Endoscopic intervention of lower airway foreign matter in adults—a different perspective
Introduction
Lower respiratory tract foreign bodies (FB) are more commonly encountered (75-85% of all cases) in children than in adults, with incidences peaking in those under 3 years of age (1,2). It is rare in the latter, with an estimated incidence of 0.2% to 0.33% of all bronchoscopies performed (3-5). However, bronchoscopists have encountered increasing need to remove foreign matter (FM) entering and lodging in the lower airway. This study reviews the classification of lower airway FM, emerging trends of treatment in a tertiary academic hospital, and the implication with regards to the differences in intervention compared to published literature on lower airway FB in adults.
Methods and materials
A retrospective review of patients with FM in the lower respiratory tract seen at a tertiary hospital between 1996 and 2014 was conducted following approval from the Ethics Committee and Hospital Institutional Review Board (number 2013/860/C). Hospital records including clinical, radiological, procedural and pathological charts of patients with FM from the trachea to the lungs were studied. FM is defined as any matter that has entered and lodged in the lower airway, requiring its removal by bronchoscopic intervention. Blood clots and mucus plugs that did not result in partial or complete lung collapse were excluded. The flexible bronchoscope (Olympus, Japan) was intubated either orally or via the endotracheal tube performed under topical anesthesia and moderate sedation with intravenous midazolam or propofol and fentanyl. Rigid bronchoscopy (using Bryan-Dumon bronchoscope, Bryan Corporation, USA) was performed under deep intravenous sedation allowing spontaneous respiration and assisted manual ventilation. The flexible bronchoscope was used through the rigid tube in all cases of rigid bronchoscopy. The former allowed both accessibility to the distal airway and thorough evaluation for residual FM fragment. All categorical variables are reported as counts and percentages and continuous variables are reported as means and ranges.
Results
Clinical presentation
Eighty patients (0.43%) of a total of 18,650 bronchoscopies performed over 18.5 years were identified to have lower airway FM that required intervention, Table 1. Four (5.0%) patients were treated for recurrent respiratory tract infections over 4 months to 20 years before the diagnosis of airway FM. Three-quarters of the patients had risk factors of either aspiration or iatrogenic cause for FM in the airway, Table 2. Risks for aspiration were neuromuscular dysphagia [23], encephalopathy [5], and severe facial trauma [1] from vehicular accident 20 years prior.
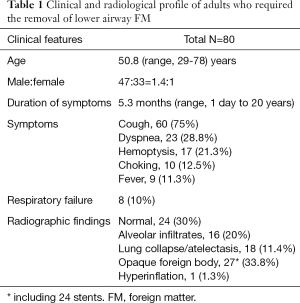
Full table
Full table
Investigations
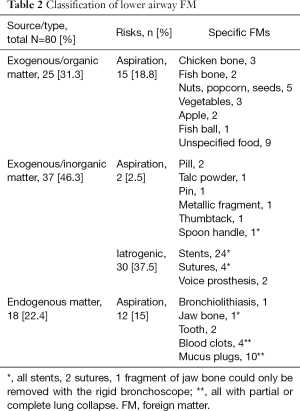
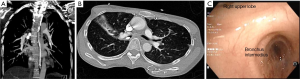
Chest X-rays (CXR) were normal (30%) or showed presence of FM (33.8%, Figure 1A) in two-thirds of the patients. Chest computed tomography (CT) scans were performed in 35% of patients and provided more information that contributed to the planning of airway intervention (Figures 1-3).

Identification of all FM was made following bronchoscopy; these can be classified into three groups, Table 2: exogenous organic (31.3%), exogenous inorganic (46.3%) and endogenous (22.4%) matter. The risk for aspiration was prevalent in about two-thirds of the patients who had either organic or endogenous matters in the airway. Iatrogenic etiology was evident in four-fifths [30] of the patients with inorganic matter of which stents [24] were the most common FM that required removal most often from tuberculous strictures [10], Tables 2,3. A total of 24 (7.0%) out of 341 stents deployed during the study period required removal. About two-thirds [15] of the stents were retrieved as they were no longer needed to maintain airway patency and the rest [9] were removed due to complications (6 stent granulomas and 3 stent migration). All stents removed were silicone stents except for four which were metallic (ultraflex) stents (Figures 2,3) (6).
