Negative pressure wound therapy for massive subcutaneous emphysema: a systematic review and case series
Introduction
Subcutaneous emphysema as observed after for example thoracic surgery, trauma, or spontaneous pneumothorax, usually has a mild course and is self-limiting. However, some patients develop massive subcutaneous emphysema, even despite the presence of functional thoracic drainage (1). Massive subcutaneous emphysema is associated with considerable morbidity, including respiratory distress and blocked eyes. Patient anxiety regarding the loss of eyesight can be a major factor driving intervention. In elderly it may even precipitate or exacerbate a delirium (1).
The air leak, causing subcutaneous emphysema should be treated first by the placement of (additional) chest tubes for adequate thoracic drainage. Occasionally, surgical repair of parenchymal or bronchial injury is required in cases with persistent air leakage (1,2). In cases where a fast regression of the subcutaneous emphysema is mandated, which is considered secondary to the air leak, different additional treatment options can be distinguished. These include minimally invasive techniques such as a blowhole incision with or without negative pressure wound therapy (NPWT) and subcutaneous placement of a fenestrated angiocatheter (3).
NPWT in the treatment of subcutaneous emphysema is sparsely reported and a variety of techniques are being used for the placement of the NPWT dressing. Consequently, conclusive evidence on its effectiveness is lacking. Therefore, the aim of the present study is to systematically review the available literature on NPWT in the treatment of massive subcutaneous emphysema. The primary outcome measure was the effectiveness of NPWT in terms of immediate (<24 hours) substantial clinical regression of subcutaneous emphysema. The review was written in accordance with the PRISMA reporting checklist and complemented by a case series of patients with massive subcutaneous emphysema treated with a blowhole incision using NPWT at our clinic (4).
Methods
Systematic review
Protocol and registration
Prior to start, a review protocol was drawn and submitted to the PROSPERO registry (ID: CRD42021262861; Approval date: July 27th, 2021). The present review was written in accordance with the PRISMA reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1483/rc) (4).
Eligibility criteria
Types of participants
All patients presenting with massive subcutaneous emphysema following thoracic surgery, trauma or spontaneous pneumothorax were eligible for inclusion. No restrictions were imposed.
Types of interventions
Studies that used any form of NPWT in the treatment of massive subcutaneous emphysema were considered. Studies performing concomitant treatments such as fenestrated angiocatheters were excluded.
Outcome measures
The primary outcome measures were (I) effectiveness of NPWT in terms of immediate (<24 hours) clinical regression of subcutaneous emphysema, and (II) total resolution of subcutaneous emphysema after completion of NPWT treatment. In addition, the following secondary outcome measures were evaluated: complications related to NPWT graded according to the Clavien-Dindo Classification (5), duration of NPWT and recurrence of subcutaneous emphysema requiring intervention.
Types of studies
All study types were considered. Studies that were not available in English or Dutch were excluded.
Search and study selection
Potentially eligible studies were identified through a systematic search of three electronic databases, including PubMed (National Library of Medicine), Embase (Embase) and Cochrane Library (Cochrane). The search queries are provided in Appendix 1-3. In addition, a manual cross-reference and related articles search was performed. No restrictions regarding publication date were imposed. The last search was performed on August 10th, 2021. The title and abstract of non-duplicate articles were independently screened by two researchers (NJ and JD). Next, the full text of potentially eligible articles was read and assessed according to the aforementioned eligibility criteria. In case of disagreement between the assessors, the senior author (EL) was consulted.
Data collection and data items
Data was extracted by the first author and evaluated for accuracy by JD through random sampling. The senior author (EL) was consulted in case of disagreement. The following data was extracted as reported: (I) study characteristics (study design, size of study sample, enrollment period, country were the study was performed); (II) patient characteristics (sex, age, primary disease or condition causing the subcutaneous emphysema, comorbidities); (III) surgical procedure details (i.e., the technique used for placement of the NPWT dressing); (IV) outcomes and other clinical data (e.g., immediate and/or full response to NPWT, duration of NPWT, mechanical ventilation, whether an (additional) chest tube was placed prior to start of NPWT, number of days between onset of subcutaneous emphysema and start of NPWT, negative pressure that was applied).
