Evolution of transbronchial needle aspiration technique
Introduction
Transbronchial needle aspiration (TBNA) has been utilized for 30 years and there was renewed interest in utilizing it in conjunction with endobronchial ultrasound [endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA)] in some areas recently. TBNA through flexible bronchoscope was first introduced in 1983 (1,2), and described with details by Wang et al. 1 year later for specimen sampling in the diagnosis of mediastinal adenopathy and peripheral pulmonary nodules (3). Chest CT and endobronchial landmarks are utilized to select the appropriate puncture site during the conventional TBNA (cTBNA), while ultrasound is used to detect and guide sampling the target such as lymph node or mass, outside the bronchial wall during EBUS-TBNA. Both cTBNA and EBUS-TBNA have unique advantages and disadvantages. Studies have suggested that the utilization of endobronchial ultrasound could improve the overall sensitivity of TBNA to some extent, and EBUS-TBNA might further improve the diagnostic yield. However, EBUS needle is unnecessarily complicated and difficult to use. Besides the high cost, EBUS equipment is also harder to obtain in clinical settings than regular flexible bronchoscope. EBUS-TBNA procedure usually requires general anesthesia or deep sedation with laryngeal mask airway (LMA) or endotracheal tube in order to have a satisfied operation process in many institutions. Therefore, compared with EBUS-TBNA, cTBNA was used much more broadly around the world especially in the developing and undeveloped countries. In order to further improve the TBNA technique, we briefly discuss the evolution of TBNA techniques in recent years.
Traditional techniques of TBNA (4,5)
Traditionally, there are four core techniques to aid the bronchoscopist during TBNA, namely the jabbing technique, pushing technique, hub against the wall technique, and cough technique. In the following sections, we highlight the important aspects of each method.
Jabbing technique (Figure 1)
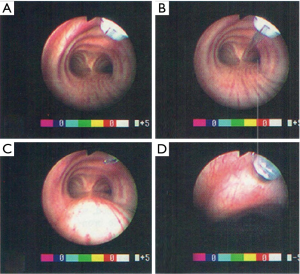
The bronchoscope should be positioned vertically in the middle of trachea with the distal tip located in the center of the trachea. With the bevel of the needle inside the metal hub, the bronchoscopist advances the outer catheter via the working channel until the distal metal hub is visualized at the end of the bronchoscope (Figure 1A). Once the distal metal hub is visualized, the needle is advanced and locked in place (Figure 1B). Then, the catheter is retracted until only the needle tip is clearly visible (Figure 1C) and the bronchoscope and needle are advanced as one unit toward the intended puncture site. With the puncture site in view, the bronchoscopist can use the thumb to press down the operating lever of the bronchoscope, so it is perpendicular to the tracheal wall. Then, the tip of needle is inserted into the tracheal mucosa at the intended puncture site and the assistant is requested to hold the proximal end of the bronchoscope stationary at the level of nose or mouth. The bronchoscopist rapidly jabs the needle catheter approximately 1–2 cm into the opening of the working channel with the thumb and index finger of right hand until the needle is completely penetrated into the airway wall; the needle hub is against the surface of the mucosa (Figure 1D). Once the needle penetration is confirmed, a continuous suction is applied, during which the needle is agitated or pushed back and forth several times.
The caution notes for the jabbing technique are as follows: (I) confirm the tip of needle has been withdrawn into the metal hub before it is inserted into the bronchoscopic working channel. The needle tip should not be protruded out of the metal hub, or withdrawn proximal to the metal hub, to avoid the damage of working channel of the bronchoscope; (II) orients the scope tip perpendicular to the bronchial wall of the puncture site as much as possible; (III) during the jabbing process, the assistant should hold bronchoscope at the level of the nose or mouth; (IV) avoid pushing the needle with the catheter out of the scope too long during the process, which will lose its force and make it more difficult to confirm whether the needle has completely penetrated the bronchial wall.
