A rare case of anomalous venous drainage of the right upper lobe
Introduction
Partial anomalous pulmonary venous drainage (PAPVD) is an anomaly of pulmonary venous drainage to the systemic circulation instead of the left atrium. Usually this is a right sided anomalous vessel that drains a part of the right lung, courses anterior to the hilum and pierces the diaphragm before draining into the inferior vena cava (1). The pattern of the pulmonary vein on the chest radiograph resembles a scimitar, a type of curved sword, hence the name (2).
We present an unusual case of partial anomalous venous drainage in which the vein of the right upper lobe drains into the superior vena cava, together with the azygos vein.
Case report
A 61-year-old woman was referred to the lung surgery department because of a central tumor of the right upper lobe. Her history stated chronic obstructive pulmonary disease and a Wolff-Parkinson-White syndrome for which she received an atrioventricular reciproke tachycardia ablation. She was recently diagnosed with pneumonia and in the work-up for this pneumonia a central tumor of the right upper lobe was diagnosed. A positron emission tomography-computed tomography (PET-CT) was made and an endobronchial ultrasound was performed, showing a cT1bN0M0 tumor. Pulmonary function tests showed a forced expiratory volume in 1 second (FEV1) of 1.52 L (57% predicted), a vital capacity of 3.61 L (116% predicted) and a CO diffusion of 45% predicted. Maximal O2 uptake during exercise was 1,011 mL/min (76% predicted), with a remarkably slow increase in O2 uptake after passing the anaerobic threshold, suggestive of an impaired increase in cardiac output. Predicted post-operative VO2 max was 13 mL/kg/min after lobectomy and 8 mL/kg/min after pneumonectomy. An ultrasound of the heart was performed and did not show any ventricular or atrial septal defects.
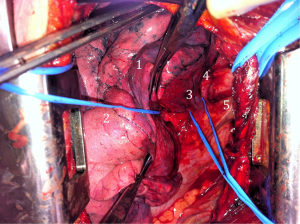
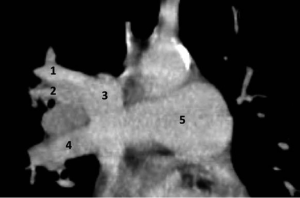
It was decided to perform a muscle sparing thoracotomy with resection of the tumor of the right upper lobe. During surgery a confluens between the azygos vein and the right upper lobe pulmonary vein draining in the superior vena cava was noted (Figure 1). Since the middle and lower lobe pulmonary veins were normally situated, a lobectomy of the right upper lobe was performed. Definitive pathology confirmed the clinical diagnosis. No further adjuvant treatment was given and recovery was without any complications. In retrospect the venous anomaly can be seen on the CT-scan, although it is not very clear (Figure 2).
Post-operatively pulmonary function tests were repeated. She was limited in her ventilatory capacity due to the chronic obstructive pulmonary disease and the lobectomy. Therefore, we were not able to see if removing the shunt improved her limitations in exercise capacity.
Discussion
Classic scimitar syndrome is a well described anomaly of total or partial right pulmonary venous drainage into the inferior vena cava instead of the left atrium. The clinical spectrum is wide. Dupuis et al. describe three forms: an infantile form associated with a large left-to-right shunt, pulmonary hypertension and significant symptoms, an adult form with a small shunt, no pulmonary hypertension and minimal symptoms and a form associated with congenital cardiac anomalies. He describes that most patients are asymptomatic and lead normal lives. Sometimes patients are slightly dyspneic at exertion (3). In the adult form pulmonary function studies show mild deficits in vital capacity and FEV1 (4). It may be associated with repeated pulmonary infections (1). In our patient, the impaired increase in O2 uptake during exercise may be caused by an impaired cardiac output due to a left-to-right shunt. It is unclear, however, to which extent this contributed to her complaints of exertional dyspnea, since the obstructive lung disease also played a role.
During embryogenesis the pulmonary venous plexus is associated with the splanchnic plexus initially. The left atrium develops an outpouching that extends to the venous plexus and becomes the pulmonary vein. The connections between the pulmonary venous plexus and the splanchnic venous plexus obliterate and the pulmonary venous plexus becomes attached to the left atrium by day 32 of the embryogenesis, leaving four pulmonary veins directly entering the left atrium. Partial or total anomalous pulmonary venous connection is due to failure of fusion of the common pulmonary vein and the primitive pulmonary plexus. The first cases were described by Cooper and Chassinat in 1836, who both described the anomaly after they discovered it during an autopsy (5,6).
We present a rare variation of partial anomalous pulmonary venous return with the azygos vein and subsequently into the superior vena cava. Such an anomaly has only rarely been described in cases of partial anomalous venous drainage of the lung. Healey recorded a large series of 147 cases of anomalous pulmonary venous return in 1952. He recorded 86 cases of partial anomalous pulmonary veins, of which only three drained in the azygos vein (7). In some of the cases described in the literature there were other anomalies, such as a patent foramen ovale, agenesis of the left lung or a one or two lobed right lung. It is important to consider the anatomic variation pre-operatively: when the partial anomalous pulmonary venous return is situated in a lobe that is not resected, a lobectomy or contralateral pneumonectomy can lead to heart failure (8).
Partial anomalous pulmonary venous return to the azygos vein is rare; we describe a case in which this is discovered during lung surgery. It can give rise to recurrent pulmonary infections and changes in the results of pulmonary function tests. Especially when discovering this by accident during lung surgery it is important to realize the anatomical relationships, so a safe resection can be performed.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gudjonsson U, Brown JW. Scimitar syndrome. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2006.56-62. [PubMed]
- Odenthal C, Sarikwal A. Anomalous unilateral single pulmonary vein versus scimitar syndrome: Comparison of two paediatric cases and a review of the literature. J Med Imaging Radiat Oncol 2012;56:247-54. [PubMed]
- Dupuis C, Charaf LA, Brevière GM, et al. The “adult” form of the scimitar syndrome. Am J Cardiol 1992;70:502-7. [PubMed]
- Schramel FM, Westermann CJ, Knaepen PJ, et al. The scimitar syndrome: clinical spectrum and surgical treatment. Eur Respir J 1995;8:196-201. [PubMed]
- Cooper G. Case of malformation of the thoracic viscera consisting of imperfect development of the right lung and transposition of the heart. London Med Gaz 1836;18:600-1.
- Chassinat R. Observations d’anomalies anatomiques remarquables de l’appareil circulatoire, avec hépatocéle congéniale, n’ayant donne lieu pendant la vie a aucun symptom particulier. Arch Gen Med 1836;11:80-4.
- Healey JE Jr. An anatomic survey of anomalous pulmonary veins: their clinical significance. J Thorac Surg 1952;23:433-44. [PubMed]
- Black MD, Shamji FM, Goldstein W, et al. Pulmonary resection and contralateral anomalous venous drainage: a lethal combination. Ann Thorac Surg 1992;53:689-91. [PubMed]


