Early stage lung cancer with nodal involvement occult to PET-CT: treat the image or treat the disease?
Non-small cell lung cancer (NSCLC) over past 10 years has become the first cancer-related cause of death both in man and women with approx. about 1.3 million new cases and 1.2 million deaths each year worldwide (1-3). Strategies offered to NSCLC patients are vast and highly depend on lung cancer staging and in particular mediastinal lymph nodes status. TNM staging model accepted by IASLC in 2007 clearly identifies the benefits of particular therapies when tailored individually to cancer patients (4). Since then it was modified and adjusted in compliance to developing understanding of lung cancer biology and growing diagnostic accuracy. However, main principles remain intact with surgery representing most appropriate modality for early stage tumors (lung involvement ± hilar nodes) and oncologic management for metastatic disease. Evaluation of mediastinal lymph nodes involvement indicating metastatic progression and in turn questionable surgery benefit has therefore become crucial and of great clinical importance.
PET-CT is a unique tool combining anatomical assessment of computed tomography (CT) and positron emission tomography (PET) allowing for functional process imaging inferences that has gained wide acceptance in USA and Western Europe over past few years with its clinical relevance and reliability expected to further advance. While image obtained in a combination with 96% accuracy, has been shown to overcome the limitations of single modalities (59% and 88% accuracy for CT and PET respectively) during mediastinal lymph node staging for N1-N2 disease (5), many data indicate that accuracy of PET-CT alone is insufficient to assess mediastinal nodal involvement in patients with suspected resectable early stage NSCLC (6,7). The clinical significance of such inconsistency is not to be underestimated as for early stage T1-2N0M0 NSCLC surgical resection is considered a treatment of choice and is associated with better outcomes and prognosis as compared to other modalities (8,9). On the other hand, 20–30% of the stage I NSCLC patients are deemed medically inoperable or refuse surgery and may be offered radiation therapy [standard external beam-(EBRT) or stereotactic ablative-radiation therapy (SABR)] (10).
In the August 2014 issue of TCR, Paravati and colleagues (11) assessed the incidence of pN1-pN2 among those clinically staged with PET-CT as cN0 lung cancer and identified predictors of nodal disease occult to PET-CT. Authors report negative predictive values (NPVs) of PET-CT of 92% for N2 (mediastinal) disease (133/144) and 90% for N1 bronchopulmonary and hilar) disease (130/144). Moreover, the NPVs for mediastinal metastases were 95% in T1 disease (93/98) and 87% in T2 disease (40/46). Additionally, in a multivariate logistic regression analysis, tumor size, central tumor location and age at the time of surgical resection were demonstrated to be strong predictive factors associated with occult nodal disease. Interestingly, only two out of 55 patients (4%) with tumor diameter ≤2.0 cm were found to have occult nodal disease. However, 7 of 43 patients (16%) with tumor diameters between 2 and 3 cm and 10 of 46 patients (22%) with tumor greater than 3 cm were found to have occult nodal disease at pathological dissection. This findings support the necessity to subclassify T1 factor and in the same time justify the recent amendments to TNM classification (8th ed. The IASLC Lung Cancer Staging Project Proposal) (12). Indeed, T1 will be subclassified into T1a (≤1 cm), T1b (>1 to ≤2 cm) and T1c (>2 to ≤3 cm) as survival analyses adjusted by histological type, gender, region and age showed that capacity of tumor size to separate tumors of different prognosis was greater than in previous analyses.
