Radical resection of right upper lung cancer using uniportal video-assisted thoracic surgery with non-intubated anesthesia
Introduction
The application of video-assisted thoracic surgery (VATS) has been regarded as a major breakthrough in the field of the thoracic surgery; after over 20 years of development with the efforts of thoracic surgeons worldwide (1), VATS has become a standard treatment and a reasonable choice for patients with non small cell lung cancer. Since 2012, as long as the patient has no contraindication of anatomy and operation and don’t violating the principle of chest tumor treatment and surgery.
VATS technology has been used in a large variety of thoracic diseases including lung cancer, pneumothorax and other common diseases. A number of studies have found no significant difference in operation time, intraoperative bleeding volume, or lymph node dissection between VATS and conventional thoracotomy in radical resection of lung cancer. Other advantages such as minimal trauma, better protection of lung function, less postoperative pain, faster postoperative recovery, shorter hospitalization time and reduced expenses have also been noted.
Traditional general anesthesia by tracheal intubation can provide good operative vision and control for thoracic surgery, however the use of tracheal intubation and the accompanying necessary muscle relaxants can cause a series of postoperative complications such as irritating cough, lung injury, lung expansion injury, bronchial spasm, etc. (2-4). Even with the advancements made in VATS, general anesthesia under tracheal intubation remains the most common method used in surgery; this has led to the emergence of the “little surgery, big anesthesia” phenomenon. This phenomenon does not coincide with the overall concept of minimally invasive thoracic surgery and is severely hampering the amelioration of minimally invasive thoracic surgery.
The recent development of non-intubated anesthesia has given us options to stop the occurrence of the “little surgery, big anesthesia” phenomenon. The use of this technique can avoid complications caused by intubated anesthesia and assist in a faster recovery of patients; it has aroused the interest of scholars worldwide. Literature regarding the use of this technique has steadily emerged including not only case reports, but also a number of systematic studies including, but not limited to, treatment of pneumothorax, tracheal and carinal sleeve resections, mediastinal tumor resection, lung volume reduction surgery, lobectomy, and segmental resection (5).
Traditional VATS is most commonly associated with the use of multiple incisions (two, three or four). There are many layers of muscle on the posterior axillary line. The equipment activities can only be carried out in a relatively small space, and intercostal nerve may suffer from crush injury of the intercostal nerve may occur as a result of the repeated use of instruments operation, all this can lead to a series of problems for patients such as increased postoperative pain, paraesthesia and mild dyskinesia. The reduction of the number of operating ports located along or on the posterior axillary line may cause a reduction in the occurrence of such issues thereby improving the postoperative quality of life. In addition a reduction in the number of ports can lead to a shorter operation time and a decrease in the volume of blood lost as a result of the shortened time of preparation required for multiple incisions and associated suturing of these ports.
All instruments are operated through one single incision during a uniportal procedure. The incision is most commonly located on the anterior axillary line, as there are less layers of muscle on the anterior axillary line, the influence of the sensation and movement is smaller for patients resulting in only mild postoperative pain. The hilar structure can be better exposed to ensure the safety of the hilar vessels. Even when faced with some intraoperative difficulties, such as the need to transfer to thoracotomy because of intraoperative hemorrhage, uniportal VATS can save time for surgeons (6-8).
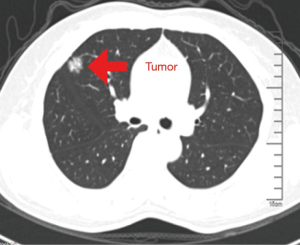
A 55-year-old female was admitted to our hospital. CT scan revealed a nodule in the anterior segment of the right upper lobe with superficial lobulated lesion and short burr-like boundaries (Figure 1). Because of the small size and placement of the lesion, peripheral nodule in the right-upper-lobe, the patient received a uniportal VATS resection with non-intubated anesthesia (Figure 2).
Clinical data
A 55-year-old female patient presented with pain in the right side of the chest 2 weeks ago a nodule located in the right upper lobe was discovered 7 days later. The patient had no history of other chronic diseases.
The chest computed tomography (CT) indicated a circular-like nodule about 1.8 cm × 1.6 cm in the anterior segment of the right upper lobe; the lesion had uneven density, superficial lobulated lesion and short burr-like boundaries. In addition, small dot-like nodules were seen around the lesion. There was no stenosis or expansion of the trachea and bronchus nor were there enlarged mediastinal lymph nodes. Enhanced cranial magnetic resonance imaging (MRI), general bone scanning, and enhanced abdominal CT showed no evidence of tumor metastasis. The patient’s preoperative diagnosis was lung cancer of the right-upper-lobe, T1aN0M0, phase IA. The results of pulmonary function test were quite satisfactory: forced expiratory volume in 1 second (FEV1) was 1.89−89%. The cardiac function test showed aortic and mitral regurgitation (mild) and diastolic insufficiency, ejection fraction (EF): 72%. The systolic function of the left ventricle was normal.
Preoperative evaluation
For patients whose primary diagnoses are lung cancer, we utilize enhanced cranial MRI, general bone scanning, and enhanced abdominal CT to exclude distant tumor metastasis. We also evaluate the cardiorespiratory function, pulmonary ventilation function, cardiac function test, and coronary CT when necessary. Lobectomy is safe for patients who have appropriate pulmonary ventilation functions (preoperative: FEV1 >1.5 L, FEV1/FVC >50%; postoperative: FEV1 >0.8 L).