Risk of bias in individual studies
Since most included articles encompassed case reports, no risk of bias evaluation was performed.
Summary measures and synthesis of results
Quantitative synthesis of the outcome measures was not performed since the included studies were deemed insufficiently homogenous. Data was reported as such.
Risk of bias across studies
The potential risk of publication bias was qualitatively described given that the creation of a funnel plot was not possible using the data from case reports.
Case series
A single-center retrospective case series study was conducted at the Department of Surgery, Division of General Thoracic Surgery of Zuyderland Medical Centre, Heerlen, the Netherlands. This case series part was written in compliance with the AME Case Series reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1483/rc) (6,7). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Medical Ethics Committee Zuyderland & Zuyd (ID: METCZ20210133; Approval date: August 11th, 2021). Informed consent for this retrospective analysis was waived. One patient approved publishment of perioperative photographs, plain radiographs and photographs depicting the typical clinical course.
Patients who developed massive subcutaneous emphysema following thoracic surgery, trauma, or spontaneous pneumothorax and who were, following adequate thoracic drainage, treated with a blowhole incision using NPWT between February 2019 and July 2021 were retrospectively analyzed. In our clinic, NPWT for subcutaneous emphysema was only indicated in patients in whom the subcutaneous emphysema involved the neck and face causing inability to open their eyes, and/or in patients with respiratory distress.
We performed an infra- and midclavicular incision of approximately 5 cm, located 2 cm below the clavicle on the most affected body side. The procedure was performed under local or general anesthesia (Figure 1). After the incision, subcutaneous tissue was dissected and a small subcutaneous pocket superficial to the fascia was created by blunt dissection to allow placement of the NPWT dressing and air drainage. After placement of the NPWT dressing, the vacuum pump was set a continuous negative pressure of 125 mmHg. Video 1 demonstrates the surgical technique.

Clinical data and endpoints as previously specified for the systematic review were also extracted from the electronic patient files. Clinical manifestation was handled as starting point of the subcutaneous emphysema. An immediate response was classified as a relief of respiratory distress or relieve of obstruction of both eyes within 24 hours after NPWT dressing. Total regression was qualitatively assessed by visual appearance and physical exam.
Categorical variables were denoted as frequency and percentage. Continuous variables were depicted as median and interquartile range (IQR).
Results
Systematic review
Study selection
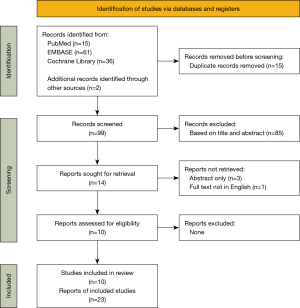
The PRISMA flow diagram provides a detailed description of our study selection process (Figure 2). One hundred twelve articles were retrieved from the electronic scientific databases. Two articles were retrieved by the manual cross-reference and related articles search. Fourteen articles describing the use of NPWT in the treatment of massive subcutaneous emphysema following thoracic surgery, trauma or spontaneous pneumothorax were identified after de-duplication and manual screening. Full text of one article was not available in English and was therefore excluded. In addition, from another three articles only the abstract was available. The remainder of 10 articles were included, describing a total of 23 unique cases (8-17).
Study characteristics
Methods
All studies concerned retrospective case reports or case series. Cases were reported between 2009 and 2020, originating from Croatia, Korea, Malaysia, the Netherlands, New Zealand, Saudi Arabia, and the USA.
Participants
Patient characteristics and clinical data are summarized in respectively Tables 1,2. Patients’ age varied from 42 to 87 years. Subcutaneous emphysema occurred following secondary spontaneous pneumothorax (n=9/23), traumatic pneumothorax (n=5/23 patients), ventilator associated barotrauma (n=5/23 patient) or lung surgery (n=4/23 patients).
