Post-operative care to promote recovery for thoracic surgical patients: a nursing perspective
Introduction
The role of thoracic nursing specialty is to support and educate patients, who are suffering from thoracic diseases, to achieve the best outcome in terms of physical, psychological, social and spiritual well beings. The care provided not only focuses on in-hospital treatments that patient received, but also encompasses the whole patient journey including lifestyle modification, health concept promotion, self-empowerment and secondary prevention. Hong Kong, as a metropolis with well-developed healthcare system, shares the same characteristics as the other developed countries. We are facing enormous fundamental challenges likes aging population, rise in medical expenses, increase in consumerism concept, etc. (1). When the patient population changes, all involved healthcare professionals, treatment strategies and caring models will be affected and should be adjusted in order to cope with the changes (2).
Over the past decades, thoracic surgical technique has been evolving in a way that surgical incision was minimized from the conventional open thoracotomy to the minimally invasive video assisted thoracoscopic surgery (VATS) and most recently to the single port VATS. Prince of Wales Hospital (PWH) is one of the four designated hospitals that provide both elective and emergency thoracic surgical services in Hong Kong. PWH is a university affiliated hospital and referral center, which provides service to the whole New Territories area with population of around 3,800,000. PWH thoracic nursing team grows together with the medical evolution; care delivery model was transformed from functional nursing to cubicle and team nursing. A few particular strategies were introduced to promote patient post-operative recovery and reduce hospital stay.
Clinical pathways
Clinical pathways, also know as clinical practice guidelines, critical pathways or integrated care pathways, are systematically developed statements that based on evidence-based practice to standardize the care processes for assisting professionals to provide the most appreciate care for a specific group of patients (3). Numerous clinical trials and studies had proven the benefits of implementing the clinical pathway, including reduction of surgical site infection (4), hospital stay and cost per admission (3,5). More importantly, the benefit attained did not cause any compromise in patient outcomes (3) and most of the implemented pathways needed no additional manpower (5).
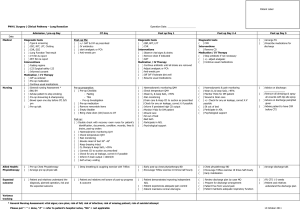
A one-paged A3 sized clinical pathway (Figure 1) had been implemented in our unit since 2011 for patients underwent lung resection surgery. This pathway was conceived and formulated by multidisciplinary teams namely medical, nursing and physiotherapy. The pathway covered patient hospital stay from pre-operative day to post-operative day 5. Interventions were clearly stated for all involved professional teams to standardize the care delivery. An expected outcome for each hospital day was also put in place to monitor patient outcome. The case nurse was responsible for ensuring the completion of the pathway every day and making remarks to those uncompleted interventions in the “Variance tracking” column. It was believed that patient would be ready to be discharged once the pathway was completed and all the “variance tracking” were followed.
Early mobilization
The benefits of early mobilization and exercise for post-operative patients were well published. It includes decrease in venous stasis, prevention of deep venous thrombosis and/or pulmonary embolism, improvement in pulmonary function and promotion of lung expansion (3) and more important, reduction in patient recovery time (6). Although it was challenging to mobilize patients receiving mechanical ventilation in the intensive care unit, early mobilization was proven to promote early extubation and reduce the length of stay (7). Early mobilization was the most effective and substantial nursing intervention in reducing post-operative complications (3). PWH nursing team established a protocol in assisting patients to sit out of bed in the early morning on the post-operative day 1 before the medical round. Sufficient manpower was crucial to ensure the established protocol to be carried out in a safe and smooth manner. Nowadays, because of the changing and expansion in nurse role, the ability and essential of the care given by supportive staffs were recognized and promoted (8). A team of supportive staffs (patient care assistants) were educated and trained, under the nurses’ supervision, they would lead and carry out the sit out process.
