Early severe mediastinal bleeding after esophagectomy: a potentially lethal complication
Introduction
Thoracolaparoscopic esophagectomy has a high morbidity and mortality (1). One of the most common complications is anastomotic leakage. The incidence of this complication has a wide range and it is thought to be responsible for up to 40% of the post-operative deaths after esophagectomy (2). Mediastinitis occurs in 9% of cases even after cervical oesophagogastrostomy (3). Adequate surgical drainage of the mediastinum in combination with antibiotics is the most important treatment. The role of expandable metal stents (EMS) to control contamination is controversial; EMS may reduce sequelae of anastomotic leakage, however, there is a significant risk of EMS migration and erosion of adjacent structures such as the trachea or aorta (4). In this case report we present two cases of massive bleeding after anastomotic leakage of a cervical oesophagogastrostomy with lethal outcome. In the first case a self-expandable stent was used, and in the second case no EMS was used.
Case A
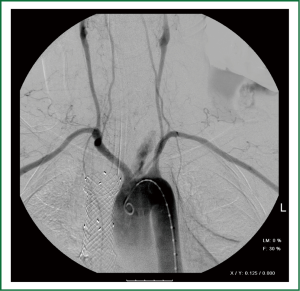
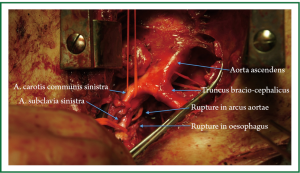
This case describes a 68-year old male patient with a distal esophageal adenocarcinoma that was clinically staged as a T3N1M0 tumor. The patient was treated with neo-adjuvant chemo-radiation and a subsequent thoracolaparoscopic esophagectomy. Six days after surgery the patient’s situation worsened. Tachycardia, tachypnea and a severe fever were the main symptoms. A CT-scan showed no signs of anastomotic leakage. Due to the worsening condition of the patient, the cervical wound was opened and a drain was placed surgically at the site of the anastomosis, despite the negative findings on CT-scan. Cultures were taken from the re-opened neck wound and broad-spectrum antibiotics were started. Antibiotics were switched based on the outcome of the cultures (Escherichia Coli). Eleven days after surgery endoscopic examination of the gastric conduit was performed and showed a massive leak of the anastomosis. An EMS (type Hanarostent 24 mm × 80 mm) was placed over this leak during endoscopy. Eleven days after placement of this stent the hemodynamic situation of the patient suddenly deteriorated. Angiography was performed in the operation theatre and showed contrast leakage to the aortic arch (Figure 1). A sternotomy was performed showing a rupture of the aorta dorsally of the arcus aortae (Figure 2). Unfortunately, due to the location and the infected area there were no endovascular or surgical options to treat this condition and the patient died of exsanguination.
Case B
This case describes a 42-year old male patient with a distal oesophageal adenocarcinoma that was staged as a T3N1M0 tumor. The patient was treated with neo-adjuvant chemotherapy followed by a thoracolaparoscopic esophagectomy. Recovery of the patient was complicated by anastomotic leakage of the cervical anastomosis after 7 days. The cervical wound was opened and a surgical drain was placed at the site of the anastomosis, cultures were taken and broad-spectrum antibiotics were started. Antibiotics were based on the outcome of the cultures (multiple Gram-negative rods). Eleven days after surgery severe hematemesis occurred and shortly after the patient became hemodynamic instable. The patient was taken to the operation theatre, but before any intervention could take place resuscitation was needed and the patient died of exsanguination. Post-mortem investigation showed dehiscence of the anastomosis and signs of severe mediastinitis. In the right pleural cavity 2.5 litre blood was found. Several blood clots were found in the trachea and the gastro-intestinal tract. The responsible blood vessel for this massive bleeding could not be identified.
