Esophageal perforation following cervical mediastinoscopy: a rare serious complication
Introduction
Cervical mediastinoscopy is commonly performed with minimal morbidity and mortality. However, this procedure is not without risks, with potential injury to adjacent blood vessels and the tracheobronchial tree. Albeit rarely reported, injury to the esophagus also can occur due to lack of visualization and overly aggressive tissue sampling. This complication can be associated with high rates of morbidity and mortality especially if not diagnosed and treated in a timely manner.
Case presentation
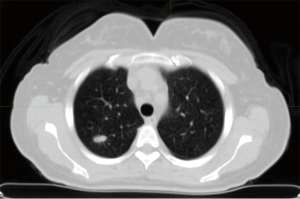
A 57-year-old woman presented with intermittent fevers, dry cough, and night sweats. Additional symptoms included loss of appetite and a ten-pound weight loss over the previous 3 weeks. Her past medical history included hypertension, ex-smoker (1 pack-per-day for 30 years), and lumpectomy for a benign breast mass. Upon presentation, she was admitted to an outside hospital for worsening fevers. A chest X-ray (CXR) revealed a right upper lobe (RUL) 1.5 cm nodule and follow up positron emission tomography/computed tomography (PET/CT) scan demonstrated fluorodeoxyglucose (FDG) uptake in mediastinal, retrohepatic and periportal lymph nodes as well as a 1.8 cm FDG avid RUL nodule (Figure 1). A bone marrow biopsy was nondiagnostic, and the decision was made to sample the mediastinal lymph nodes.
The patient was admitted day of surgery and underwent a cervical mediastinoscopy under general anesthesia. Biopsies of lymph nodes at levels 7, 4R, and 4L were sent for frozen sectioning. The level 4L specimen returned as skeletal muscle, while the lymph nodes at level 4R and level 7 were negative for tumor. The patient was extubated and taken to the recovery room where a CXR demonstrated no acute pathology (Figure 2A).
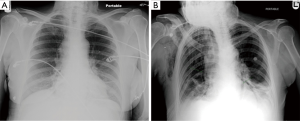
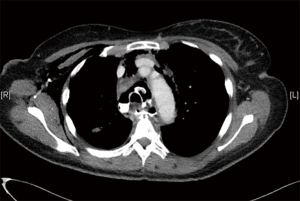
Prior to discharge, the patient complained of severe chest pain and was admitted for observation. By the next morning, she was tachycardic and had subcutaneous emphysema in her neck and upper chest. Additionally, her white blood cell count had increased from 4,400 to 15,600/mcL. A repeat CXR showed pneumomediastinum and subcutaneous emphysema (Figure 2B). A CT scan with oral contrast demonstrated an esophageal perforation with subcutaneous emphysema, contrast in the mediastinum, and bilateral pleural effusions (R>L) (Figure 3). Broad-spectrum antibiotics and intravenous fluids were initiated and emergency surgery was undertaken.
The patient was taken to the operating room and intubated with a double lumen endotracheal tube. A fiberoptic esophagoscope was passed while instilling minimal air into the esophagus. The perforation was identified at 26 cm after which the esophagoscope was advanced beyond and into the stomach. A guide wire was introduced and the esophagoscope withdrawn with identification of the distal and proximal ends of the tear. These were marked on the chest with radiopaque markers and a 120 mm × 18 mm BONASTENTTM (ENDOCHOICE; Atlanta, GA) was deployed under fluoroscopy. Repeat esophagoscopy through the stent showed coverage of the perforation. The patient was then turned and underwent left video-assisted thoracoscopy via a single incision in the seventh intercostal space. Careful inspection demonstrated a small amount of murky fluid but no fibrin deposits. The fluid was aspirated and cultured, the chest was irrigated, a 28Fr chest tube was placed, and the patient was closed.
Next, the patient underwent a right lateral thoracotomy in the fifth intercostal space. Murky fluid, edema, and crepitus were noted overlying the esophagus. The mediastinum was opened and pus was aspirated. Mediastinal debridement and irrigation was then performed. The RUL mass was identified and a generous wedge resection was performed. Two 32 Fr chest tubes were placed, one in the mediastinum and the other in the diaphragmatic sulcus, and the patient was closed. Additionally, a nasogastric tube was passed into the stomach and secured into position. The patient was then transferred intubated to the intensive care unit.
The patient remained stable and was extubated post-operative day 1. Total parenteral nutrition was initiated, and she was transferred to the floor day 4. On postoperative day 6, the nasogastric tube was discontinued and a swallow study demonstrated no extravasation or obstruction. The patient was started on clear liquids. An additional test with methylene blue in her diet showed no leak into the chest tubes. The left chest tube was removed postoperative day 7, and the patient was advanced to a mechanical soft diet. The RUL mass pathology returned positive for neuroendocrine tumor and after consultation with the oncology service, the patient returned to the operating room on postoperative day 13 for a completion RUL lobectomy. She had an uneventful postoperative course and was discharged on antibiotics and a regular diet on postoperative day 10 (postoperative day 23 from original surgery). Six weeks later, the patient returned for stent removal and resumption of a normal diet.
