Prevalence of carotid artery stenosis in Chinese patients with angina pectoris
Introduction
In China, stroke has surpassed cardiovascular disease as the leading cause of death and adult disability (1). Carotid artery atherosclerotic stenosis is an important cause of stroke worldwide (2). Unlike in western countries, patients in China and other Asian countries predominantly exhibit intracranial atherosclerotic stenosis (3-5), whereas those in western countries are more likely to experience extracranial carotid artery stenosis (CAS) (6). However, recent studies have shown that significant extracranial CAS is not uncommon in Asian populations (7,8). The rising prevalence of extracranial carotid and vertebral artery disease was noted in a Chinese population (9) and may due to lifestyle changes in an effort to adopt western habits.
Atherosclerosis is a systemic disorder that can involve multiple arterial beds (10). The association between CAS and coronary artery disease (CAD) has been widely reported (11-13). Approximately 8% to 14% of patients undergoing myocardial revascularization because of CAD have significant CAS (14), and 28% of patients in western countries who are candidates for carotid endarterectomy because of CAS have significant CAD (15). However, until now, few studies have determined the prevalence of CAS in Chinese patients with angina pectoris.
We performed carotid ultrasonography, which is the first choice for imaging in carotid stenosis screening (16), in consecutive patients undergoing nonemergent coronary artery angiography. We investigated the prevalence and severity of CAS in a Chinese patient population with angina pectoris to identify the risk factors associated with CAS.
Materials and methods
Study population
The study population consisted of 989 consecutive patients with angina pectoris who were scheduled to undergo nonemergent coronary angiography for suspicion of CAD between January 2013 and December 2014 at our hospital. Patients who were making their initial visits to the clinic and patients with previous percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) histories were enrolled. Patients who did not undergo coronary angiography and carotid ultrasonography within a month before or after coronary angiography were also excluded. The study procedures were in accordance with institutional guidelines. All data were collected retrospectively. The study was approved by the institutional ethics committee of our hospital.
Associated risk factors
The risk factor variables evaluated in the study included age, sex, body mass index (BMI), hypertension, hyperlipidemia, diabetes mellitus, chronic kidney insufficiency, smoking, hyperhomocysteinemia, history of stroke, history of myocardial infarction and previous PCI or CABG.
Hypertension was defined as any history of hypertension or if the subject’s blood pressure exceeded 140 mmHg in systole or 90 mmHg in diastole according to at least two measurements performed in the hospital. Hyperlipidemia was defined as a fasting serum total cholesterol of >200 mg/dL, triglyceride concentration of >150 mg/dL, low-density lipoprotein cholesterol concentration of >140 mg/dL, high-density lipoprotein cholesterol concentration of <40 mg/dL or documented hyperlipidemia requiring lipid-lowering drug therapy. Diabetes mellitus was defined as a requirement for diabetes medication or a repeated fasting plasma glucose level exceeding 126 mg/dL or 200 mg/dL 2 hours after eating. Chronic kidney insufficiency was defined as evidence of renal damage or a glomerular filtration rate of <60 mL/min/1.73 m2. Smoking was defined as if the patient smoked >1 cigarette per day for more than 6 months or had quit smoking for less than 2 years. Hyperhomocysteinemia was defined as a serum homocysteine concentration of >15 umol/L.
Definition of CAD
Nonemergent coronary angiography to investigate CAD was performed with a commercially available machine (Allura Xper FD20, Phillips) by standard techniques. The percentage of diameter stenosis was calculated by quantitative coronary angiography with an automated coronary analysis system (DCI-S, Phillips Medical System). CAD was defined as a lumen diameter stenosis of >50% in at least one major coronary artery (left anterior descending artery, left circumflex artery, right coronary artery or grafting vessel in patients with previous CABG). CAD was also considered present if the stenosis existed in some major branches (e.g., marginal or diagonal arteries) of the major coronary artery as mentioned above. According to the number of diseased vessels, each patient was classified into 1 of the following 4 groups: group 1, patients with 0-vessel disease; group 2, patients with 1-vessel disease; group 3, patients with 2-vessel disease; and group 4, patients with 3-vessel disease or left main trunk disease with right coronary artery disease.