Discussion
Severe haemorrhage is a rare and highly lethal complication after esophagectomy. This condition seems related to anastomotic leakage with mediastinal manifestation. Although it is believed that cervical oesophagogastrostomy has the potential advantage that a leakage will remain confined to the neck, there is still a considerable risk of mediastinal manifestation (3). There are several risk factors for development of anastomotic leakage such as patient related factors (e.g., BMI) and technical aspects (type of anastomosis) (5). Neoadjuvant chemo(radio)therapy, may also be a risk factor since it modulates certain matrix metalloproteinases (MMP9) involved in breakdown of the submucosal collagen matrix collagen (6). However the exact contribution of neoadjuvant chemo(radio)therapy in development of anastomotic leakage remains elusive. Acute inflammation can result in subsequent erosion into nearby structures. Especially in case of mediastinal inflammation due to intrathoracic manifestation of anastomotic leakage, erosion may extent into adjacent arteries with detrimental consequences (7). Adequate surgical drainage administration of antibiotics and containment of the leakage is therefore essential. Endoscopic placement of an expandable metal stent is a minimally invasive method to prevent further contamination of the mediastinum due to anastomotic leakage. However, some reports describe a dislocation rate of near to 20-40% (2). Furthermore, severe bleeding is also described after EMS placement due to stent migration and erosion into the thoracic aorta (4). It is still unknown if stent migration is the causal factor for the formation of esophageal-vascular fistula, although this seems to be a reasonable contributing factor. Bleeding due to EMS is reported in several months after stent placement or even after removal of the stent (8). Only in very rare cases early bleeding, within two weeks, is described (4). Interestingly, both cases presented describe severe haemorrhage with and without stent placement.
It is possible that certain types of bacteria contribute to aggressive infection and subsequent esophageal-vascular fistula formation. In both cases Gram-negative rods were cultured from the neck wound. Evidence is lacking whether this type of bacteria contributes to risk of bleeding in case of mediastinal manifestation of anastomotic leakage. Reduction of anastomotic leakage is important to prevent its deleterious sequelae. An intra-thoracic anastomosis (Ivor-Lewis) of the gastric conduit with the remaining esophagus is associated with less anastomotic leakage and perioperative death (9). However, in the event of anastomotic leakage mediastinitis is inevitable.
Conclusions
Severe haemorrhage is a rare and potentially lethal complication after esophagectomy. This condition is related to anastomotic leakage wit mediastinal manifestation. Awareness of this complication is important for early recognition and treatment although this complication is often lethal and therapeutic options are often limited.
In our opinion optimal surgical drainage of the mediastinum in combination with antibiotics is the cornerstone of treatment. Endoscopic stenting of the cervical anastomosis is controversial and potentially dangerous.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Nagai Y, Watanabe M, Ikeda O, et al. Successful therapy of brachiocephalic arteriogastric fistula after esophagectomy. Ann Thorac Surg 2011;92:e65-7.
- Kauer WK, Stein HJ, Dittler HJ, et al. Stent implantation as a treatment option in patients with thoracic anastomotic leaks after esophagectomy. Surg Endosc 2008;22:50-3.
- van Heijl M, van Wijngaarden AK, Lagarde SM, et al. Intrathoracic manifestations of cervical anastomotic leaks after transhiatal and transthoracic oesophagectomy. Br J Surg 2010;97:726-31.
- Schweigert M, Dubecz A, Stadlhuber RJ, et al. Risk of stent-related aortic erosion after endoscopic stent insertion for intrathoracic anastomotic leaks after esophagectomy. Ann Thorac Surg 2011;92:513-8.
- Nederlof N, Tilanus HW, Tran TC, et al. End-to-end versus end-to-side esophagogastrostomy after esophageal cancer resection: a prospective randomized study. Ann Surg 2011;254:226-33.
- Rieff EA, Hendriks T, Rutten HJ, et al. Neoadjuvant radiochemotherapy increases matrix metalloproteinase activity in healthy tissue in esophageal cancer patients. Ann Surg Oncol 2009;16:1384-9.
- Pucher P, Kashef E, Woods C, et al. Life-threatening bleeding from arterial-oesophageal fistula following oesophagectomy. Updates Surg 2012. [Epub ahead of print].
- Rogart J, Greenwald A, Rossi F, et al. Aortoesophageal fistula following Polyflex stent placement for refractory benign esophageal stricture. Endoscopy 2007;39:E321-2.
- Schieman C, Wigle DA, Deschamps C, et al. Patterns of operative mortality following esophagectomy. Dis Esophagus 2012;25:645-51.