Temporary placement of metallic stent could lead to long-term benefits for benign tracheobronchial stenosis
Introduction
Benign tracheobronchial stenosis (BTS) is a common disease extensively influencing the patients’ quality of life. Serious BTS may cause dyspnea, respiratory distress, atelectasis, obstructive pneumonia and even early death from suffocation. Endobronchial tuberculosis (EBTB), post-intubation tracheal stenosis (PITS) and post-tracheostomy tracheal stenosis (PTTS) make up the majority causes of BTS in China (1). Surgical resection and reconstruction is the gold standard of therapy (2,3). However, a proportion of patients who are not surgical candidates need endoscopic interventions such as stenting, balloon dilatation, electrocautery and laser (4-6).
Permanent placement of airway stent for tracheobronchial stricture can relieve symptoms immediately and was widely used in the patients with BTS. However, stenting in these patients was pretty problematic due to their long life expectancies. For metallic stents, granulation tissue ingrowth after long-term implantation frequently occurs (7,8), resulting in restenosis that requires repeated endoluminal procedures to maintain stent patency or removal. Stent fracture, esophagorespiratory fistula and bacterial colonization were the other three common complications of metallic stent (9,10). More than one-fourth of patients presented removal indications (11-13). But actually, once metallic stent was deployed, it was difficult to remove (11,14). In view of these disadvantages, the permanent placement of metallic stent was not recommended for BTS unless silicone stents were unsuitable (15). For silicone stent, stent migration was the commonest complication after long-term placement (16-18). And its disruption of mucociliary clearance and minor cross-sectional airway diameter can lead to high risk of mucus plugging (19,20).
Based on these potential disadvantages and limitations of permanent stenting, we designed a novel uncovered retrievable self-expansible metallic stent (SEMS) which was temporarily placed in BTS patient. This retrospective study was conducted to explore whether temporary stenting could lead to long-term benefits for BTS patients.
Patients and methods
Patients
Between December 2008 and April 2011, the BTS patients who received temporary stenting were included in this study. However, the following patients were excluded: previously treated by stents and balloon dilation, strictures caused by external compression, strictures with acute inflammations, and patients with other serious pulmonary or cardiac comorbidities. Informed consent form was obtained from each patient; and our institutional review board approved this study.
Stents
Stents (Figure 1) [Micro-Tech (Nanjing) Co., Ltd, China] were woven from a single thread of nitinol wire in a tubular configuration. To make the stent retrievable, each end of the stent was wound with a nitinol loop, grasping which could remove or relocate the stent.
Procedure
Before stenting, the internal diameter of stenosis segment was measured by computed tomography (CT). Respiratory function was evaluated by Hugh-Jones scale, percentage of forced expiratory volume in one second (FEV1%) to predictive value and 6-minute walk test (6MWT).
Prior to placement, a stent with suitable size was selected in order to completely cover the length of stricture and keep it completely patent. Topical anesthesia and intravenous sedations were used during the placements of 47 stents, and another two stents were placed under general anesthesia as these two patients had high risks of asphyxia during the procedure. Under flexible bronchoscopic, stent compressed and loaded in a sheath was located cross the stricture through a guidewire. After placement, all patients underwent conventional radiography to verify the location and patency of the stent on day 1, 3 and 7. Bronchoscopy was performed on day 2 and 7 or when complications or symptom recurrence occurred. Stent-related complications were evaluated and the incidence of granulation tissue growth or stent migration or stent mal-expansion was analyzed. Once granulation tissue grew, it was eliminated by mechanical clearance in order to prevent it covering the stent. All stents with mal-expansion were replaced by the stents with stronger expandability, in order to completely open the airway stenosis.
Stents were usually removed in 2–4 weeks after placement. Stent removals were all performed under topical anesthesia and intravenous sedations. Flexible bronchoscopy was inserted through mouth, and then foreign body forceps was inserted through working channel. After grasping the nitinol loop at distal end, the forceps were pulled out together with scope. The removed stent was restored in an expanded shape to check its integrity.
Technical success was defined as successful placement or removal of the stents without any major procedure-related complications.
Follow-up and outcomes
After stent removal, clinical examination and bronchoscopy or CT scan were performed at 1 week, 1 month, and 3 months, and then at every 6 months, or when symptom recurrence occurred. The internal diameter of stricture site was measured. Respiratory function was evaluated by Hugh-Jones scale, FEV1% and 6MWT. During the follow-up period, patients were recommended to receive tailored treatment option, such as balloon dilation, permanent placement of silicone stent, electrocautery and cryotherapy once symptom recurrence occurred.