Definition of CAS
CAS was investigated by carotid duplex ultrasound scanning using a commercially available machine (SSA-660A, Toshiba) with a 10-MHz linear array transducer. The sonography technician was experienced and blinded to clinical and coronary angiographic data. The sites of the extracranial measurements included the common carotid artery, bifurcation and internal carotid artery. The intima-media thickness, lumen diameter and the diameter of atherosclerotic plaque were also measured. The carotid stenosis was evaluated by the maximum percentage of diameter reduction recorded by B-mode ultrasound, by peak systolic velocity (PSV) and by peak diastolic velocity per Doppler. The maximum stenosis was defined as the greatest stenosis observed in the common carotid artery, bifurcation and internal carotid artery either on the right or left. Patients were classified into the following five categories: normal (carotid arteries with no signs of atherosclerotic lesion, no plaque and normal intima-media thickness); mild CAS (stenosis diameter <50% and PSV <125 cm/s); moderate CAS (stenosis diameter 50% to 70% and PSV between 125 and 230 cm/s); severe CAS (stenosis diameter >70% and PSV >230 cm/s); and total occlusion (PSV of 0). We defined cases of moderate CAS, severe CAS and total occlusion to be significant CAS.
Statistical analysis
Continuous variables are presented as the mean ± SD. A two-sided unpaired t-test was performed for continuous variables, and the chi-square test or Fisher’s exact test was used to analyze discrete variables. Spearman correlation was used to evaluate the relationship between CAS severity and CAD extent. Multivariate stepwise logistic regression analysis was applied to detect independent predictors of significant CAS. Data analysis was performed using SPSS version 22 (SPSS Inc., Chicago, IL, USA). A P value of <0.05 was considered statistically significant.
Results
The final study population consisted of 989 consecutive patients (627 men; mean age 63.4±10.5 years, range 32 to 91 years), and the demographic and clinical features of the patient cohort are presented in Table 1.
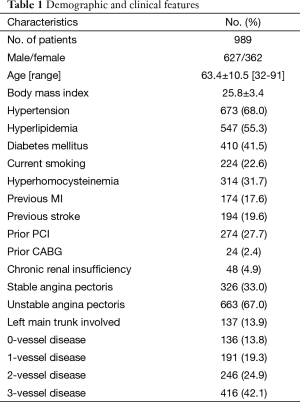
Full table
In the entire study population, CAD was present in 853 patients (86.2%) of whom 191 patients (19.3%) had 1-vessel disease, 246 patients (24.9%) had 2-vessel disease and 416 patients (42.1%) had 3-vessel disease. Left main trunk stenosis was present in 137 patients (13.9%). In carotid ultrasonography, 267 patients (27%) had patent carotid arteries without any evidence of atherosclerosis. The prevalence of mild, moderate, and severe stenosis as well as that of total occlusion of the carotid artery was 54.5%, 13%, 4.7% and 0.8%, respectively. Significant CAS (>50% stenosis diameter and total occlusion) was present in 10.3%, 13.1%, 19.9%, 22.8% and 30.7% of patients with 0-vessel, 1-vessel, 2-vessel, 3-vessel and left main trunk involved CAD, respectively (Table 2). There was a stepwise increase in the number of patients with significant CAS among patients with increasing severity of CAD (Figure 1). The severity of CAS was weakly correlated (r=0.194, P<0.001) with the extent of CAD.

Full table
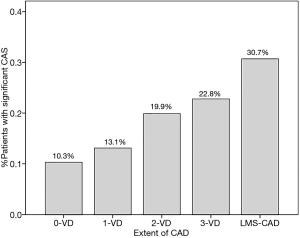
The incidence of significant CAS was higher in patients with left main trunk involvement than in the study population as a whole (30.7% vs. 18.5%, P< 0.001).
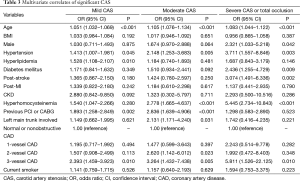
A forward stepwise logistic regression was applied to identify factors that were associated with CAS. The results of this analysis are presented in Table 3. The independent predictors of severe CAS and total carotid artery occlusion were increased age, male sex, hypertension, diabetes mellitus, hyperhomocysteinemia, a previous history of stroke and 3-vessel CAD.
Full table
Discussion
Our principle finding was that the prevalence of CAS was not rare in China compared with that in western countries, and the presence of CAS was weakly correlated with the extent of CAD. Furthermore, age, male sex, hypertension, diabetes mellitus, hyperhomocysteinemia, a previous history of stroke, and 3-vessel CAD were independently related to the presence of severe CAS and total carotid artery occlusion.
