
Outcomes and quality of life after Robot-assisted lobectomy/segmentectomy for lung cancer compared to video-assisted thoracoscopic surgery: both three-port procedures performed by a single surgeon
Introduction
Lung cancer has high morbidity and mortality worldwide, with non-small cell lung cancer (NSCLC) accounting for 85% of cases globally (1). Early screening and concurrent surgical intervention is still the most effective curative method to improve the survival of lung cancer patients (2). Multimodal therapy with either surgery or radical radiotherapy combined with chemotherapy is considered optimal for patients with stage III NSCLC (3). With the continuous development of surgical technology, lobectomy has evolved from being the earliest open large traumatic surgery to a minimally invasive thoracoscopic and robot-assisted procedure. For patients with poor lung function, anatomical segmentectomy can better retain lung function, and is not inferior to lobectomy in terms of overall survival (4).
With the system update iteration and the introduction of other robotic surgical systems, robot-assisted thoracic surgery (RATS) is expected to become a routine technique for major lung resection, together with video-assisted thoracoscopic surgery (VATS) and thoracotomy (5). The safety and efficacy of RATS was still controversial. Some meta-analysis shown that robotics seemed to have longer operative time and higher hospital costs without superior advantages in morbidity rates and oncologic efficiency (6), possibly there was no significant advantage for an established VATS lobectomy surgeon to transition to robotics based on clinical outcomes (7). However, research comparing the effectiveness and safety of RATS versus VATS in lobectomy/segmentectomy for lung cancer is insufficient, and the safety and short-term efficacy of robotic surgery remain controversial. This paper aimed to compare the safety, short-term efficacy, and short-term quality of life (QoL), and delayed complications of three-ports RATS vs. VATS in lobectomy/segmentectomy at 6 weeks postoperatively via a retrospectively controlled study by a single surgeon with propensity score matching (PSM). We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-238/rc).
Methods
Study design and patient characteristics
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the Third Affiliated Hospital of Soochow University (Approval No. 2021 technology 97) and informed consent was taken from all the patients. We retrospectively analyzed 110 NSCLC cases with complete follow-up data (cT1-3N0-2M0) from December 2020 to May 2021. The patients were divided into divided into RATS and VATS groups (both three-port procedures) according to the patients’ preference. There were 67 patients in the RATS group, including 23 males and 44 females with a mean age of 60 years. Meanwhile, there were 43 patients in the VATS group, including 18 males and 25 females, with a mean age of 58 years.
The age, gender, body mass index (BMI), smoking history, operation method, longest tumor diameter, and tumor site of all patients were analyzed statistically. The propensity-score matching method was applied to control the potential differences between the patients’ characteristics, and the patients were matched according to a 1:1 ratio. After matching, there were 43 patients in the RATS group (29 males and 14 females, mean age: 58 years) and 43 patients in the VATS group (25 males and 18 females, mean age: 58 years).
Surgical procedures
RATS
Patient positioning and port placement
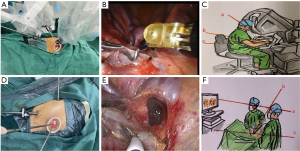
Equipment and personnel were positioned similar to a traditional VATS procedure. All surgical procedures were performed under general anesthesia. Single-lung ventilation was achieved by employing double-lumen endotracheal intubation. The patient was placed in a lateral position and bent by fixing the pelvis and hip. The robot was placed behind the patient’s head. Three ports (BP) were used. A 0.8 cm camera port incision was made between the seventh or eighth ribs at the midline of the arm. A 30-degree three-dimensional (3D) endoscope was then inserted to probe the thorax. Under direct vision, a practical 3 cm incision was made between the fifth or sixth front ribs, which served as the operating hole for the assistant, as well as a robotic arm working channel after placing the trocar sleeve. A 0.8 cm incision was then made between the seventh or eighth ribs at the rear axillary line for the trocar, which was the robot-operated robotic arm working channel. The port location for lung segment resection or same lateral surgery did not change except on the left side; the location of the camera port was more lateral than the right side to prevent the heart from blocking the surgical area (Figure 1).