Symptom recurrence-free survival (SRFS) was defined as the time without return of symptoms and identified airway restenosis under bronchoscopy or CT scan after temporary stenting.
Statistical analysis
Statistical analysis was conducted using STATA software version 11.0 (StataCorp, College Station, TX). The P value less than 0.05 was considered to indicate a significant difference. The pre-operation and follow-up internal diameters of the stricture sites, FEV1% and 6MWT were analyzed using the paired student’s test. The Wilcoxon signed-rank test was used to assess the pre-operation and follow-up Hugh-Jones scales. Recurrence-free survival after temporary stenting was calculated using the Kaplan-Meier method. Multivariate logistic regression estimated the prognostic factors for the long-term outcomes of temporary stenting in BTS patients.
Results
Patients
A total of 40 consecutive patients with BTS (17 men, 23 women; median age 41 years, range, 18–79 years) were included from December 2008 to April 2011 in our institution (Table 1). The etiologies of the 40 BTS were EBTB (n=22), PTTS (n=10), PITS (n=6) and post radiotherapy stenosis (n=2). The lesion sites included trachea (n=26), left main bronchus (n=12), and right main bronchus (n=4). The stenosis in two patients involved lower trachea and main bronchus and they were placed two SEMS respectively.
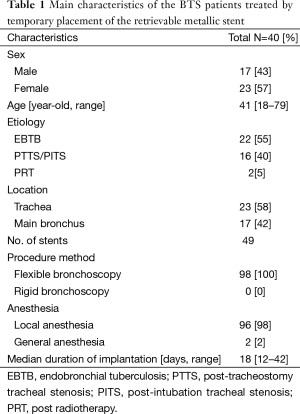
Full table
Procedures
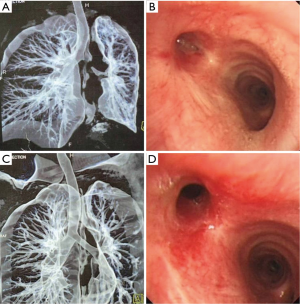
A total of 49 stents were successfully placed and removed in 40 patients under flexible bronchoscopy (Figure 2). All stents were removed integrally after temporary placement for a median of 18 days (range from 12 to 42 days). The technical success rate was 100%. Procedure related complications mainly included minor bleeding and post-bronchoscopy fever without evidence of infection.

During the period of stenting, the overall incidence of stent-related complications was 26.5% (13/49), including 16.3% (8/49) of granulation tissue growth, 6.1% (3/49) of stent migration, and 4.1% (2/49) of stent mal-expansion. Among these patients, four with recurrent granulation tissue growth, one with stent migration and both of the patients with stent mal-expansion experienced stent replacements.
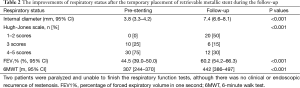
Respiratory status
After a median 27 months follow-up period after stent removal (data cutoff, December 31, 2013), the internal diameter of strictures (follow-up: 7.4 mm, 95% CI, 6.6–8.1 mm; pre-operation: 3.8 mm, 95% CI, 3.3–4.2 mm; P<0.001) (Figure 3), Hugh-Jones scale (Z=4.771; P<0.001), 6MWT (follow-up: 442 m, 95% CI, 386–497 m; pre-operation: 307 m, 95% CI, 244–370 m; P<0.001) and FEV1% (follow-up: 60.2%, 95% CI, 54.2–66.3%; pre-operation: 44.5%, 95% CI, 39.0–50.0%; P<0.001) were significantly improved compared with pre-operation (Table 2).
Full table
Symptom recurrence-free survival (SRFS)
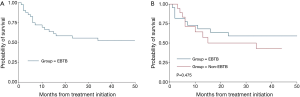
During the period of follow-up, a total of 22 patients were free of symptom recurrence (55%). As shown in Figure 4A, the overall 3-year SRFS rate was 52.0%. According to the etiology, the 3-year SRFS rates were 59.1% and 42.9% in the patients with EBTB and non-EBTB, respectively (Figure 4B). And the results of multivariate logistic regression suggested that granulation tissue growth and tracheobronchial malacia were independent prognostic factors for the long-term outcomes of temporary stenting.