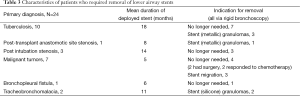
Full table
Intervention and outcome
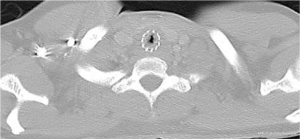
Forty-eight (60.0%) patients had FM removed via flexible bronchoscopy, with the remainder via rigid bronchoscopy. The majority of FM removed by rigid bronchoscopy (27 out of 32) could not otherwise be done with the flexible bronchoscope (Figures 1E,2,3) (6). This was primarily due to the fact that stent retrieval (in 24 of the cases) was only possible with the rigid bronchoscope. Accessory tools utilized were: grasping or biopsy forceps [51], suction [27], neodymium-doped yttrium aluminium garnet (Nd-YAG) laser [6], urokinase (2 involving blood clots) and one each for cryoapplication (removal of mucus plug), Dormia basket (tooth) and magnet extractor (pin) (Figure 1A). One patient had severe airway inflammation and stricture due to inhalation of cosmetic talc diagnosed on histological and spectral analysis of bronchial biopsy; the patient responded well to a course of oral steroids and avoidance of talc exposure. Complications during bronchoscopic retrieval of FM were: transient hypoxia [20], bleeding from granulomas (4; easily controlled with ice-cooled saline flush or Nd-YAG laser application) and severe mucosal damage from removal of metallic stents [4] (Figure 3) (6). All but four patients recovered completely from the effects of FM: two patients had significant residual airway fibrotic strictures following removal of metallic stents, one who aspirated two tablets of Domperidone (Figure 4) had complete stenosis due to fibrosis and severe malacia of the right bronchus intermedius despite repeated interval balloon dilatation, and the last patient had severe localized bronchiectasis requiring lobectomy two years after removal of a jaw fragment (Figure 1E) as a result of untreated airway actinomycosis.
Discussion
Foreign body (FB) aspiration occurs most commonly in toddlers when they explore things by putting them in their mouths (1,2). In adults, FB aspiration is uncommon and is caused mostly by the failure of airway protective mechanisms. Previous studies have classified airway FB into organic and inorganic objects (2,4,7,8). In this study, the term FM is preferred as it encompasses any matter that has entered and lodged in the lower airway from a source that maybe exogenous or endogenous to the body. This includes luminal matter requiring bronchoscopic intervention for removal, such as deployed airway stents, large blood clots and mucus plugs. Therefore, both the risk factors (74.0%) and the incidence (0.43%) of lower airway FM in adults reported here are higher than the respective figures reported by Ramos et al (44.0%) (4) and Debeljak et al. (0.2%) (3). A higher incidence of lower airway FM (0.33%) has been reported in studies (4,5) subsequent to Debeljak et al. The results here are attributed to the study being conducted in a thoracic surgery referral centre (4) and 90% of the cohort being at high risk for aspiration (5). Common organic materials inadvertently aspirated, are bones, nuts, peas, beans, seeds, vegetables and apple (4,5,9) Bone is the commonest FB retrieved in most studies (3,5,9,10) The predominance of aspirated matter has been correlated to cultural and social factors such as eating habits, customs and climate (5,7,9,10) The etiology of inorganic airway FM can either be inhalational or iatrogenic. Small objects that are placed at or in the mouths, including toothpicks, nails, screws, needles, pins, clips, caps of writing stationery and dental parts; can be unintentionally inhaled into the lower airway during sneezing, coughing or laughing. These actions require sudden deep inspiration. Al-Sarraf et al. (7) reported headscarf pin tracheobronchial aspiration as a distinct clinical entity in females who placed the pins in their mouths prior to securing their veils. As these pins are radiopaque (Figure 1A), the diagnosis is generally made earlier than for organic FB aspiration. Lower airway FM from iatrogenic source is invariably inorganic matter and has been related to tracheostomies, voice prostheses, as well as dental and bronchoscopic procedures (3,4). In this report, iatrogenic inorganic matters include sutures and voice prostheses in the first 5 years and airway stents in the subsequent years of the study period [1996-2014]. Airway stenting has become an important therapeutic option in many mechanical obstructive airway lesions. The use of more stents in the airway will concomitantly require increased removal. In this study, 7.0% of deployed stents were removed, often from benign airway lesions and also because they are no longer functional or needed in maintaining airway patency rather than as a result of stent complications. Endogenous matter lodged in the lower airway can enter the lumen either from the patient’s oral cavity (e.g., fractured facial bones due to trauma and dislocated teeth) or from the lower respiratory tract (e.g., large clots, mucus plugs, bronchiolitis) (3,10,11).