Flat recognition of lung segment by expansion and collapse
After the precise cut-off of the target bronchus pulmonary artery, and pulmonary veins, the anesthesiologist was instructed to expand the lung and initiate unilateral lung ventilation after the lung lobe of the target segment was completely expanded. Normal lung tissue could almost completely collapse, but the target segment maintained an expanded state because the gas in the alveolar cavity could not be continually discharged. The collapsed normal lung tissue formed an obvious boundary with the expanding target segment, which was the intersegment plane.
Surgical procedure
The target pulmonary artery, target pulmonary vein and bronchus were accurately dissected and identified, according to the preoperative evaluation of the bronchial and vascular structure using 3D computed tomography bronchography and angiography (3D-CTBA) of the pulmonary nodules and pulmonary segment. If segmentectomy was performed, the expansion collapse method was used to determine and mark the intersection plane. The intersegmental plane was dissected using the energy equipment and the Endo-GIA staplers, and a sufficient safe margin was ensured. The specimen was removed after the resection and subjected to rapid freezing pathological examination at the same time, and the rapid pathology reports guided the lymphadenectomy procedure. Lymph nodes were sampled in cases of adenocarcinoma in situ carcinoma or microinvasive adenocarcinoma, and were systematically dissected in cases of invasive carcinoma. One chest tube and one silicon sphere were placed respectively after surgery.
VATS
Patient positioning and port placement
After general anesthesia and double cavity tracheal intubation, the patient was placed in a healthy lateral position and ventilated with single pulmonary. The thoracoscopic approach was performed using a three-ports method. A 1 cm observation hole was placed between the seventh or eighth ribs of the midline of the arm to probe the thorax. Under direct vision, a 3 cm practical incision was made between the front fourth or fifth costal areas for the main operating hole. Also, a 2 cm incision was subsequently made for the secondary hole between the seventh or eighth ribs at the posterior axillary line (Figure 1).
Flat recognition of lung segment by expansion and collapse
The expansion and collapse method for lung intersegmental plane was performed as outlined above in the RATS section.
Surgical procedure
This was performed using the same method, except without utilizing the robot platform.
Observational indicators
Safety, economic, and short-term efficacy observation indicators
Operation time, intraoperative blood loss, number of dissecting lymph nodes and dissecting stations, drainage volume on the first day postoperatively, total postoperative drainage, thoracic drainage indwelling time, postoperative complications, postoperative hospital stay, hospitalization costs, and unplanned re-hospitalization at 6 weeks postoperatively.
QoL observation indicators
(I) Pain score evaluation
This involved recording the pain score on the first day postoperatively using the visual analogue score (VAS). After visual measurement, postoperative patients drew a point consistent with the pain intensity in a straight line according to their own situation, which was repeated twice and the average of both times was recorded. The pain number scores at day 1 and 6 weeks postoperatively were recorded.
(II) Quality of survival evaluation
Using the tumor patient quality of survival core scale (EORTC-C30) at 1 day before surgery and 6 weeks postoperatively, we evaluated the baseline and short-term quality of survival changes of the two groups. The questionnaire of the department of thoracic surgery includes a global QoL scale and five functional scales (somatic function, role function, emotional function, cognitive function, and social function), with each scale scored from 0 to 100 points. The total score was the average score of each scale, with higher QoL scores indicating a better quality of survival. Unplanned re-hospitalization rates were also reported.
Follow-up
- Long-term postoperative follow-up: the patient follow-up began upon completion of the surgery, and a follow-up tracking process table of the study subjects was developed.