Discussion
This study with a long-term follow-up period demonstrated that (1) temporary placement of retrievable uncovered SEMS was safe for BTS patients and (2) short-term stenting could significantly improve the symptoms and respiratory status of the BTS patients in the long term after stent removal.
The mechanism of the long-term efficacy of temporary stenting might be similar to that of balloon dilation. The stent provided a continuous dilation effect against the wall of the stricture, but the dilating period was much longer and the strength was softer than that of balloon. The serious complications associated with violent dilation such as tracheobronchial tear and massive hemoptysis (20,21) can be avoided by temporary stenting. Furthermore, the expanded stent could provide a chance for the stricture to remodel or heal. The longer dilation maintained, the better long-term efficacy might be. It was indicated in Kim’s study (22), the recurrence rate of 2 months stenting group was significantly higher than that of 6 months stenting group (83.3% vs. 41.7%). However, our study with a similar follow-up period showed that only 2–4 weeks stenting can lead to less recurrence rate than that in the 2 months stenting group in Kim’s study (45.0% vs. 83.3%), the reason of which might be that the patients in Kim’s study were those failed with balloon dilation before. They were refractory to the dilation treatments, including temporary stenting. Under this circumstance, a longer stenting period was optimal. On the other hand, however, why didn’t we place the stent longer to get better benefit? The placement of SEMS with a longer period could lead to higher risks of serious granulation tissue growth, stent fracture, lengthening luminal damage, inciting subglottic strictures, and causing esophagorespiratory fistula (7-10). The stent-related complications in our study were mild, but with a relative high incidence (26.5%), even the median stenting period was only 18 days. Weighting the benefit and risk of the temporary placement of metallic stent, 2–4 weeks stenting period was recommended. The results demonstrated that this kind of temporary stenting not only could lead to a satisfied long-term efficacy, but also had avoided the long-term serious complications caused by metallic stents.
The stent used in this study was a novel retrievable SEMS, which included all the advantages of common SEMS, such as greater ease of placement, greater cross-sectional airway diameter, less migration rate, less disruption of mucociliary clearance and stronger dilating force compared with silicone stent (23). Moreover, it had overcome the problem caused by removal and relocation of metallic stent, which was the significant reason that metallic stent was not recommended to be applied in patients (15). Even when metallic stent related serious complications occurred, it can be easily removed. In our experiences, almost all of the stents were easily successfully placed and removed using the flexible bronchoscopy (100%) under local anesthesia (98%), without any major procedure-related complications. The removal procedure did not cause massive bleeding, mucosal tears and retained stent fragments. All stents were integrally removed.
The outcome benefits of temporary stenting were estimated by respiratory status [including respiratory anatomy (internal diameter) and respiratory function (FEV1%, 6MWT and Hugh-Jones scale)] and SRFS in our study. The results showed that all of the endpoints were significantly improved during the follow-up period. Although the respiratory status was not completely restored to normal, it was enough for the physiological drive to keep the patients stay away from dyspnea-recurrence. BTS was a chronic disorder that can hardly reach anatomic cure by interventional procedures except for surgical methods. Thus, the primary endpoint of temporary stenting for inoperable patients might be symptom-recurrence-free survival which should be placed more emphasis on.
Anyway, part of BTS patients were refractory to the treatment of temporary stenting in our study, which might be associated with the etiologies, length of stenting period, airway malacia and secondary granulation tissue growth. Patent airway was normally maintained by the intact tracheobronchial cartilaginous rings. However, it can be damaged by tracheobronchial inflammation and long-term ischemia, leading to airway malacia. The results of multivariate logistic regression in our study suggested that tracheobronchial malacia might be an independent prognostic factor for the long-term efficacy of temporary stenting besides granulation tissue growth. Pre-operation assessment such as thin-slice CT scan and endobronchial ultrasound (EBUS) can be performed to detect the severities of the damages of tracheobronchial cartilaginous rings in order to select the patients with better predicted outcomes. In addition, this study showed that the 3-year SRFS rate of EBTB patients was likely to be higher than that of non-EBTB patients (59.1% vs. 42.9%). As a result, temporary stenting should be applied in the better selected BTS patients.
The limitations of this study included retrospective design, relatively small sample size of each cause of tracheobronchial stenosis. Further perspective investigations with larger sample sizes were undergoing.
In conclusion, temporary placement of the retrievable SEMS not only avoided the main disadvantages of permanent stenting, but also presented satisfied long-term benefits for BTS patients. It might be an alternative treatment for patients with BTS.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Li YQ, Li Q. Analysis of etiopathogenisis of benign central airway stenosis in 386 cases. J Navy Med 2007;28:307-9.