Table 1
| Study (year) | Country | Study type (level of evidence) | Patients, (n) | Gender, male (%) | Age, median (IQR) | Primary disease (n) | Comorbidities |
|---|---|---|---|---|---|---|---|
| Sciortino et al. (2009) | USA | Case-study (level V) | 1 | 100 | 70 | Secondary spontaneous pneumothorax due to bullous emphysema | None |
| Byun et al. (2013) | Korea | Case-series (level V) | 4 | 100 | 73 (69–76) | Secondary spontaneous pneumothorax due to COPD with emphysema | NR |
| Towe et al. (2014) | USA | Case-study (level V) | 1 | 100 | 74 | Malignancy treated with VATS lobectomy | Coronary disease |
| Son et al. (2014) | Korea | Case-series (level V) | 10 | 70 | Mean 62 (range, 42–81) | Lung surgery-related (1), blunt trauma-related lung laceration (1), ventilator associated barotrauma (5), bronchopleural fistula post-lung transplantation (1), secondary spontaneous pneumothorax (1) | NR |
| Mihanović et al. (2018) | Croatia | Case-study (level V) | 1 | 100 | 60 | Traumatic pneumothorax (rib fractures with bilateral pneumothorax) | Lung malignancy treated with lobectomy |
| Sindi et al. (2019) | Saudi Arabia | Case-study (level V) | 1 | 100 | 7 | Traumatic pneumothorax | None |
| Taylor et al. (2020) | USA | Case-study (level V) | 1 | 0 | 52 | Traumatic pneumothorax (rib fractures with bilateral pneumothorax and pneumomediastinum) | COPD, cardiomyopathy, bipolar disorder |
| Prakash et al. (2020) | New Zealand | Case-study (level V) | 1 | 100 | 54 | Traumatic pneumothorax | Emphysema, blood dyscrasia, schizophrenia, end-stage liver failure with coagulopathy |
| Huan et al. (2020) | Malaysia | Case-study (level V) | 1 | 100 | 80 | Secondary spontaneous pneumothorax due to COPD | None |
| Wezel et al. (2020) | The Netherlands | Case-series (level V) | 2 | 100 | (range, 66–75) | Secondary spontaneous pneumothorax due to bullous emphysema (1), secondary spontaneous pneumothorax due to COPD (1) | NR |
COPD, chronic obstructive pulmonary disease; IQR, inter-quartal range; NR, not reported; VATS, video assisted thoracic surgery.
Table 2
| Article | Mechanical ventilation | Chest tube placed prior to NPWT | Pressure NPWT, mmHg | Days to NPWT, median (range) |
|---|---|---|---|---|
| Sciortino et al. (2009) | Yes | Yes | 100 | Unknown |
| Byun et al. (2013) | No | Yes | 150 | 0–3 |
| Towe et al. (2014) | No | Yes | 125 | 8 |
| Son et al. (2014) | Yes | Yes | 150 | 1–7 |
| Mihanović et al. (2018) | Yes | Yes | 100 | NR |
| Sindi et al. (2019) | Yes | Yes | NR | 0 |
| Taylor et al. (2020) | Yes | Yes | 125 | 6 |
| Prakash et al. (2020) | No | Yes | NR | 0 |
| Huan et al. (2020) | Yes | Yes | 50 | NR |
| Wezel et al. (2020) | No | Yes | 125 | NR |
NPWT, negative pressure wound therapy; NR, not reported.
Interventions
Different NPWT techniques were reported which varied from location of incision, and creation of a prepectoral pocket. In addition, the use of closed incision NPWT (ciNPWT) and PICO© device were reported. Most articles (n=6/10) described a small infraclavicular blowhole incision technique, creating a prepectoral pocket to insert the NPWT foam (9-11,15-17). The incision lengths differed from 2 to 6 cm. In five cases a blowhole incision was not only placed on the affected body half but also on the contralateral side while the clinician felt it was necessary for adequate treatment given the extent of emphysema (8,10,16,17). In three patients the incision was placed supraclavicular, based on the severity and location of the subcutaneous emphysema (10).
Huan et al. handled a specific position of the blowhole incision. They placed the incision 5 cm below the clavicle and 5 cm from the sagittal midline. They also assured that the incision was placed at the superior border of the underlying rib (8). Furthermore, the article by Towe et al. recommended a safety margin between the clavicle and the incision, keeping at least 4 cm space in between (11).
