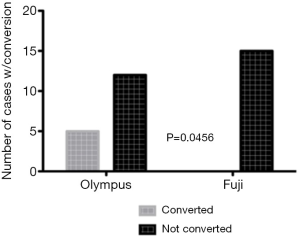
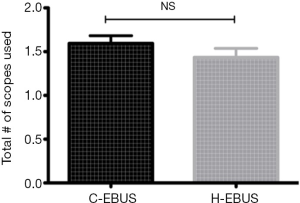
In cases in which EBUS-TBNA was the only procedure performed for staging and diagnosis (n=32, 17 C-EBUS vs. 15 H-EBUS), the need for use of a second bronchoscope to perform an adequate airway inspection was significantly higher in C-EBUS compared to H-EBUS (5 vs. 0, P=0.046) (Figure 5), however no difference in the number of bronchoscopes used per procedure was seen when including bronchoscopy during which interventions in addition to EBUS-TBNA were performed (Figure 6). There was no difference in intraobserver agreement for adequacy of airway examination. There was no difference in mean procedure length between the 2 groups (28 minutes C-EBUS vs. 25 minutes H-EBUS) P= NS (Figure 7).
Cytopathology
No difference in specimen adequacy (P=1.0) (defined as diagnostic or lymphoid material on final pathology) or diagnostic yield (P=0.725) was observed when comparing scopes for performance of lymph node TBNA with either the H-EBUS or C-EBUS bronchoscopes. Figure 8 shows the lymph nodes sampled by the two bronchoscopes. No TBNA with the conventional bronchoscope was performed during this study.
Additional procedures
Of the 62 patients who underwent EBUS-TBNA, 15 underwent procedures other than TBNA using the EBUS scopes. BAL was performed in nine patients (seven using H-EBUS and two with C-EBUS), the median instilled volume was 150 mL (IQR =105 mL) and the median return volume was 40 mL (IQR =34 mL). R-EBUS was employed in seven cases [5 H-EBUS: 2 left upper lobe (LUL), 1 right upper lobe (RUL), 1 lingula and 1 RLL; and 2 C-EBUS: 1 LUL and 1 RUL]. Of the five H-EBUS cases that employed R-EBUS, three also underwent brushing and TBBx, with adequate tissue obtained. There was no difference in intraobserver agreement for performing addition procedures. No complications were encountered.
Discussion
C-EBUS bronchoscopes have been limited to TBNA of the mediastinum, hilum and central parenchymal lesions due to low resolution optics, limited viewing angle, large outer diameter and decreased flexion of the bronchoscope when compared to standard bronchoscopes. While the C-EBUS scope has become the standard first line sampling technique for hilar and mediastinal disease (1), the need for increased procedural flexibility is highly desirable. This is the first randomized study to offer a comparison of C-EBUS and H-EBUS in patients undergoing bronchoscopy for mediastinal and hilar disease. We demonstrated that use of an H-EBUS bronchoscope was associated with improved lung segmental visualization and the use of significantly fewer bronchoscopes when performing airway inspection prior to EBUS-TBNA. Additional procedures including BAL, R-EBUS, transbronchial brushing and biopsy were shown to be feasible using the H-EBUS scope although the study was not powered to detect a difference between C-EBUS and H-EBUS in this regard.
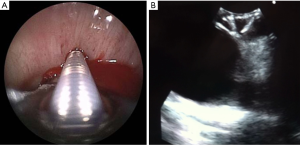
Typically; prior to performing EBUS-TBNA, a conventional bronchoscope is utilized to perform airway inspection (8). This use of multiple scopes may not only prolong the procedure, bringing with it increased costs, but may be potentially noxious to patients with multiple scope entries through the vocal cords being required. The introduction of a novel hybrid bronchoscope has shown that the performance of a full airway inspection and EBUS-TBNA is possible using a single bronchoscope. The H-EBUS bronchoscope mimics a standard bronchoscope in regards to forward visualization. This is due to a decrease in the forward oblique angle of view from 35 to 10 degrees as well as an additional 10 degrees of flexion of the scope (Figure 9). In addition, the optics of the H-EBUS scope utilizes a high definition charge coupled device (CCD) and dual light sources allowing improved imaging (Figure 10). These improvements in scope performance allowed intubation of the upper lobes when using the H-EBUS and significantly better evaluation of the LUL and lower lobes bilaterally. This resulted in a decrease in scope usage. Factors related to decreased scope usage, but not assessed in this study, include decreased need for scope turnover and maintenance which but might in fact lead to improvements in patient flow, case booking, endoscopy case volume and overall cost.