After thoracic operation, one or more chest tubes would be placed in the pleural cavity for hemostasis monitoring and facilitation of lung expansion. However, patient movement was bounded and walking distance was restricted to near the suction source when additional drainage force was applied to the chest drainage system. To facilitate their mobilization, two measures were implemented. First, an electronic portable chest drainage system was introduced. Patient chest tube was connected to a chargeable portable device that was able to provide and maintain preset suction force with or without connection to the power source. Patients were then able to move freely with the device mounted on a moveable drip stand; the planned treatment was thus unaffected. In addition, this portable device also provided solid electronic data of chest drainage status like the amount of air-leakage, monitored pressure value, etc. This data was useful in facilitating patient management.
The second measure was the implementation of a fast-track program “Chest drain removal by nurses”. This program was implemented in 2011 and aimed at promoting patient early mobilization and recovery. A group of experienced nurses were trained to remove chest tube independently and safely under the preset protocol. The training program consisted of classroom lecture, technique demonstration, stimulation training, clinical supervision and practical assessment. Nurses were required to pass the practical assessment by an in-charge cardiothoracic surgeon and a cardiothoracic nurse specialist in order to get the qualification. The training program was carried out every 3 years for assessing and upholding the competency of those qualified nurses. An audit was conducted right after the program implementation and revealed that the post chest tube removal complication rate was similar to those of doctors. Promisingly, the average time from order to removal was greatly shortened from 7 hours (by doctors) to 2 hours (by nurses). Currently, over half of the nurses of the PWH thoracic nursing team are qualified and over 80% of the chest tubes were removed by them. It is believed that the early removal of chest tube would promote patient early mobilization.
Staff training and clinical audit
Complication monitoring is one of the major nursing interventions for post-operative thoracic patients. Complications include post-operative bleeding, broncho-pleural fistula, persistent air-leakage, wound infection, etc. Failure in early detection or monitoring might result in irreversible and tremendous consequences. Post-operative complications became the most paramount factor that affected patient recovery. Repetitive education and training were able to remove barriers of individuals, unite their direction and facilitate the implementation of clinical initiatives and protocols (7). Continuous specialty training was one of the essential elements in maintaining nurses’ surveillance awareness and alertness. Unfortunately, the number of available specialty training program was far beyond the actual demand, resulting in insufficient certified nurses working in that particular specialty (9).
In PWH thoracic nursing team, only approximately two fifth of nurses were equipped with cardiothoracic specialty qualification. In order to improve the above situation and fill in the gap between the clinical need and training opportunity, PWH nursing team formulated its own in-house training program. Teaching topics were prioritized with respect to practical importance and clinical utilization regularity, e.g., chest drain management, blood gas interpretation and bedside bronchoscopy care were categorized higher. The decided topics were taught by experienced nurses or doctors. Stimulation training and hand-on workshop were arranged to enhance future applicability in particular to the topics with practical importance.
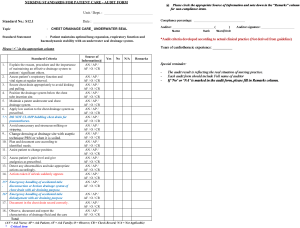
Furthermore, a clinical audit form (Figure 2) was developed together with the training program. Clinical audit was defined as “a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change” (10). The developed clinical audit form was intervention-orientated and was used to assess the program effectiveness in terms of particular nursing intervention. Besides program effectiveness, audits were also used to look for any change in clinical outcome by carrying it out before and after the program. Proper utilization of clinical audit could review current practice, identify potential threats, implement positive changes and confirm improvement.
It is believed that the tailor made staff training program with corresponding clinical audit can train up nurses with knowledge and practical skills, but also increase nurses’ awareness and alertness in complication monitoring, suggest clinical potential improvement area and provide continuous outcome monitoring.
Future advancement and development
The care planning approaches were shifted from practitioner-centered to patient-centered (11), it was a common practice to adopt the patient-orientated evidence-based practice in the clinical areas nowadays. Most of the patient-orientated evidence-based practice only focused on physical outcomes, but not the patients’ psychological needs. For example, cancer treatment side effects and emotional distress always accompany one another. However, the psychological and emotional needs of those patients suffering from cancer were seldom being cared (12). Patient-centered care composed of three fundamental elements: (I) addressing individual patients’ perspective and needs; (II) empowering patients by involving them in the care planning and; (III) establishing a patient-clinician relationship (13).