Alternative techniques were described by Son et al., Taylor et al., and Prakash et al. (12-14). Namely, Son et al. described the creation of a large subcutaneous pocket over the pectoral fascia for better drainage. Two 2–3 cm long blocked shaped foam pieces are inserted into the pocket (12). They report no bleeding associated with dressing changes or wound healing problems as they formed a sort of tunneled wound by creating a large subcutaneous pocket.
Taylor et al. implemented the use of closed incision NPWT (ciNPWT) for the treatment of subcutaneous emphysema. They also performed an incision just below the clavicula, 3 cm length, and then loosely closed the incision using a simple one-layer technique. The foam was then applied over the loosely closed incision. The proposed advantages of this technique were the avoidance of potential bleeding and pain caused by dressing changes, as well as the fact that the technique prevents collapse of the foam over a tunneled wound (14).
Prakash et al. used a PICO© system, a specific single-use NPWT device, instead of the conventional NPWT. The PICO© system from Smith & Nephew’s consists of a small NPWT pump connected to an absorbent and adhesive dressing. The dressing is normally placed over an incision or superficial wound as the system does not contain a polyurethane foam that can fill up and apply suction pressures on deeper wounds. However, Prakash et al. applied the PICO© dressing on top of the regular polyurethane foam that was placed into the incision as usual. The connector of the PICO© system was attached to wall suction. An airtight sealing was reached (13).
Set pressures of the NPWT device varied from 50 to 150 mmHg. Only one article did apply a pressure <100 mmHg (9); two articles did not report pressure rates including Prakash et al. reporting the PICO© technique (13,17). Sufficient air drainage was reached with the above-mentioned suction pressures in all cases and no pressure adjustments were made. No wound or dressing related pain was reported in the cases where a higher negative pressure was applied.
Synthesis of results
Qualitative synthesis
Most articles (7/10 articles, 20/23 patients) reported an immediate response to NPWT therapy and all articles described a full response. Immediate and full response rates per article, as well as the other outcomes are summarized in Table 3. Towe et al. reported a partial response at initial placement, but a full response after adequate replacement. Sciortino et al. document stabilization during the first 48 hours and decrease of the subcutaneous emphysema thereafter (10). No direct link between the application technique of the NPWT and the lower response rate could be found as the mentioned articles applied the most used technique of the blowhole incision and report no alterations or particularities that could explain a diminished response. Duration of NPWT varied strongly, with a median duration of 4 days (IQR 3–7.5 days). No relation with the used technique was observed. No statement can be made about a possible relation between the length of the period prior to start of NPWT and duration of the NPWT due to lacking data.
Table 3
| Study (year) | Patients, (n) | Immediate response (<24 hours) | Full response | Duration of NPWT (days) | Complications associated with NPWT | Recurrence requiring intervention |
|---|---|---|---|---|---|---|
| Sciortino et al. (2009) | 1 | No, only stabilization | Yes | Unknown | None | No |
| Byun et al. (2013) | 4 | Yes | Yes | 2–4 | None | No |
| Towe et al. (2014) | 1 | No | Yes | 6 | None | No |
| Son et al. (2014) | 10 | Yes | Yes | 3–14 | None | No |
| Mihanović et al. (2018) | 1 | Yes | Yes | 3 | None | No |
| Sindi et al. (2019) | 1 | NR | Yes | NR | None | No |
| Taylor et al. (2020) | 1 | Yes | Yes | 8 | None | No |
| Prakash et al. (2020) | 1 | Yes | Yes | NR | None | No |
| Huan et al. (2020) | 1 | Yes | Yes | 4 | None | No |
| Wezel et al. (2020) | 2 | Yes | Yes | 8 in one case, other case unknown | None | No |
| All patients | 23 | 87% (20/23) | 100% (23/23) | 2–14 | 0% (0/23) | 0% (0/23) |
NPWT, negative pressure wound therapy; NR, not reported.
No complications related to the use of NPWT or recurrence of the subcutaneous emphysema to a degree that required intervention were documented. Also in case of the creation of a tunneled wound no complications were seen.