Pushing technique (Figure 2)
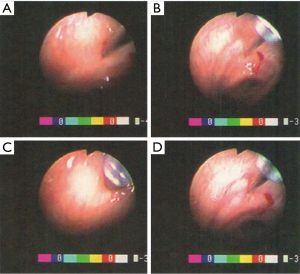
The bronchoscope should be positioned in the middle of trachea with the distal tip located in the center of the trachea. With the bevel of the needle inside the distal metal hub, the bronchoscopist advances the needle system via the working channel of bronchoscope, until the metal hub is visualized at the distal tip of the bronchoscope, then protrudes the needle and locks it in place (Figure 1A-C). The operating lever of the bronchoscope can be pressed down with left thumb and adjusted to orient the puncture path perpendicular to the airway wall as mentioned above. With the tip of needle embedded and fixed into the mucosa of the intended puncture site (Figure 2A), the bronchoscopist advances the out catheter till only the metal hub is visible (Figure 2B), and fixes the proximal end of the outer catheter at the entrance of the bronchoscopic working channel. The needle system could be locked to the body of the bronchoscope by hooking with the small finger (digitus minimus) of the left hand or through the iron head fixator. Then the needle and bronchoscope are advanced as one unit to puncture the identified target site (Figure 2C). Once the needle completely penetrates into the bronchial wall, continuous suction is applied and the needles together with the scope are moved back and forth several times rapidly. After the puncture movement is finished, the needle system is retracted out of the bronchial wall and scope (Figure 2D).
When the bronchoscopist uses a core histology needle, such as a dual core biopsy needle (MW-319, ConMed, Utica, NY), a pushing technique is often needed. As mentioned above, the needle’s out catheter is inserted through the working channel until the metal hub is visualized (Figure 3A). The assistant will then push and lock the needle assembly that includes the inner 21-gauage (21-Ga) needle and the outer 19-Ga core biopsy needle. Both needles will be protruded out and ready for puncture (Figure 3B). The catheter and bronchoscope are then advanced until the tip of the dual 21-Ga/19-Ga needle embedded in the mucosa (Figure 3C). The scope and needle are then forcefully advanced with pushing technique until the needles penetrate through the bronchial wall completely (Figure 3D). Then suction is applied, the inner 21-Ga needle is retracted, the outer 19-Ga core biopsy needle is moved back and force with scope to sample lesions for histology specimens.
The caution notes for pushing technique include: (I) in the pushing process, the needle assembly should be fixed at the proximal entrance of the working channel as one unit with scope to avoid sliding when the needle’s tip encounters resistance; (II) maintain visualization of the distal metal hub during the pushing process; (III) jabbing technique can be simultaneously applied during pushing process to facilitate the satisfied penetration.
Hub against the wall technique
As described above, after advance the needle into the bronchoscopic working channel once the metal hub is visualized in the airway, the bronchoscopist moves the bronchoscope towards the intended puncture site, places and fixes the metal hub against the airway wall. Then, the assistant will protrude and lock the needle in place. If the needle does not completely penetrate through the wall, the jabbing or pushing technique may be employed to assist with penetration.
The caution notes for hub against the wall technique are: (I) carefully maintain the position of the hub because its smooth surface may allow the hub to slide on the airway wall prior to puncture; (II) the needle tip should not be withdrawn too deep into the metal hub, otherwise, the outer catheter and working channel of the bronchoscope will be penetrated and damaged when the needle is protruded.
Cough technique
This may be used adjunctive to either the jabbing or pushing technique, during which the bronchoscopist asks the patient to cough intentionally. The coughing technique is helpful not only for puncturing, but also for maintaining a clear bronchoscopic vision.
Combination of multiple puncture techniques
When resistance is encountered during the puncturing process, the bronchoscopist should first determine whether the path is correct or penetration is through an inter-cartilaginous space. If the puncture is obstructed by cartilage, the needle should be repositioned to avoid penetrating through a cartilaginous ring. The lesion itself and a core needle with a larger diameter are other contributing factors for a difficulty penetration. A combination of multiple puncture techniques is often needed in such a situation. For example, if the jabbing technique alone is not successful, it may be supplemented by the pushing or cough technique, to facilitate the penetration.