Perhaps the most interesting aspect of the study by Paravati and colleagues is the distinguishing of negative predictive values for N1 and N2 disease, N1 disease alone and N2 disease alone (‘skip metastases’). Indeed, N2 disease alone has been shown to be associated with better prognosis than the more common progression of tumor (lung→N1→N2) (13). Whether improved outcomes in these patients result from lower total burden of the metastatic disease or represent an inherently different process of disease progression remains matter of ongoing debate (14). Again, the implications from this analysis are further reflected in the proposal for TNM revision by the IASLC Lung Cancer Staging Project which will under rank the current N2 disease alone. With regard to pathological staging, analyses regarding the prognosis were performed by further dividing N1 into N1 at a single station (N1a) and N1 at multiple stations (N1b), and N2 into N2 at a single station without N1 involvement (N2a1), N2 into N2 at a single station with N1 involvement (N2a2), and N2 at multiple stations (N2b). The survival curves for N1b and N2a2 overlapped each other, and N2a1 had numerically a better prognosis than N1b, though the difference was not significant (15).
Stereotactic ablative radiation therapy is an effective and well-tolerated non-invasive treatment for medically inoperable patients with peripheral NSCLC. Results from prospective and retrospective studies suggest that lung SABR has superior outcomes when compared with conventionally fractionated treatments and is comparable with surgical resection (16). In patients with FDG-PET/CT-based stage I NSCLC however, SABR confers worse locoregional tumor control because of more nodal failures compared with surgery, stressing the need to improve mediastinal and hilar staging; in particular in centrally located primary tumor and known adenocarcinoma (17). Tomahiro et al. found, that in 876 patients with clinical stage I NSCLC the total incidence of mediastinal lymph involvement is 9.1%. They proved no cases with hilar or mediastinal lymph node metastasis only in ground glass opacity predominant tumors (18).
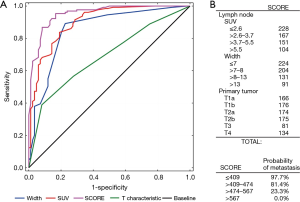
As promptly noticed by Paravati (11) overall underestimation of true pathological stage by integrated PET-CT is not uncommon (19), particularly with larger and centrally located tumors, characteristics found to be associated with occult nodal disease (11). PET-CT image alone should therefore never be considered definitive for early NSCLC staging. In a recently available analysis (20), we were able to demonstrate that single factor tests: nodes’ characteristics: length, width, volume, maximal standard uptake value (SUVmax), topographical location; and primary tumor characteristics: size, location and TNM classification although linearly correlated with mediastinal involvement in retrospective study, the established cutoffs all failed in prospective validation on an unmatched group of patients. On the other hand, when considered as composite, node’s SUV and size along with primary tumor (T) characteristics were the strongest predictors of metastatic involvement regardless of test employed in artificial neural network gaining the NPV of 94–95%. Additionally, logistic regression analysis allowed for construction of scoring model with certain parameters corresponding to risk thresholds of metastatic disease (Figure 1).
Paravati and colleagues present an excellent study of 144 patients closely reflecting recent advancements in mediastinal nodal staging in early stage NSCLC. They conclude that with NPV ranging from 90% to 98% in PET-CT for T1 descriptor and peripheral location there exists a potential role for non-surgical treatment of lung cancer such as SABR without prior routine pathological nodal staging performed. Before this is confirmed in a randomized trial, invasive mediastinal staging should be considered and consequences of missing the occult nodal metastases on PET-CT made clear to patients considering non-surgical options in particular in absence of contraindications for surgery.
Further reading
- Paravati AJ, Johnstone DW, Seltzer MA, et al. Negative predictive value (NPV) of FDG PET-CT for nodal disease in clinically node-negative early stage lung cancer (AJCC 7th ed T1-2aN0) and identification of risk factors for occult nodal (pN1-N2) metastasis: implications for SBRT. Transl Cancer Res 2014;3:313-9.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. CA Cancer J Clin 2005;55:74-108. [PubMed]
- Pisani P, Bray F, Parkin DM. Estimates of the world-wide prevalence of cancer for 25 sites in the adult population. Int J Cancer 2002;97:72-81. [PubMed]
- Feins RH, Reed CE, LoCicero III J, Shields TW, 2009. General Thoracic Surgery. Wolters Kluwer Health| Lippincott Williams & Wilkins. Accessed: 15th Dec 2015. Available online: http://www.lww.com/Product/9780781779821
- Rusch VW, Crowley J, Giroux DJ, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the N descriptors in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2007;2:603-12.