The different prevalence rates of CAS between western and Asian countries have been reported in many studies (4,6,8,17). A magnetic resonance angiography study (4) in Chinese stroke patients showed that extracranial CAS was less frequent in Chinese patients than in patients from western countries (14% compared with 30% to 60% in western patients), whereas intracranial lesions were more common (46.6%). In the 1990s, Shi (18) reported that the incidence of clinically significant extracranial CAS was 3% in Chinese elderly patients without CAD. The incidence of extracranial CAS has increased in the past few decades in Asian countries. In 2005, Tanimoto et al. (19) reported that the incidence of CAS was 7% in patients without CAD in a Japanese population. Our study showed that CAS was present in 10.3% of patients without CAD. The reported prevalence of CAS in western countries has ranged from 2% to 18% among the patients studied (15). Thus, the prevalence of CAS in our cohort was comparable with those reported in western populations, which may be due to lifestyle changes in China that favor western habits. Another possible explanation for the increased prevalence of CAS in China may be improved diagnostic techniques and screening frequencies compared with those of western countries.
Atherosclerosis can affect both the coronary artery and the carotid artery. Concurrent CAS and CAD are frequently detected in clinical practice (20). Autopsy studies (21) and clinical studies (15) have demonstrated a strong correlation between the extent of CAD and CAS. Ciccone (22) reported that the left ventricular mass index (LVMI) and the severity of CAD were positively related to the carotid intima media thickness in an Italian patient population. However, the prevalence of CAS in Chinese patients with angina pectoris has not been well evaluated. In our study, the prevalence of significant CAS was 18.5% in patients with angina pectoris, and the severity of CAS was weakly correlated with the extent of CAD.
It has been reported (23) that soft carotid plaque with large necrotic core may be predictive of increased risk for neurological events, and heavily calcified plaque may be indicative of a high risk of coronary events. The presence of CAS in patients with CAD is associated with apparently higher perioperative stroke if the patient requires heart surgery (24,25). During coronary revascularization, neurological complication is the leading cause of mortality and disability (25,26). Thus, to decrease the neurological complication rate, Ascher et al. (27) indicated that carotid screening is recommended for patients undergoing open heart surgery who are over 60-year-old or less than 60-year-old but have risk factors for CAS.
It has been reported that carotid screening may be cost-effective in patients for whom the prevalence of severe CAS exceeds 4.5% (27). Age and sex may influence the detection of early markers of atherosclerosis (28). CAS screening seems insufficient in China because the prevalence of CAS was assumed to be low in these patients. In our study population, the prevalence of severe CAS reached 5.5% and increased age, male sex, hypertension, diabetes mellitus, hyperhomocysteinemia, a previous history of stroke and 3-vessel CAD were identified as predictors of concomitant CAS. Therefore, we recommend that screening for CAS should be carried out in Chinese patients with angina pectoris, especially those with the risk factors mentioned above.
There may be limitations to our study. First, this is a retrospective study, and all limitations inherent in any retrospective study may also exist here. Second, the enrolled patients were referred for coronary angiography because of angina pectoris. Thus, our findings are relevant only to this particular group of patients and may not be applicable to the general population. Third, compared with selective intra-arterial digital subtraction angiography, color duplex sonography has an overall sensitivity of 91% to 95% and a specificity of 86% to 97% (16), and therefore, false positive or negative results may be present in the CAS screening data reported here.
Conclusions
In conclusion, the prevalence of CAS was not rare in China compared with western countries, and the presence of CAS was weakly correlated with the extent of CAD. CAS screening is recommended in Chinese patients with CAD, especially in those with one or more CAS-associated risk factors.