Methods and techniques of EBUS-TBNA
In recent years, EBUS-TBNA has been utilized to help augment the technique of cTBNA. The external diameter of the EBUS bronchoscope is larger than that of the regular bronchoscope with the visual angle. Currently different EBUS scopes have different viewing and needle exit angle, compared with standard bronchoscopes. In addition, the needle angles of Olympus EBUS and Pentax EBUS scopes are 35 and 45 degrees respectively, with their visual angles consistent with the puncture needle angles. The puncture needle angle of Fuji bronchoscope is between 35 and 45 degrees, however, its visual angle is only 10 degrees, which makes it more easily to be used as a standard bronchoscope. The visual angles of the EBUS scopes and larger external diameter also make them more difficult to go through the vocal cords.
The basic procedures and techniques of EBUS-TBNA have been described previously (5). The bronchoscopist inserts the scope into the trachea and advances the tip of the scope to the planned target as identified by CT and/or the WANG lymph node map. Then, position the endoscopic tip to contact the airway wall and generate an ultrasonic image to obtain target. The optimal ultrasound image may be facilitated by inflating the balloon to improve the contact of probe and bronchial wall. When the appropriate puncture site is confirmed, the scope is straightened to allow the needle assembly to pass through the working channel. With the outer catheter advanced through the working channel, the bronchoscopist can lock the needle assembly proximal to the bronchoscope. Then after determine the depth of the penetration (generally 2 cm), the bronchoscopist adjusts and fixes the distal tip of the needle catheter in the working channel, followed by flexing the distal tip of the scope to retrieve the ultrasound image of the target site, and release the needle fixator and force the needle penetrated through the lesion. It is of note that this technique is modeled after the previously described hub against wall technique for cTBNA. With the needle positioned in the target confirmed by the ultrasound, the stylet is retracted and followed with suction. The needle is then pulled back and forth several times rapidly with the jabbing technique. When the punctures are completed, the bronchoscopist withdraws the needle into the working channel of the needle and, removes the whole needle assembly from the working channel of the scope and blows the specimens onto a slide or into the liquid for further examination. The stylet is also used to push specimens out of the needle to keep the catheter unblocked.
The caution notes for EBUS-TBNA technique are: (I) for EBUS-TBNA, the bronchoscopists need to learn how to recognize and interpret ultrasound images of different lymph nodes accurately. It also needs to be emphasized that currently real-time endobronchial ultrasound images are displayed upside-down, which is like ultrasound imaging of cardiac or gastrointestinal systems. No satisfactory results could be obtained without adequate training. What’s more, the incorrect use of instruments can increase the risk of complications (6-8). Adequate training is critical prior to clinical application; (II) comparing to regular bronchoscopy, EBUS-TBNA procedure requires deeper anesthesia. General anesthesia is helpful; especially for beginners; (III) we should also pay attention to the prevention of severe complications, such as mediastinitis or abscess; (IV) the mastery of cTBNA technique is very helpful for EBUS-TBNA procedure. In particular, it should be appreciated that the fundamental techniques of cTBNA and EBUS-TBNA are exactly the same except the outer catheter is pushed with the needle already protruded and locked in place during cTBNA procedure, whereas in EBUS-TBNA procedure, the needle is unlocked; (V) besides less availability of EBUS equipment than standard flexible bronchoscopies, the much higher cost of EBUS-TBNA procedure, compared to cTBNA, also limits the broader application of EBUS in some areas. The advantages and disadvantages of EBUS-TBNA and cTBNA should be carefully evaluated when they are applied; (VI) it is not recommended to retract the stylet into the needle lumen before the initial puncture, or push it back into the lesion repeatedly after a successful puncture, which may increase the risk of mediastinitis, pericarditis, pneumonia, pulmonary cyst infection, or sepsis (9-11). Especially for those with an immune deficiency disease or cyst.