Discussion
Esophageal perforation is associated with considerable mortality with rates as high as 20% if treated early (1). However, these numbers may double if the perforation is diagnosed greater than twenty-four hours after the initial insult. By far the most common cause of perforation is iatrogenic with most injuries occurring during endoscopic procedures (1). Signs and symptoms are often nonspecific and because of this, the clinician must be suspicious for possible esophageal injury. Diagnosis using CXR alone is difficult, although it may demonstrate pneumomediastinum, pleural effusions, or subcutaneous emphysema. Improved diagnostic accuracy is achieved with a barium swallow study or a CT scan with oral contrast.
Cervical mediastinoscopy is important for staging lung cancer as well as aiding the diagnosis of lymphoma, sarcoidosis, and tuberculosis. Additionally, cervical mediastinoscopy has proven to be safe and effective in diagnosing mediastinal masses (2). Low rates of morbidity and mortality have consistently been reported in published series, and the procedure can be performed on an outpatient basis (2,3). However, when a complication does occur it can be severe. Injuries can occur to the azygous vein, pulmonary artery, superior vena cava, innominate artery, and aortic arch resulting in possible emergency surgery. Additionally, injury can occur to the tracheobronchial tree or recurrent laryngeal nerve. An uncommon and rarely reported complication is esophageal perforation (3-5). One series of over 4,000 cervical mediastinoscopies performed at a single institution had one esophageal perforation that was treated by drainage through the mediastinoscopy incision (3). Injury to the esophagus can take place with biopsies at level 4 L lymph nodes or at level 7 as the esophagus courses under the trachea. The surgeon must carefully dissect and visualize lymph nodes prior to taking overly aggressive biopsies. The frozen section report of skeletal muscle in our case was an indication of esophageal injury, though perforation was not diagnosed until later.
A high index of suspicion is necessary to optimize therapy and decrease the associated morbidity and mortality from iatrogenic esophageal perforation. A patient with post-procedural subcutaneous emphysema should have an immediate contrast scan. As in this case, a direct laceration can present with early signs and symptoms, allowing for prompt diagnosis and treatment. However, if thermal damage occurs from coagulation, the injury may have a more insidious onset, possibly taking days or weeks to manifest. In these cases, the injury may be missed as a complication related to the mediastinoscopy itself resulting in a potentially fatal delay in medical care.
Although the management algorithm differs depending on location and time to presentation, early recognition may allow for maintaining esophageal continuity and preventing the need for diversion or resection. If recognized immediately, direct suture repair can be undertaken, thus preventing mediastinal soilage and the deleterious outcomes associated with frank mediastinitis and sepsis. If recognized late, the patient should undergo exclusion of the perforation. A well-described way of achieving exclusion is by covering the injury with an esophageal stent (6,7). The benefits of a stent are its speed and ease; it maintains continuity; and it allows for early oral feeding. After exclusion of the injury, the patient must have all infected spaces adequately drained. In this report, the CT scan showed more effusion and abscess on the right side. Thus, the patient underwent explorative thoracoscopy on the left and a thoracotomy on the right where a more extensive debridement and drainage could be performed.
Conclusions
We present a case of an iatrogenic esophageal perforation as a complication of cervical mediastinoscopy. One must keep in mind the location of the esophagus when performing these procedures and keep a high index of suspicion for injury. Regardless of the cause, early diagnosis and treatment is warranted to give the patient optimal chance for recovery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Brinster CJ, Singhal S, Lee L, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg 2004;77:1475-83. [PubMed]
- Chabowski M, Szymanska-Chabowska A, Skotarczak J, et al. The role of mediastinoscopy in the diagnosis of thoracic disease: one-year single center experience. Adv Exp Med Biol 2015;852:1-4. [PubMed]
- De Leyn P, Lerut T. Videomediastinoscopy. Multimed Man Cardiothorac Surg 2005. doi:. [PubMed]
- Dernevik L, Larsson S, Pettersson G. Esophageal perforation during mediastinoscopy--the successful management of 2 complicated cases. Thorac Cardiovasc Surg 1985;33:179-80. [PubMed]
- Pereszlenyi A Jr, Niks M, Danko J, et al. Complications of video-mediastinoscopy--successful management in four cases. Bratisl Lek Listy 2003;104:201-4. [PubMed]
- Freeman RK, Ascioti AJ, Dake M, et al. An Assessment of the Optimal Time for Removal of Esophageal Stents Used in the Treatment of an Esophageal Anastomotic Leak or Perforation. Ann Thorac Surg 2015;100:422-8. [PubMed]
- Dasari BV, Neely D, Kennedy A, et al. The role of esophageal stents in the management of esophageal anastomotic leaks and benign esophageal perforations. Ann Surg 2014;259:852-60. [PubMed]