- Follow-up from 1 to 24 months postoperatively: the EORTC-QLQ-30 and pain scores were completed 6 weeks after surgery. Also, physical examination, chest slices, abdominal B ultrasound (liver, pancreas, spleen, adrenal), tumor markers (carcinoembryonic antigen (CEA), squamous cell carcinoma antigen (SCC), human CYFRA21-1 antigen (CYFRA21-1), neuron specific enolase (NSE), etc.), and chest CT were conducted every 6 months to determine the presence of tumor recurrence.
- At any time any sign of tumor recurrence, further cranial magnetic resonance imaging (MRI), systemic bone scan, or positron emission tomography-computed tomography (PET-CT) was performed to determine the presence or absence of tumor recurrence.
Statistical analysis
For quantitative data, the distribution morphology and homogeneity of variance were verified. If the data was normally distributed, the Student’s t-test was compared and represented by the mean ± standard deviation (mean ± SD); otherwise, median (interquartile spacing) [M (IQR)], the Mann-Whitney U test was applied. Classification data was compared using the chi-square test or Wilcoxon rank-sum test. The test standard was 0.05, using two-sided tests, and P<0.05 was considered statistically significant. Statistical analysis was carried out using SPSS 17.0 software (SPSS, Inc., Chicago, IL, USA).
Results
Clinical data before and after matching
A total of 110 patients underwent pulmonary surgery, including 67 patients in the RATS group and 43 patients in the VATS group. Statistical analysis of the baseline data (age, gender, BMI, smoking history, operation method, longest tumor diameter, and tumor site) of all patients was performed. Gender differed significantly between the two groups (P<0.001). After propensity-score matching, the two groups were comparable, there were 43 cases in each group, and there were no significant differences in all baseline data (P>0.05, Table 1).
Table 1
| Variables | Before matching | After matching | |||||
|---|---|---|---|---|---|---|---|
| VATS (n=43) | RATS n=67) | P value | VATS (n=43) | RATS (n=43) | P value | ||
| Gender | <0.001 | 0.31 | |||||
| Female | 25 | 44 | 25 | 29 | |||
| Male | 18 | 23 | 18 | 14 | |||
| Age (years, mean ± SD) | 58.26±10.28 | 60.61±10.91 | 0.26 | 58.26±10.28 | 57.98±10.70 | 0.90 | |
| BMI (kg/m2) | 23.16±3.91 | 23.35±2.82 | 0.79 | 23.16±3.91 | 22.82±2.76 | 0.64 | |
| Smoking history | 0.89 | 0.29 | |||||
| Yes | 6 | 10 | 6 | 3 | |||
| No | 37 | 57 | 37 | 40 | |||
| Operation method | |||||||
| Lobectomy | 17 | 32 | 17 | 22 | |||
| Segmentectomy | 26 | 35 | 26 | 26 | |||
| Tumor diameter (cm, mean ± SD) | 1.44±1.13 | 1.49±0.73 | 0.79 | 1.44±1.13 | 1.49±0.79 | 0.82 | |
| Tumor site | 0.07 | 0.33 | |||||
| RUL | 8 | 24 | 8 | 14 | |||
| RML | 3 | 8 | 3 | 6 | |||
| RLL | 6 | 14 | 6 | 12 | |||
| LUL | 20 | 13 | 20 | 13 | |||
| LLL | 6 | 8 | 6 | 8 | |||
VATS, thoracoscopic assisted surgery group; RATS, robotic assisted surgery group; BMI, body mass index; RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; LUL, left upper lobe; LLL, left lower lobe; SD, standard deviation.