Case series
In our retrospective series, all potential eligible patients (n=11) met the inclusion criteria. No concomitant treatments were performed. Most patients (n=7/11) underwent an uniportal video assisted thoracic surgery (uVATS) lobectomy, while the remaining patients were surgically treated by an uVATS approach for pleural empyema (n=1), mediastinal lymph node dissection (n=1) and pleural biopsy (n=1); One patient had a secondary spontaneous pneumothorax caused by underlying chronic obstructive pulmonary disease (COPD). The median age in our series was 69 (IQR 65–72), and male:female ratio was 7:4. Most patients (6/11) had lung related comorbidities including COPD (n=5), emphysema (n=1), asthma (n=1), and post corona virus disease (COVID) pneumonia (n=1). Patients’ comorbidities included cerebral ischemia (n=2), atrial fibrillation (n=2), aortic aneurysm (n=1), congestive heart failure (n=1), esophageal carcinoma (n=1), and peripheral arterial disease (n=1). Two patients of this cohort required mechanical ventilation support for respiratory insufficiency resulting from post-operative pneumonia. One of these two patients also suffered from a segmental lung embolus.
NPWT was initiated at a median of 5 days (IQR 2–13) after subcutaneous emphysema symptoms were first observed. In all patients a chest tube was in situ upon start of NPWT. Chest tubes were on a no suction-water seal regime.
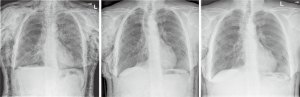
Outcomes of the blowhole incision with NPWT are shown in Table 4. In 9/11 patients, subcutaneous emphysema totally resolved during NPWT, and all patients showed direct improvement after initiation of NPWT. Figures 3,4 demonstrate the clinical course of one of the included patients. A median duration of the NPWT of 8 days was observed (IQR 6–11), with 1 or 2 wound dressings. No complications related to the subcutaneous emphysema were reported and there was no recurrence requiring intervention. One patient subsequently underwent parenchymal repair by uVATS because of ongoing air leakage. Complete regression of the subcutaneous emphysema was achieved by NPWT and the patient was therefore not excluded. One of the two patients that required mechanical ventilation support died during hospitalization due to sepsis. Additionally, the patient who presented with a secondary spontaneous pneumothorax died during hospitalization due to a combination of respiratory failure and pre-existing comorbidities including COPD GOLD IV and congestive heart failure. The patient who received a pleural biopsy had a complicated postoperative course due to pleural empyema and the biopsy showed pleural carcinosis. He was transferred to a palliative unit.
Table 4
| Patient number | Immediate response (<24 hours) | Full response | Number of dressings | Duration of NPWT (days) | Complications associated with NPWT | Recurrence requiring intervention |
|---|---|---|---|---|---|---|
| 1† | Yes | Yes | 1 | 7 | None | NA |
| 2 | Yes | Yes | 1 | 5 | None | No |
| 3 | No, only stabilization | Yes | 1 | 6 | None | No |
| 4 | Yes | Yes | 1 | 6 | None | No |
| 5 | Yes | Yes | 2 | 8 | None | No |
| 6 | Yes | Yes | 2 | 10 | None | No |
| 7 | Yes | Yes | 2 | 11 | None | No |
| 8† | Yes | No | 1 | 2 | None | NA |
| 9 | Yes | Yes | 1 | 9 | None | No |
| 10 | Yes | Yes | 1 | 11 | None | No |
| 11† | Yes | Yes | 1 | 13 | None | NA |
| All patients | 11 | 91% (10/11) | 1–2 | Median 8, IQR (6–11) | 0% (0/11) | 0% (0/11) |
†, died during or shortly after hospitalization. NA, not applicable; NPWT, negative pressure wound therapy.

In the minority of patients (n=3/11 patients), NPWT was continued until air leakage ceased, and all chest tubes were removed. In about a half (n=5/11 patients), NPWT was stopped prior to removal of the chest tubes. The decision to stop NPWT prior to removal of the chest tubes was based on a major decrease of air leakage through the chest tubes as well as the absence of subcutaneous emphysema for several consecutive days. In the two patients that died during hospitalization and the patient that was transferred to a palliative unit, NPWT was discontinued.