In addition to improvements in airway visualization and efficiency, the H-EBUS showed itself to be potentially capable of filling the role of a true hybrid bronchoscope. With improved airway visualization came the ability to comfortably perform other procedures typically reserved for conventional bronchoscopy. Peripheral nodule evaluation was performed using a radial EBUS probe through a 1.7 millimeter guide-sheath followed by transbronchial brushing, biopsy and BAL. However, further studies are needed to ascertain the safety and yield of H-EBUS for peripheral bronchoscopy.
While no differences in specimen adequacy or diagnostic yield were observed, a few interesting performance characteristics were noted with using the H-EBUS. The left paratracheal lymph node (station 4 L) (9), normally a more challenging nodal station to biopsy due to the difficulty in flexing the C-EBUS scope with a needle inserted, was found to be easily accessible with the H-EBUS scope as the needle takes a more perpendicular trajectory into the target lymph node with less of a need to flex the scope allowing for improved ultrasound visualization. Neither factor was the focus of this study but both issues are of potential interest for further research.
Several limitations of this study exist including performance at a single site which is a high volume center and thus results may not be generalizable. Although the study was randomized, given the design differences in EBUS bronchoscopes, proceduralists were unable to be blinded to the type of bronchoscope used. This may have led to bias in outcome measures such as visualization however the study design attempted to control for this bias by the a priori requirement that there had to be independent agreement consensus between at least two bronchoscopists during the procedure. If any bronchoscopist did not feel there was adequate visualization, the exam was to be considered inadequate for that specific segment. In addition, the study was not powered to detect a difference between types of EBUS scopes in regards to procedures other than airway inspection and TBNA. Finally, the procedures described in this study were performed using deep sedation through a laryngeal mask airway. This may limit the generalizability of the study to those centers that utilize this form of sedation rather than moderate sedation.
Conclusions
In conclusion, the novel H-EBUS scope is an effective way of both performing a thorough airway inspection and TBNA of hilar, mediastinal and proximal parenchymal lymph nodes and masses utilizing a single bronchoscope. It obviates the need for airway inspection using a conventional WLB, and is associated with decreased procedure times/ procedural costs. In addition, early data suggests that it may be able to function as a true hybrid bronchoscope in the performance of peripheral nodule location and sampling.
Acknowledgements
None.
Footnote
Conflicts of Interest: Drs. Yarmus, Akulian, Feller-Kopman, Lee and Wang have received educational grants, research grants and consulting fees from Fuji Inc. The other authors have no conflicts of interest to declare.
References
- Silvestri GA, Gould MK, Margolis ML, et al. Noninvasive staging of non-small cell lung cancer: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest 2007;132:178S-201S.
- Herth FJ, Eberhardt R, Vilmann P, et al. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax 2006;61:795-8. [PubMed]
- Asano F, Aoe M, Ohsaki Y, et al. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: a nationwide survey by the Japan Society for Respiratory Endoscopy. Respir Res 2013;14:50. [PubMed]
- Eapen GA, Shah AM, Lei X, et al. Complications, consequences, and practice patterns of endobronchial ultrasound-guided transbronchial needle aspiration: Results of the AQuIRE registry. Chest 2013;143:1044-53. [PubMed]
- Yasufuku K, Pierre A, Darling G, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg 2011;142:1393-400.e1.
- Ernst A, Anantham D, Eberhardt R, et al. Diagnosis of mediastinal adenopathy-real-time endobronchial ultrasound guided needle aspiration versus mediastinoscopy. J Thorac Oncol 2009;4:568-77. [PubMed]
- Xiang Y, Zhang F, Akulian J, et al. EBUS-TBNA by a new Fuji EBUS scope (with video). J Thorac Dis 2013;5:36-9. [PubMed]
- Nakajima T, Yasufuku K. The techniques of endobronchial ultrasound-guided transbronchial needle aspiration. Innovations (Phila) 2011;6:57-64. [PubMed]
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.