Acknowledgements
Funding: This work was supported by a China International Cooperation Grant (No. 2013DFA31900).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Liu L, Wang D, Wong KS, et al. Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke 2011;42:3651-4. [PubMed]
- Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009;8:355-69. [PubMed]
- Kieffer SA, Takeya Y, Resch JA, et al. Racial differences in cerebrovascular disease. Angiographic evaluation of Japanese and American populations. Am J Roentgenol Radium Ther Nucl Med 1967;101:94-9. [PubMed]
- Wang Y, Zhao X, Liu L, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke 2014;45:663-9. [PubMed]
- Wu YW, Lin MS, Lin YH, et al. Prevalence of concomitant atherosclerotic arterial diseases in patients with significant cervical carotid artery stenosis in Taiwan. Int J Cardiovasc Imaging 2007;23:433-9. [PubMed]
- Gorelick PB, Caplan LR, Hier DB, et al. Racial differences in the distribution of anterior circulation occlusive disease. Neurology 1984;34:54-9. [PubMed]
- Mannami T, Baba S, Ogata J. Strong and significant relationships between aggregation of major coronary risk factors and the acceleration of carotid atherosclerosis in the general population of a Japanese city: the Suita Study. Arch Intern Med 2000;160:2297-303. [PubMed]
- Jeng JS, Chung MY, Yip PK, et al. Extracranial carotid atherosclerosis and vascular risk factors in different types of ischemic stroke in Taiwan. Stroke 1994;25:1989-93. [PubMed]
- Chen WH, Ho DS, Ho SL, et al. Prevalence of extracranial carotid and vertebral artery disease in Chinese patients with coronary artery disease. Stroke 1998;29:631-4. [PubMed]
- Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med 1999;340:115-26. [PubMed]
- Sanguigni V, Gallù M, Strano A. Incidence of carotid artery atherosclerosis in patients with coronary artery disease. Angiology 1993;44:34-8. [PubMed]
- Salasidis GC, Latter DA, Steinmetz OK, et al. Carotid artery duplex scanning in preoperative assessment for coronary artery revascularization: the association between peripheral vascular disease, carotid artery stenosis, and stroke. J Vasc Surg 1995;21:154-60; discussion 161-2. [PubMed]
- Craven TE, Ryu JE, Espeland MA, et al. Evaluation of the associations between carotid artery atherosclerosis and coronary artery stenosis. A case-control study. Circulation 1990;82:1230-42. [PubMed]
- Borger MA, Fremes SE, Weisel RD, et al. Coronary bypass and carotid endarterectomy: does a combined approach increase risk? A metaanalysis. Ann Thorac Surg 1999;68:14-20; discussion 21. [PubMed]
- Steinvil A, Sadeh B, Arbel Y, et al. Prevalence and predictors of concomitant carotid and coronary artery atherosclerotic disease. J Am Coll Cardiol 2011;57:779-83. [PubMed]
- Gaitini D, Soudack M. Diagnosing carotid stenosis by Doppler sonography: state of the art. J Ultrasound Med 2005;24:1127-36. [PubMed]
- Brust RW Jr. Patterns of cerebrovascular disease in Japanese and other population groups in Hawaii: an angiographical study. Stroke 1975;6:539-42. [PubMed]
- Shi Z, Shen P, Shen G. The prevalence and risk factors of carotid atherosclerosis in elderly patients. Zhonghua Nei Ke Za Zhi 1996;35:25-7. [PubMed]
- Tanimoto S, Ikari Y, Tanabe K, et al. Prevalence of carotid artery stenosis in patients with coronary artery disease in Japanese population. Stroke 2005;36:2094-8. [PubMed]
- Roffi M, Cremonesi A. Current concepts on the management of concomitant carotid and coronary disease. J Cardiovasc Surg (Torino) 2013;54:47-54. [PubMed]
- Mathur KS, Kashyap SK, Kumar V. Correlation of the extent and severity of atherosclerosis in the coronary and cerebral arteries. Circulation 1963;27:929-34. [PubMed]
- Ciccone MM, Scicchitano P, Zito A, et al. Correlation between coronary artery disease severity, left ventricular mass index and carotid intima media thickness, assessed by radio-frequency. Cardiovasc Ultrasound 2011;9:32. [PubMed]
- Ciccone MM, Marzullo A, Mizio D, et al. Can carotid plaque histology selectively predict the risk of an acute coronary syndrome? Int Heart J 2011;52:72-7. [PubMed]
- Anastasiadis K, Karamitsos TD, Velissaris I, et al. Preoperative screening and management of carotid artery disease in patients undergoing cardiac surgery. Perfusion 2009;24:257-62. [PubMed]
- Naylor AR, Mehta Z, Rothwell PM, et al. Reprinted article "Carotid artery disease and stroke during coronary artery bypass: a critical review of the literature". Eur J Vasc Endovasc Surg 2011;42 Suppl 1:S73-83. [PubMed]
- Prapas SN, Tsakiridis K, Zarogoulidis P, et al. Current options for treatment of chronic coronary artery disease. J Thorac Dis 2014;6 Suppl 1:S2-6. [PubMed]
- Ascher E, Hingorani A, Yorkovich W, et al. Routine preoperative carotid duplex scanning in patients undergoing open heart surgery: is it worthwhile? Ann Vasc Surg 2001;15:669-78. [PubMed]
- Ciccone MM, Bilianou E, Balbarini A, et al. Task force on: 'Early markers of atherosclerosis: influence of age and sex'. J Cardiovasc Med (Hagerstown) 2013;14:757-66. [PubMed]