Operative techniques
Anesthesia and body posture
The anesthesia procedure was epidural block and thoracic intercostal nerve block. The body posture was left recumbent position.
Operative incision
The operative incision was made on the right anterior axillary line in the 4th intercostal space. The incision was 4 cm.
Operating procedure
Step 1: A wedge resection of the lesion in the right-upper-lobe was performed first. Intraoperative frozen biopsy confirmed infiltrating adenocarcinoma, at which point a radical resection of right upper lobe was planned.
Step 2: We separated the oblique fissure and educed posterior ascending branches and branches of the arteries of right upper lobe, closured it with a hem-o-lock and mutilated it with an ultrasonic knife.
Step 3: We educed right upper lobe bronchus. Next we closured it with ECHELON FLEX™ Powered ENDOPATH® Stapler (Johnson & Johnson Investment Co. Ltd., NJ) using ECR45G (Green) and made sure the median lobe had no atelectasis by ventilating. Resection of right upper lobe immediately followed.
Step 4: The horizontal fissure of right lung was separated using ECHELON FLEX™ Powered ENDOPATH® Stapler using ECR45D (Gold) and mutilated right upper lobe veins.
Step 5: Lymph node dissection was performed (group 2, 4, 7 and 10).
Step 6: An intrathoracic chest drainage tube was placed and the incision was sutured.
Postoperative care
Postoperative treatments including anti-infection, phlegm eliminating, and broncho relaxing are routine. The patient was required to coughing exercise actively. The intrathoracic drainage tube was removed 3 days later. The patient was discharged to post-hospital care 7 days later.
Pathologic diagnosis
The mass in the right-upper-lobe was confirmed invasive adenocarcinoma, which wan mainly papillary, accompanied with part of acinous components. The tumor invaded the visceral pleural. Pathological results confirmed the bronchial stump as negative, All dissected lymphnodes were also confirmed negative for adenocarcinoma (group 2, 4, 7 and 10). Postoperative diagnosis was invasive adenocarcinoma of the right-upper-lobe, T1aN0M0, phase IA.
Comments
Radical resection of lung cancer under VATS has been confirmed safe and feasible for cancer patients in good physical condition. Non-intubated anesthesia has also been confirmed as safe and feasible in a number of studies during a large variety of procedures. Our patient was in relatively good physical condition, with only a small nodule in the peripheral lung; because of the complications associated with the use of tracheal intubation, we selected the use of non-intubated anesthesia. The body of literature regarding indications for VATS and non-intubated methods is constantly expanding, and the majority of literature supports the use of these techniques in younger patients or in patients with good physical condition. Reducing the length of postoperative recovery, the level of postoperative pain, and give a patient a better postoperative quality of life is the cornerstone of the development of minimally invasive surgery; and the benefits associated with uniportal and non-intubated techniques are a major development in this sense. A faster recovery and reduction in the length of hospital stay are only a few of the benefits recorded for patients who have received such operations. Patients recover quickly and reduce the length of hospital stay. Patients under anesthesia with non-tracheal intubation are in the state of spontaneously breathing. To reduce the cough reflex in patients with spontaneously breathing and the increase of respiratory activity caused by pain, we can block the cranial nerve in the thoracic cavity. We can also reduce intraoperative pain reflex by blocking the intercostal nerve. All this can make us fell like doing the operation under general anesthesia by tracheal intubation. We may pay attention to the cooperation between instruments and the placement angle of the instruments in order to avoid accidental injury during a radical resection of lung cancer with uniportal VATS. It’s effective to treat large vessels and bronchus with the use of a rotating-head endoscopic stapler such as ECHELON FLEX™ Powered ENDOPATH® Stapler. However, for small vessels, the Hem-o-lock can be used to reduce the risk of the important tissue damages caused by inappropriate placement angle of the endoscopic stapler.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Lewis RJ, Caccavale RJ, Sisler GE, et al. One hundred consecutive patients undergoing video-assisted thoracic operations. Ann Thorac Surg 1992;54:421-6. [PubMed]
- Mineo TC. Epidural anesthesia in awake thoracic surgery. Eur J Cardiothorac Surg 2007;32:13-9. [PubMed]
- Fitzmaurice BG, Brodsky JB. Airway rupture from double-lumen tubes. J Cardiothorac Vasc Anesth 1999;13:322-9. [PubMed]
- Huang CC, Chou AH, Liu HP, et al. Tension pneumothorax complicated by double-lumen endotracheal tube intubation. Chang Gung Med J 2005;28:503-7. [PubMed]
- Hung MH, Hsu HH, Cheng YJ, et al. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014;6:2-9. [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [PubMed]
- Salati M, Brunelli A, Rocco G. Uniportal video-assisted thoracic surgery for diagnosis and treatment of intrathoracic conditions. Thorac Surg Clin 2008;18:305-10. vii. [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [PubMed]
- Wang W, Peng G, Guo Z, et al. Uniportal video-assisted thoracoscopic surgery right upper lobectomy with systematic lymphadenectomy under non-intubated anesthesia. Asvide 2015;2:161. Available online: http://www.asvide.com/articles/739