Discussion
Clinical symptoms of subcutaneous emphysema vary from mild pain and disfigurement of the chest wall’s contour to obstruction of the eyes and respiratory distress as seen in massive subcutaneous emphysema. Although subcutaneous emphysema is often self-limiting, fast release of trapped subcutaneous air may be mandated in the presence of massive subcutaneous emphysema. This study showed that different techniques involving a blowhole incision with the use of NPWT are all associated with favorable outcomes. No preference regarding the most optimal technique can be made.
For the indication of subcutaneous emphysema there is no literature available on placement of the blowhole incision at another location than infraclavicular or supraclavicular. We hypothesize that re-opening the uniportal access for the placement of the NPWT foam could lead to an empyema as it creates a transmission route to the thoracic cavity. It could also provoke the development of a thoracic wall hernia. Moreover, most of the subcutaneous emphysema is centered around the neck and face as the trapped air tends to migrate upwards. Therefore, we advise an infraclavicular or supraclavicular incision as this will allow optimal air drainage without placement of the additional scarring at a prominent location.
Different treatment options for subcutaneous emphysema have been described in the literature. Johnson et al. systematically reviewed 14 articles to identify the ideal technique for the treatment of severe subcutaneous emphysema, encompassing conventional blowhole incisions, insertion of a subcutaneous drain and applying suction to an already present chest tube. They concluded that in the absence of comparative studies no conclusion can be drawn regarding the most favorable technique (3). Subcutaneous drains may be potentially favored due to their simplicity and their relatively low-cost (18). However, disadvantages of such catheters are that they tend to get blocked by blood clots or the subcutaneous fat itself quite fast. In addition, they easily luxate or fail to function adequately at all. The duration of the treatment also varies greatly among the articles (1–7 days) (3).
The first description of a blowhole incision with the use of NPWT for the treatment of massive subcutaneous emphysema was by Sciortino et al. in 2009; whereupon several other small case series followed (8-17). Conventional blowhole incisions were widely used before. However, they are associated with more complications (i.e. wound infections) due to the fact that the wound needs to be kept open for sufficient air drainage. In addition, frequent changes of the dressing causes considerable patient discomfort. As there is no negative pressure suction on the wound bed and the subcutaneous emphysema must resolve by passive drainage, the results are not optimal and prolonged treatment is often necessary, also adding to a higher infection risk (3,16).
On the contrary, a blowhole incision with the use of NPWT is a quick and sterile procedure that can easily be performed under local anesthesia, and is therefore also suitable for patients with critical comorbidities. If necessary, it can safely remain in situ for extended time periods without the risk of malfunctioning (16). A possible disadvantage is that high suction pressures in NPWT may cause discomfort to the patient. However, negative pressures up to 150mmHg were tolerated by the patients in the described cases. Nevertheless, in individuals where such pressures cause discomfort, the suction pressure can be lowered to a level that is tolerated as lower suction pressures also provided sufficient air drainage in reported cases.
This study is the first study that systematically reviewed and critically appraised the literature specifically on the use of NPWT for the treatment of massive subcutaneous emphysema. We also presented a cases series of 11 patients treated at our clinic which is the largest case series reported to date. The first limitation of this study is that in the analysis of the outcome of the surgical techniques there may have been a selection bias due to the lack of definition or commonly agreed upon indications for massive subcutaneous emphysema. The second limitation is the possible publication bias because of the very limited number of cases described. However, in our case series all potentially includable patients met the eligibility criteria, and a favorable outcome was seen in all cases. Furthermore, one article was excluded based on availability of full text in English as the reviewers had no access to a translation service. Results of the systematic review may have been further limited by the low quality of evidence of the selected studies.
Further studies are needed to corroborate the evidence on the usefulness and cost-effectiveness of NPWT. Future studies should be designed as a randomized controlled trial and compare NPWT to conservative treatment as well as other treatment modalities. However, adequately powered studies may be hard to constitute. We furthermore propose to address the topic of the duration between the occurrence of symptomatic subcutaneous emphysema in a patient and the start of NPWT to establish if associated morbidity can be limited by earlier intervention.