Update of cTBNA technique in recent years
Needle tip against the wall technique
With the hub against wall technique, the needle tip is invisible during its penetration through the bronchial wall. Moreover, the smooth apex of the metal hub may be difficult to be fixed at the selected puncture site. Therefore, during our practice, we have adapted the needle tip against the wall technique as follows. The initial operation is similar to that of the hub against the wall technique; however, we minimally advance the needle tip out of metal hub of the needle catheter before placing the metal hub against the targeted puncture site, and then embed the needle tip in the mucosa, which aids in hub fixation. Finally, we fully protrude the needle with force and rapidly lock it in place till the needle completely penetrates into lesions. This method has proven to be more successful and safer by combining with the jabbing technique, and avoiding the disadvantages of the hub against the wall technique.
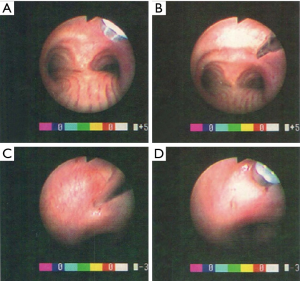
Iron head fixator technique
Both jabbing technique and pushing technique have limitations. The common reason that the needle cannot penetrate into the bronchial wall completely during the jabbing technique, is that the locked needle with its catheter is out of the tip of the scope too far, which greatly decreases its penetration strength and finally leads to the failure of cTBNA procedure. Another important reason for unsuccessful cTBNA procedure using pushing technique is failing to fix the needle catheter system with the scope as one unit during the process. To avoid these common mistakes and to increase the successful puncture ratio of jabbing or pushing technique, we introduced the iron head fixator in our practice. It could prevent the needle catheter from protruding too long or sliding back into the scope lumen, thus, ensure the best puncture angle and depth.
The iron head fixator technique is briefly illustrated as follows (Figure 4). When the metal hub is visualized, the bronchoscopist screws the rotary knob of iron head fixator in clockwise and fixes the needle’s outer catheter. Then, the needle’s movement is tested to ensure that it is able to advance and retract without restriction. If the needle cannot advance easily, the bronchoscopist can marginally loosen the fixator until the needle is free to move but the catheter remains locked. Then the bronchoscopist advances the bronchoscope toward the target puncture site only with the tip of the needle visualized. Once the needle reaches the target puncture site, it is protruded and locked, and then penetrates into the lesions with the pushing technique. The fixator could also be used during cTBNA with regular pushing technique. The bronchoscopist fixes the needle catheter with fixator when the locked needle and the metal hub are in view. Then the scope is pushed to force the needle penetrates through the bronchial wall. After obtaining specimens, the bronchoscopist pulls the needle out of the airway wall, retracts it into the metal hub, after unscrews the rotary knob of the iron head fixator, then takes the whole needle system out of the scope and prepares the specimens for pathology examination.
The iron head fixator technique can prevent the puncture failure due to unsatisfied fixation of the needle catheter to bronchoscope during pushing technique or the over extension of the needle catheter during jabbing technique. From our experiences, a much more stable and reliable result could be achieved with this simple and convenient technique without adding any extra equipment. It is worthy considering especially among the inexperienced operators.
The caution notes for iron head fixator technique are: (I) when fixing the needle’s out catheter, the iron rotary knob should not be screwed too tight since it may fix the inner catheter system accidently; (II) it is important to screw the iron head fixator counterclockwise to release the needle system completely before retracting it from the bronchoscope. This will avoid any stretching of the outer catheter due to the friction between catheter and fixator during withdrawal, which may influence the next puncture.
Advance of EBUS-TBNA techniques in recent years
Different EBUS lenses with charge coupled devices (CCD) have different visual (field of view) angles as well as angles at which the needle will exit the working channel. Thus, different EBUS equipment system requires different TBNA needles and techniques. The efforts to achieve better clinical results and broader application of TBNA techniques have been largely absent but become increasingly important. On one hand, EBUS-TBNA itself is constantly adopted through training in both conventional and ultrasound techniques. On the other hand, companies are also making continuous improvements in the EBUS bronchoscope, as well as, the EBUS needles in recent years. For example, needle 5 (DT company, Changzhou, China) specially adapted to EBUS has been developed and used in China. The development of DT-522 needle made by nitinol will be accomplished and the product is expected to become available clinically in the near future. The project to improve the design of needle exit angle of Fuji scope is also ongoing.