As tracheobronchial FB is uncommon and clinico-radiological presentation is nonspecific, a high index of suspicion is required (10). A history suggestive of FB aspiration is reported in up to 42% of cases and the longest retained lower airway FB before removal was 40 years (9). These FBs can result in airway obstruction via a direct physical mechanical effect and/or an indirect chemical/reactive effect, causing severe acute mucosal inflammation, granulation tissue and airway stricture which may eventually be irreversible due to fibrotic scarring and malacia. Some of these FBs, such as pills (12,13), inhalational particles (14) and vegetative matters induce chemical reactions as they disintegrate, result in severe mucosal inflammation and formation of granulation tissue within few hours following inhalation. Vegetative matters such as beans, seeds and corn can absorb water and on subsequent swelling, change partial obstruction to total, leading to atelectasis or complete lung collapse. Infection, including actinomycosis (9,15,16), endobronchitis and bronchiectasis can then ensue. Destructive irreversible bronchiectasis may develop many years after unrecognised aspiration of a FB. Post-obstructive sequelae include subcutaneous emphysema, pneumonia, abscess and empyema. One of the largest and most recent series of cases reviewed by Dong et al. (9) attributed the high incidence (79.5% of 200 cases) of FB-related complications to the delayed diagnosis by more than one month in 58% of the patients. Therefore, it is crucial to remove these FB, especially chemical matter, as soon as possible before more complications set in and retrieval becomes technically more difficult and unsafe once the FB embeds in the bronchial wall, particularly, when ‘engulfed’ by exuberant granulation tissue (5,9).
Diagnostic evaluation comprises of imaging and bronchoscopy. In the series reported by Al-Sarraf et al. (7), all aspirated headscarf pins were evident on CXR, leading directly to therapeutic bronchoscopy in the majority of cases. A third of the patients (33.8%) in this study had visible FB on CXR (with the majority of these being stents). However, about the same proportion of patients had normal CXR (30%). The CXR may remain normal in the first 24 hours and beyond in 15-25% of the cases reported (1,3-5,10,13). The absence of a radiopaque FB does not exclude the possibility of FB aspiration, even if it is a metallic object as only 7-21% of aspirated FB (in particular organic matter) is radiolucent (1,3,5,8,10). A standard radiological work-up including soft tissue neck radiograph, posteroanterior and lateral CXR should be performed in the initial diagnostic evaluation as it provides data that may lead to further imaging with CT scan and/or diagnostic bronchoscopy in the majority of cases (1,3-5). The presence of atelectasis, lung collapse, pulmonary infiltrates, bronchiectasis, air trapping and mediastinal shift on the chest radiographs may be suggestive of FB aspiration. The radiological finding of unilateral or segmental hyperaeration, due to ball-valve effect of the FB lodged in the airway, can be better seen on expiratory radiographs. Chest CT scan provides further information and aids in the planning of intervention (Figures 1-3). Bronchoscopy is frequently required for the diagnosis to be certain. When FB aspiration is not suspected clinically or the FB is absent on bronchoscopy (such as a dissolved pill), the pathologist may play an important role in making the diagnosis (12,13,17). Histological identification of the aspirated material may then be necessary for a definitive diagnosis. As an example, histological and spectral analysis of the bronchial biopsy of one patient in this study confirmed the diagnosis of inhaled cosmetic talc as the cause of bilateral severe bronchial inflammation and stricture.
In 1897, Gustav Killian performed the first bronchoscopy by removing a bone in the airway through a rigid tube (18). With clinical application of flexible bronchoscopy in 1967, the flexible bronchoscope has been the preferred instrument for the diagnosis and the removal of lower airway FB in adults (3,5,9,10,19). The rigid bronchoscope plays a complementary role to the flexible scope and is occasionally an essential therapeutic tool as the chronicity, size, and nature of the FM (Figure 1E) can render its retrieval unsafe and/or near impossible with the flexible scope (3,4,7,9). Rigid bronchoscopy, rarely followed by surgery, should then be therapeutic options (4,8,10). Despite the majority of published studies reporting the successful removal of FB with the flexible bronchoscope (at a rate of 91-97%) (3,5,9,19), this study indicated a relatively higher frequency of the rigid bronchoscope (40%) as the therapeutic instrument. This is because it is preferred to the flexible bronchoscope for the removal of large and/or sharp objects, with the majority (27 out of 32 cases reviewed) of FM removed by rigid bronchoscopy not removable using the flexible bronchoscope. It is worth noting that the retrieval of all stents [24] was only possible with the rigid bronchoscope. Silicone stents can be easily removed, but the retrieval of metallic stents deployed for more than 6 weeks is difficult and frequently results in severe mucosa injury (Figure 3) (6) with an attendant risk of transmural rupture. Due to the accessibility of rigid bronchoscopy in the study hospital, it is the preferred option when there are clear advantages such as the easier and/or safer retrieval of the FM.