Based on the existing healthcare system and care planning strategies, patients’ need might not be holistically addressed. For example, the above-mentioned clinical pathway did not consider the patients’ individual need during the preparatory setup. In addition, there was no proper channel for patients to initiate communication with the respective healthcare team and express their own opinions and concerns. It was a one-way communication. On the other hand, patient support group seemed to be an alternative to provide better communication access. Surely it will be useful for the patients to learn about other patients suffering from the same illness, where they could meet and support each others. Unfortunately and interestingly, the actual participation rate was lower than expected despite of the potential benefit (14). And also, patient support group was seldom being invited to participate in the patient care planning process. In general, channel for patient-clinician communication was not adequate and not easy to access. Introduction of nursing case manager might become one of the solutions.
Case management is defined as a “collaborative process which assesses, plans, implements, coordinates, monitors, and evaluates options and services to meet an individual’s health needs through communications and available resources to promote quality cost-effective outcomes” (15). The definition of case management echoes with the nursing process with assessment, planning, implementation and evaluation, wherein nurses knew well since their first day in nursing study. Moreover, as the insider of the healthcare system, nurses understand well about the culture and infrastructure of the organization, in which could facilitate them to coordinate care and collaborate with other professional teams. It intuitively make nurses became the most suitable person to work as the patient case manager.
Nursing case managers assess patients by using in-person interview, this provides accessible channel for patients to participate in the care planning process. Patients’ individual needs in the physical, psychological and social aspects would thereby able be addressed and all the information acquired by the nurse managers could be used to drive the change for improving the planned treatments and also the patient-clinician relationship (3). Besides patient assessment and according to the patients’ identified needs, nurse managers would also assess the health system for locating any available resources (16) that would be able to deliver the most suitable interventions to them. Nurse managers were responsible for the care planning and implementation of the planned care to patients by coordination and collaboration with healthcare professional teams. They also advocated patients to pursuit healthier lifestyle by solving the health problems and promoting secondary disease prevention (17). Nurse managers monitored and evaluated the care given according to the preset goals and made adjustments when necessary.
Nursing case management approach gathered the opinions from the patients and used it in the care management plan. Together with the clinical pathway, a more comprehensive and holistic care service can be provided. Fragmented and unorganized care delivery will then be reduced where unnecessary hospital stay and admission could also be prevented as reported by previous study (5). Nursing case management model was proven, in particular patient population, to have significantly lower the total cost per patient but the care quality was maintained or even improved (5,18,19). Moreover, since the actual patients’ needs were identified and the care planning was customized, the staffing need was better estimated without any wastage (20).
Patients with thoracic neoplasm had multifaceted concerns including selection of medical therapy, side effects of treatment received, potential disease recurrent, quality of life, emotional distress, family issues, etc., in which causing enormous disturbance on patients’ physical, psychological and social aspects. As nursing case management approach could address and take care all patient concerns, it was most suitable for this group of patients. It is believed that the implementation of nursing case management is a three-win situation that health organization resources could be effectively utilized; patients received patient-centered care with better outcomes and nurses gained autonomy and job satisfaction.
Conclusions
Nowadays, healthcare system is facing numerous challenges due to aging population, medical technique advancement and rise of consumerism. Surgical technique and treatment strategies for thoracic surgical patients continue to evolve. Nurses, as one of the pivotal members of the healthcare teams, need to grow and go forward together as well. Thoracic nursing team works closely together with other healthcare professionals and provides quality care to patients suffering from thoracic diseases. Nursing case management was proven to be a cost-effective approach in providing holistic care, especially for patients suffering from thoracic neoplasm. Despite of the advance development in medical treatment strategies and nursing management approaches, post-operative nursing interventions including complication monitoring, early mobilization, etc. remain the most important and essential care to ensure early and complication-free rehabilitation. Not to forget, continuous specialty training and clinical audit are the keys to maintain and uphold the standard of quality care provided.