- Krajc T, Janik M, Benej R, et al. Urgent segmental resection as the primary strategy in management of benign tracheal stenosis. A single center experience in 164 consecutive cases. Interact Cardiovasc Thorac Surg 2009;9:983-9. [PubMed]
- D'Andrilli A, Ciccone AM, Venuta F, et al. Long-term results of laryngotracheal resection for benign stenosis. Eur J Cardiothorac Surg 2008;33:440-3. [PubMed]
- Rubin AE, Wang KP, Liu MC. Tracheobronchial stenosis from acid aspiration presenting as asthma. Chest 2003;123:643-6. [PubMed]
- Ciccone AM, De Giacomo T, Venuta F, et al. Operative and non-operative treatment of benign subglottic laryngotracheal stenosis. Eur J Cardiothorac Surg 2004;26:818-22. [PubMed]
- Bolliger CT, Sutedja TG, Strausz J, et al. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J 2006;27:1258-71. [PubMed]
- Saad CP, Murthy S, Krizmanich G, et al. Self-expandable metallic airway stents and flexible bronchoscopy: long-term outcomes analysis. Chest 2003;124:1993-9. [PubMed]
- Chung FT, Lin SM, Chou CL, et al. Factors leading to obstructive granulation tissue formation after ultraflex stenting in benign tracheal narrowing. Thorac Cardiovasc Surg 2010;58:102-7. [PubMed]
- Gottlieb J, Fuehner T, Dierich M, et al. Are metallic stents really safe? A long-term analysis in lung transplant recipients. Eur Respir J 2009;34:1417-22. [PubMed]
- Kapoor BS, May B, Panu N, et al. Endobronchial stent placement for the management of airway complications after lung transplantation. J Vasc Interv Radiol 2007;18:629-32. [PubMed]
- Fruchter O, Raviv Y, Fox BD, et al. Removal of metallic tracheobronchial stents in lung transplantation with flexible bronchoscopy. J Cardiothorac Surg 2010;5:72. [PubMed]
- Doyle DJ, Abdelmalak B, Machuzak M, et al. Anesthesia and airway management for removing pulmonary self-expanding metallic stents. J Clin Anesth 2009;21:529-32. [PubMed]
- Noppen M, Stratakos G, D'Haese J, et al. Removal of covered self-expandable metallic airway stents in benign disorders: indications, technique, and outcomes. Chest 2005;127:482-7. [PubMed]
- Rampey AM, Silvestri GA, Gillespie MB. Combined endoscopic and open approach to the removal of expandable metallic tracheal stents. Arch Otolaryngol Head Neck Surg 2007;133:37-41. [PubMed]
- Lund ME, Force S. Airway stenting for patients with benign airway disease and the Food and Drug Administration advisory: a call for restraint. Chest 2007;132:1107-8. [PubMed]
- Ryu YJ, Kim H, Yu CM, et al. Use of silicone stents for the management of post-tuberculosis tracheobronchial stenosis. Eur Respir J 2006;28:1029-35. [PubMed]
- Gildea TR, Murthy SC, Sahoo D, et al. Performance of a self-expanding silicone stent in palliation of benign airway conditions. Chest 2006;130:1419-23. [PubMed]
- Dumon JF. A dedicated tracheobronchial stent. Chest 1990;97:328-32. [PubMed]
- Dutau H, Cavailles A, Sakr L, et al. A retrospective study of silicone stent placement for management of anastomotic airway complications in lung transplant recipients: short- and long-term outcomes. J Heart Lung Transplant 2010;29:658-64. [PubMed]
- Hautmann H, Gamarra F, Pfeifer KJ, et al. Fiberoptic bronchoscopic balloon dilatation in malignant tracheobronchial disease: indications and results. Chest 2001;120:43-9. [PubMed]
- Kim JH, Shin JH, Song HY, et al. Tracheobronchial laceration after balloon dilation for benign strictures: incidence and clinical significance. Chest 2007;131:1114-7. [PubMed]
- Kim JH, Shin JH, Song HY, et al. Benign tracheobronchial strictures: long-term results and factors affecting airway patency after temporary stent placement. AJR Am J Roentgenol 2007;188:1033-8. [PubMed]
- Chin CS, Litle V, Yun J, et al. Airway stents. Ann Thorac Surg 2008;85:S792-6. [PubMed]