Clinical applications
In clinical practice, which method or technique should be chosen in different conditions often depends on the bronchoscopists’ skills and clinical experiences. Generally, bronchoscopists combine various techniques in practice to achieve the best results. Their experience from relevant training and practice is the most important factor for a successful TBNA procedure. As with most tools, the best way to master it is to use it.
With the tip of outer catheter or metal hub in view (Figure 4), the bronchoscopist fixes the outer catheter by turning the fixator clockwise to tighten.
Prospect
Although with 30 years history, cTBNA is still not included in the clinical staging of lung cancer. However, EBUS-TBNA, with only 10 years of application, has been applied to the TNM staging of lung cancer in 2009, due to its more consistent performance than cTBNA. Nevertheless, considering the economic benefits, medical costs, developmental potential and the sustainability, the training and application of cTBNA are still very important. cTBNA, as a basic technique, plays an important role in a successful navigation bronchoscopy examination or EBUS-TBNA procedure. At any time, we should not do it as necessary just because we could do it. While medical science and technologies will advance for better diagnosis and treatment, the basic technique like cTBNA still has an irreplaceable role in clinical practice. We should strengthen training for both cTBNA and EBUS-TBNA in the future to achieve successful applications of these complementary techniques.
Acknowledgements
All authors greatly appreciate Dr. Turner JF, Department of Medicine, Division of Pulmonary and Critical Care Medicine, University of Tennessee School of Medicine, Knoxville, TN, for critically editing of the manuscript.
Funding: This study was supported by Critical R&D Project of Shandong Province, 2015 (2015GSF118184).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wang KP, Terry PB. Transbronchial needle aspiration in the diagnosis and staging of bronchogenic carcinoma. Am Rev Respir Dis 1983;127:344-7. [PubMed]
- Wang KP, Brower R, Haponik EF, et al. Flexible transbronchial needle aspiration for staging of bronchogenic carcinoma. Chest 1983;84:571-6. [PubMed]
- Wang KP, Haponik EF, Britt EJ, et al. Transbronchial needle aspiration of peripheral pulmonary nodules. Chest 1984;86:819-23. [PubMed]
- Wang KP. Transbronchial needle aspiration: How I do it. J Bronchol 1994;1:63-8. [PubMed]
- Mehta AC, Wang KP. Teaching conventional transbronchial needle aspiration. A continuum. Ann Am Thorac Soc 2013;10:685-9. [PubMed]
- Fernández-Villar A, Leiro-Fernández V, Botana-Rial M, et al. The endobronchial ultrasound-guided transbronchial needle biopsy learning curve for mediastinal and hilar lymph node diagnosis. Chest 2012;141:278-9. [PubMed]
- Medford AR. Learning curve for endobronchial ultrasound-guided transbronchial needle aspiration. Chest 2012;141:1643; author reply 1643-4. [PubMed]
- Jantz MA, McGaghie WC. It's time for a STAT assessment of bronchoscopy skills: the endobronchial ultrasound bronchoscopy (EBUS)-STAT and EBUS-transbronchial needle aspiration skill evaluation. Am J Respir Crit Care Med 2012;186:703-5. [PubMed]
- Fukunaga K, Kawashima S, Seto R, et al. Mediastinitis and pericarditis after endobronchial ultrasound-guided transbronchial needle aspiration. Respirol Case Rep 2015;3:16-8. [PubMed]
- Asano F, Aoe M, Ohsaki Y, et al. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: a nationwide survey by the Japan Society for Respiratory Endoscopy. Respir Res 2013;14:50. [PubMed]
- Haas AR. Infectious complications from full extension endobronchial ultrasound transbronchial needle aspiration. Eur Respir J 2009;33:935-8. [PubMed]