Bronchoscopic intervention is primarily aimed at the removal of intraluminal lesions employing various bronchoscopic techniques. A range of accessory devices is required to retrieve FM with different characteristics in size, shape, edge, texture, consistency, and state of matter. Tools and procedures reported to be useful are grasping or biopsy forceps, wire baskets, Fogarty balloons (used to separate wired stents from mucosa), cryotherapy, Nd-YAG lasers, argon plasma coagulators, electrocautery, suction catheters, magnet extractors, snare loop catheters and fluoroscopy (1,3,4,7,9,10). The Nd-YAG laser is a versatile accessory to use, as it can ablate granulomas and release embedded FM, secure hemostasis and resect large solid matter allowing for their piecemeal removal. The retrieval of FM using the flexible bronchoscope through an endotracheal tube has the advantage of easy direct access to the lower airway, especially when repeated extubation of the scope is required for piecemeal removal of the FM or cleaning of the scope lens (3,5). It is safer to grasp the sharp end of small object through the tube (7); the larger object can then be wedged against the tip of the endotracheal tube and removed en bloc with the scope. It is therefore less likely that the FM will be dislodged at the vocal cords, pharynx, mouth and nose. However, there has been a preference in removing large or sharp object with the rigid bronchoscope in this and previous studies (7,8).
The use of thrombolytic agents on airway clots has been previously documented (20). In the current study, urokinase was administered to a large clot in the main bronchus of two patients. Mucus and blood clots can result in acute airway occlusion leading to lung collapse and the removal of such semi-solid material (including food material) containing significant amounts of water with bronchoscopic suction can be challenging. The best therapeutic tool is cryoapplication on the water-containing matter (21). The cryoprobe operates using the Joule-Thomson effect, in which a compressed gas is released at high flow and undergoes expansion. This rapidly cools the probe tip to near −80 °C within seconds and allows for the adhesion of the probe to any material containing water and retrieval of the frozen material. The advantage of the cryoprobe is that a large amount of material can be extracted during the freeze-thaw cycle.
Although none of the patients in this study required surgical removal of FM in the lower respiratory tract, it is conceivable that there will be rare instances for the need to intervene surgically (3,5,10) as the FM may be too distally or deeply embedded in the lower respiratory tract, rendering bronchoscopic removal impossible or unsafe.
Full and rapid recovery is expectant upon early mechanical removal of the FM (5,7,9,10). The cessation of inhalational exposure to minute particles and a course of steroids may suffice in rare instances. However, follow-up chest imaging and, if necessary, bronchoscopy is recommended to detect chronic complications (10,12,15). As illustrated for four patients in this study, irreversible airway destruction such as fibrotic strictures, bronchomalacia, bronchiectasis and actinomycosis are known complications even after removal of FM. Granulation is invariably present adjacent to long-standing retained FM. However, when there is exuberant tissue in the presence of aspiration of oropharyngeal content, actinomycosis must be considered and biopsy for microbiologic and histological studies should be done. Although a previous study (2) suggests resolution of granulation tissue and bronchiectasis after FB extraction, this may not occur in the presence of untreated coexisting airway actinomycosis. A prior course of antibiotics will reduced the granulation tissue, easing the removal of the FM. Conversely, the removal of FM must be followed by an adequate duration of antibiotics to avert lobectomy (10,15).
This study, like previous ones, suffers from the weakness associated with a retrospective study conducted over extended period, given that FM in the lower respiratory tract is indeed uncommon in adults. The evolving therapeutic tools developed over a long period of 18.5 years also result in the heterogeneity of lower-airway FM management. This study included FM as any matter that has entered and lodged in the lower airway requiring bronchoscopic intervention. Therefore the number of aspirated FBs [37] is much lower than reported in few larger studies (3,5,9). However, it provides the data on removal of perhaps the most common iatrogenic source of FM (stents) and endogenous matter including large obstructive clots and mucous plugs.