- Vansteenkiste JF, Stroobants SG, De Leyn PR, et al. Mediastinal lymph node staging with FDG-PET scan in patients with potentially operable non-small cell lung cancer: a prospective analysis of 50 cases. Leuven Lung Cancer Group. Chest 1997;112:1480-6. [PubMed]
- Schmidt-Hansen M, Baldwin DR, Zamora J. FDG-PET/CT imaging for mediastinal staging in patients with potentially resectable non-small cell lung cancer. JAMA 2015;313:1465-6. [PubMed]
- Schmidt-Hansen M, Baldwin DR, Hasler E, et al. PET-CT for assessing mediastinal lymph node involvement in patients with suspected resectable non-small cell lung cancer. Cochrane Database Syst Rev 2014;11:CD009519. [PubMed]
- Khullar OV, Liu Y, Gillespie T, et al. Survival After Sublobar Resection versus Lobectomy for Clinical Stage IA Lung Cancer: An Analysis from the National Cancer Data Base. J Thorac Oncol 2015;10:1625-33. [PubMed]
- Yu JB, Soulos PR, Cramer LD, et al. Comparative effectiveness of surgery and radiosurgery for stage I non-small cell lung cancer. Cancer 2015;121:2341-9. [PubMed]
- Boily G, Filion É, Rakovich G, et al. Stereotactic Ablative Radiation Therapy for the Treatment of Early-stage Non-Small-Cell Lung Cancer: CEPO Review and Recommendations. J Thorac Oncol 2015;10:872-82. [PubMed]
- Paravati AJ, Johnstone DW, Seltzer MA, Johnstone CA. Negative predictive value (NPV) of FDG PET-CT for nodal disease in clinically node-negative early stage lung cancer (AJCC 7th ed T1-2aN0) and identification of risk factors for occult nodal (pN1-N2) metastasis: implications for SBRT. Transl Cancer Res 2014;3:313-9.
- Rami-Porta R, Bolejack V, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for the Revisions of the T Descriptors in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2015;10:990-1003.
- Li H, Hu H, Wang R, et al. Lung adenocarcinoma: Are skip N2 metastases different from non-skip? J Thorac Cardiovasc Surg 2015;150:790-5. [PubMed]
- Rusch VW. Nodal metastases in non-small cell lung cancer: Hop, skip, or jump? J Thorac Cardiovasc Surg 2015;150:765-6. [PubMed]
- Asamura H, Chansky K, Crowley J, et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the Revision of the N Descriptors in the Forthcoming 8th Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2015;10:1675-84.
- Roach MC, Videtic GM, Bradley JD, et al. Treatment of Peripheral Non-Small Cell Lung Carcinoma with Stereotactic Body Radiation Therapy. J Thorac Oncol 2015;10:1261-7. [PubMed]
- van den Berg LL, Klinkenberg TJ, Groen HJ, et al. Patterns of Recurrence and Survival after Surgery or Stereotactic Radiotherapy for Early Stage NSCLC. J Thorac Oncol 2015;10:826-31. [PubMed]
- Haruki T, Aokage K, Miyoshi T, et al. Mediastinal nodal involvement in patients with clinical stage I non-small-cell lung cancer: possibility of rational lymph node dissection. J Thorac Oncol 2015;10:930-6. [PubMed]
- Mattes MD, Weber WA, Foster A, et al. A Predictive Model for Lymph Node Involvement with Malignancy on PET/CT in Non-Small-Cell Lung Cancer. J Thorac Oncol 2015;10:1207-12. [PubMed]
- Wnuk P, Kowalewski M, Małkowski B, et al. PET-CT derived Artificial Neural Network can predict mediastinal lymph nodes metastases in Non-Small Cell Lung Cancer patients. Preliminary report and scoring model. Q J Nucl Med Mol Imaging 2014. [Epub ahead of print]. [PubMed]