Acknowledgements
The author wishes to acknowledge the PWH Cardiothoracic nursing team led by Mr. Daniel Ng for the development of clinical pathway and the implementation of clinical audit.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Food & Health Bureau, Hong Kong Special Administrative Region. “Your Health Your Life”. Healthcare Reform Consultation Document 2008. Available online: . Assessed 2 September 2015.http://www.fhb.gov.hk/beStrong/files/consultation/Condochealth_full_eng.pdf
- Riley C, Poss WB, Wheeler DS. The evolving model of pediatric critical care delivery in North America. Pediatr Clin North Am 2013;60:545-62. [PubMed]
- Morris BA, Benetti M, Marro H, et al. Clinical practice guidelines for early mobilization hours after surgery. Orthop Nurs 2010;29:290-316. [PubMed]
- Trussell J, Gerkin R, Coates B, et al. Impact of a patient care pathway protocol on surgical site infection rates in cardiothoracic surgery patients. Am J Surg 2008;196:883-9. [PubMed]
- Wayman C. Hospital-based nursing case management: role clarification. Nurs Case Manag 1999;4:236-41. [PubMed]
- Lee TG, Kang SB, Kim DW, et al. Comparison of early mobilization and diet rehabilitation program with conventional care after laparoscopic colon surgery: a prospective randomized controlled trial. Dis Colon Rectum 2011;54:21-8. [PubMed]
- Castro E, Turcinovic M, Platz J, et al. Early Mobilization: Changing the Mindset. Crit Care Nurse 2015;35:e1-5. [PubMed]
- Kahn BA. The evolution of orthopaedic nursing at the Hospital for Special Surgery: the first orthopaedic institution in the United States. Orthop Nurs 2005;24:343-8. [PubMed]
- Watman R, Escobedo M, Langston CA. The Hartford Geriatric Nursing Initiative: developing a focused strategy and strong partnerships to improve nursing care for older adults. Nurs Outlook 2011;59:182-7. [PubMed]
- National Institute for Clinical Excellence. Principles for Best Practice in Clinical Audit 2002. Available online: http://www.uhbristol.nhs.uk/files/nhs-ubht/best_practice_clinical_audit.pdf. Accessed 26 September 2015.
- Dale AE. Determining guiding principle for evidence-based practice. Nurs Stand 2006;20:41-6. [PubMed]
- Arora NK. Importance of patient-centered care in enhancing patient well-being: a cancer survivor’s perspective. Qual Life Res 2009;18:1-4. [PubMed]
- Belkora JK, Loth MK, Volz S, et al. Implementing decision and communication aids to facilitate patient-centered care in breast cancer: a case study. Patient Educ Couns 2009;77:360-8. [PubMed]
- Quin J, Stams V, Phelps B, et al. Interest in internet lung cancer support among rural cardiothoracic patients. J Surg Res 2010;160:35-9. [PubMed]
- Taylor P. Comprehensive nursing case management. An advanced practice model. Nurs Case Manag 1999;4:2-10. [PubMed]
- Goodwin BA. Home cardiac rehabilitation for congestive heart failure: a nursing case management approach. Rehabil Nurs 1999;24:143-7. [PubMed]
- Baker CM, Miller I, Stitterding M, et al. Acute stroke patients comparing outcomes with and without case management. Nurs Case Manag 1998;3:196-203. [PubMed]
- Morrison RS, Beckworth V. Outcomes for patients with congestive heart failure in a nursing case management model. Nurs Case Manag 1998;3:108-14. [PubMed]
- Baldwin KM, Black D, Hammond S. Developing a rural transitional care community case management program using clinical nurse specialists. Clin Nurse Spec 2014;28:147-55. [PubMed]
- Moore M, Hastings C. The evolution of an ambulatory nursing intensity system: measuring nursing workload in a day hospital setting. J Nurs Adm 2006;36:241-8. [PubMed]