Conclusions
NPWT seems to be an effective treatment modality for massive subcutaneous emphysema generally resulting in quick improvement of symptoms. No obvious differences are described regarding the optimal technique for NPWT. Future comparative studies are recommended to corroborate this evidence and to compare results with conservative treatment as well as other treatment options.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA and AME Case Series reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1483/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1483/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1483/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Medical Ethics Committee Zuyderland & Zuyd (ID: METCZ20210133; Approval date: August 11th, 2021). Informed consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Herlan DB, Landreneau RJ, Ferson PF. Massive spontaneous subcutaneous emphysema; Acute management with infraclavicular “blow holes”. Chest 1992;102:503-5. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Maniscalco LM. Management of subcutaneous emphysema after pulmonary resection. Ann Thorac Surg 2008;85:1759-63; discussion 1764-5. [Crossref] [PubMed]
- Johnson CH, Lang SA, Bilal H, et al. In patients with extensive subcutaneous emphysema, which technique achieves maximal clinical resolution: infraclavicular incisions, subcutaneous drain insertion or suction on in situ chest drain? Interact Cardiovasc Thorac Surg 2014;18:825-9. [Crossref] [PubMed]
- Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [Crossref] [PubMed]
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. BMJ Case Rep 2013;2013:bcr2013201554. [Crossref] [PubMed]
- Agha RA, Sohrabi C, Mathew G, et al. The PROCESS 2020 Guideline: Updating Consensus Preferred Reporting Of CasESeries in Surgery (PROCESS) Guidelines. Int J Surg 2020;84:231-5. [Crossref] [PubMed]
- Huan NC, Mohamed Arifin N, Khoo TS, et al. Management of extensive subcutaneous emphysema using negative pressure wound therapy dressings. Respirol Case Rep 2020;8:e00544. [Crossref] [PubMed]
- Byun CS, Choi JH, Hwang JJ, et al. Vacuum-assisted closure therapy as an alternative treatment of subcutaneous emphysema. Korean J Thorac Cardiovasc Surg 2013;46:383-7. [Crossref] [PubMed]
- Sciortino CM, Mundinger GS, Kuwayama DP, et al. Case report: treatment of severe subcutaneous emphysema with a negative pressure wound therapy dressing. Eplasty 2009;9:e1. [PubMed]
- Towe C, Solomon B, Donington JS, et al. Treatment of recalcitrant subcutaneous emphysema using negative pressure wound therapy dressings. BMJ Case Rep 2014;2014:bcr2014205577. [Crossref] [PubMed]
- Son BS, Lee S, Cho WH, et al. Modified blowhole skin incision using negative pressure wound therapy in the treatment of ventilator-related severe subcutaneous emphysema. Interact Cardiovasc Thorac Surg 2014;19:904-7. [Crossref] [PubMed]
- Prakash M, Meikle F. How to create negative pressure wound dressing with wall suction: novel treatment of subcutaneous emphysema with PICO dressing. ANZ J Surg 2020; [Epub ahead of print]. [PubMed]
- Taylor BC, McGowan S. Use of Closed Incision Negative Pressure Therapy for Massive Subcutaneous Emphysema. Cureus 2020;12:e7399. [Crossref] [PubMed]
- Mihanović J, Bačić I, Sulen N. Negative-pressure in treatment of persistent post-traumatic subcutaneous emphysema with respiratory failure: Case report and literature review. Trauma Case Rep 2018;13:42-5. [Crossref] [PubMed]
- Wezel A, Kidane AS, Oosterhuis JWA. Negative pressure therapy for the treatment of severe subcutaneous emphysema. Ned Tijdschr Geneeskd 2020;164:D5186. [PubMed]
- Sindi D, Mirza A, Khirallah M, et al. Management of extensive subcutaneous emphysema using vacuum-assisted closure therapy. J Pediatr Surg Case Reports 2019;48:101272. [Crossref]
- Ahmed Z, Patel P, Singh S, et al. High negative pressure subcutaneous suction drain for managing debilitating subcutaneous emphysema secondary to tube thoracostomy for an iatrogenic post computed tomography guided transthoracic needle biopsy pneumothorax: Case report and review of literat. Int J Surg Case Rep 2016;26:138-41. [Crossref] [PubMed]