Conclusions
Early recognition and removal of lower airway FM is paramount in minimizing or averting complications such as airway strictures and infections. Lower airway FM encompasses not only aspirated FB but also from iatrogenic, the most common being stents for tuberculous strictures; and endogenous sources. There is an increasing indication for bronchoscopists to retrieve FM, particularly those of iatrogenic and endogenous sources, entering and lodging in the lower airway. There is likely a paradigm shift back to the use of the rigid bronchoscope in this setting. This is primarily due to the increasing need to remove airway stents with their increased deployment. When the rigid tube system is utilised more often, it will be made more accessible; this creates a tendency for the safer, easier and faster removal of FM, escalating the demand for rigid bronchoscopy. From the patients’ perspective, rigid bronchoscopy confers increased comfort, as it is performed under deep sedation. The flexible bronchoscope through the rigid tube allows accessibility to the distal airway. The armamentarium of endoscopic accessory devices has widened and tools traditionally used for tumor ablation are useful adjuncts in the retrieval of FM. In particular, the relatively cheap and safe cryosystem will allow the removal of water-containing FM, including large airway clots and mucus plugs, with greater efficiency compared to bronchoscopic suction.
Acknowledgements
The author expresses appreciation to Dr. Philip Eng who provided care and management of some of the patients in this study and Ng Heok Hee of SingHealth Academy for his writing assistance.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Goyal R, Nayar S, Gogia P, et al. Extraction of tracheobronchial foreign bodies in children and adults with rigid and flexible bronchoscopy. J Bronchology Interv Pulmonol 2012;19:35-43. [PubMed]
- Dikensoy O, Usalan C, Filiz A. Foreign body aspiration: clinical utility of flexible bronchoscopy. Postgrad Med J 2002;78:399-403. [PubMed]
- Debeljak A, Sorli J, Music E, et al. Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974-1998. Eur Respir J 1999;14:792-5. [PubMed]
- Ramos MB, Fernández-Villar A, Rivo JE, et al. Extraction of airway foreign bodies in adults: experience from 1987-2008. Interact Cardiovasc Thorac Surg 2009;9:402-5. [PubMed]
- Mise K, Jurcev Savicevic A, Pavlov N, et al. Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995-2006. Surg Endosc 2009;23:1360-4. [PubMed]
- Hsu AA. Endoscopic intervention of lower airway foreign matter in adults—a different perspective. Asvide 2015;2:127. Available online: http://www.asvide.com/articles/703
- Al-Sarraf N, Jamal-Eddine H, Khaja F, et al. Headscarf pin tracheobronchial aspiration: a distinct clinical entity. Interact Cardiovasc Thorac Surg 2009;9:187-90. [PubMed]
- Athanassiadi K, Kalavrouziotis G, Lepenos V, et al. Management of foreign bodies in the tracheobronchial tree in adults: a 10-year experience. Eur J Surg 2000;166:920-3. [PubMed]
- Dong YC, Zhou GW, Bai C, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med 2012;51:2515-9. [PubMed]
- Chen CH, Lai CL, Tsai TT, et al. Foreign body aspiration into the lower airway in Chinese adults. Chest 1997;112:129-33. [PubMed]
- Menivale F, Deslee G, Vallerand H, et al. Therapeutic Management of Broncholithiasis. Ann Thorac Surg 2005;79:1774-6. [PubMed]
- Kinsey CM, Folch E, Majid A, et al. Evaluation and Management of Pill Aspiration: Case Discussion and Review of the Literature. Chest 2013;143:1791-5. [PubMed]
- Küpeli E, Khemasuwan D, Lee P, et al. "Pills" and the air passages. Chest 2013;144:651-60. [PubMed]
- Steele AA. Suicidal death by aspiration of talcum powder. Am J Forensic Med Pathol 1990;11:316-8. [PubMed]
- Ling Hsu AA, Pena Takano AM, Wai Chan AK. Beyond removal of endobronchial foreign body. Am J Respir Crit Care Med 2014;189:996-7. [PubMed]
- Godfrey AM, Diaz-Mendoza J, Ray C, et al. Endobronchial actinomycosis after airway stenting. J Bronchology Interv Pulmonol 2012;19:315-8. [PubMed]
- Pritt B, Harmon M, Schwartz M, et al. A tale of three aspirations: foreign bodies in the airway. J Clin Pathol 2003;56:791-4. [PubMed]
- Killian G. Meeting of the Society of Physicians of Freiburg, Dec. 17, 1897. Munchen Med Wschr 1898;45:378.
- Lan RS, Lee CH, Chiang YC, et al. Use of fiberoptic bronchoscopy to retrieve bronchial foreign bodies in adults. Am Rev Respir Dis 1989;140:1734-7. [PubMed]
- Vajo Z, Parish JM. Endobronchial thrombolysis with streptokinase for airway obstruction due to blood clots. Mayo Clin Proc 1996;71:595-6. [PubMed]
- Gonzalez EL, Khosla R. Cryotherapy In The Management Of Airway Clotting In Post Coronary Artery Bypass Graft Complicated With Massive Hemoptysis. Available online: http://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A5967