Both matched groups achieved a R0 resection rate of 100%. The postoperative pathological analysis showed that there were 42 cases of adenocarcinoma and one case of squamous carcinoma in the RATS group; T stage: 17 cases of T1a, 18 cases of T1b, seven cases of T1c, and one case of T2b; N stage: 40 cases of N0 and three cases of N2; Pathological staging (pTNM stage): 17 cases of stage I A1, 17 cases of I A2, five cases of stage I A3, one case of stage II A, and three cases of stage III A. In the VATS group, there were 40 cases of adenocarcinoma and three cases of squamous carcinoma; T stage: 20 cases of T1a, 17 cases of T1b, four cases of T1c, one case of T2b, and one case of T3; N stage: 41 cases of N0, one case of N1, and one case of N2; pTNM stage: 20 cases of stage I A1, 17 cases of I A2, two cases of I A3, one case of II A, two cases of stage II B, and one case of III A. There were no significant differences in the pathological type or T, N, and pTNM stage between two matched groups (P>0.05, Table 2).
Table 2
| Variables | VATS (n=43) | RATS (n=43) | P value |
|---|---|---|---|
| Histological type | 0.31 | ||
| Adenocarcinoma | 40 | 42 | |
| Squamous cell carcinoma | 3 | 1 | |
| R0 resection | 43 | 43 | |
| T stage | 0.72 | ||
| T1a | 20 | 17 | |
| T1b | 17 | 18 | |
| T1c | 4 | 7 | |
| T2b | 1 | 1 | |
| T3 | 1 | 0 | |
| N stage | 0.37 | ||
| N0 | 41 | 40 | |
| N1 | 1 | 0 | |
| N2 | 1 | 3 | |
| pTNM stage | 0.48 | ||
| IA1 | 20 | 17 | |
| IA2 | 17 | 17 | |
| IA3 | 2 | 5 | |
| IIA | 1 | 1 | |
| IIB | 2 | 0 | |
| IIIA | 1 | 3 |
VATS, thoracoscopic assisted surgery group; RATS, robotic assisted surgery group.
Operative features
The average operation time in the RATS group was 21 minutes shorter compared to VATS (91.59±21.59 vs. 113.14±37.16 min, P=0.001), and the average hospitalization costs were 17,746 China Yuan (CNY) higher than VATS (73,380.35±8,126.85 vs. 55,634.74±6,544.36 CNY, respectively, P<0.001). Moreover, the RATS group had less intraoperative blood loss than VATS, with an average reduction of 8 mL (83.74±39.26 vs. 92.49±19.97 mL, respectively, P=0.19), but had a higher drainage volume on the first day postoperatively than the VATS group (186.63±176.11 vs. 162.02±63.44 mL, respectively, P=0.39). Meanwhile, the total postoperative drainage of the RATS group was less than that of the VATS group, with an average reduction of 97.44 mL (362.91±338.96 vs. 460.35±150.71 mL, respectively, P=0.09), and the thoracic drainage indwelling time of the RATS group was shorter than that of the VATS group (2.14±1.19 vs. 2.58±0.88 days, respectively, P=0.05); however, these differences were not statistically significant. In addition, there were no significant differences in the number of dissecting lymph nodes and dissecting stations, postoperative complications, or postoperative hospital stay between the two groups (Table 3).
Table 3
| Variables | VATS (n=43) | RATS (n=43) | P value |
|---|---|---|---|
| Operation time (min, mean ± SD) | 113.14±37.16 | 91.59±21.59 | 0.001 |
| Number of the dissecting lymph nodes in N1 (mean ± SD) | 2.47±1.94 | 2.02±1.60 | 0.25 |
| Number of the dissecting lymph nodes in N2 (mean ± SD) | 1.49±0.99 | 1.40±0.93 | 0.65 |
| Intraoperative blood loss (mL, mean ± SD) | 92.49±19.97 | 83.74±39.26 | 0.19 |
| Postoperative hospital stay (days, mean ± SD) | 3.79±1.04 | 3.42±2.26 | 0.33 |
| Thoracic drainage indwelling time (days, mean ± SD) | 2.58±0.88 | 2.14±1.19 | 0.05 |
| Drainage volume on the first day postoperatively (mL, mean ± SD) | 162.02±63.44 | 186.63±176.11 | 0.39 |
| Total postoperative drainage (mL, mean ± SD) | 460.35±150.71 | 362.91±338.96 | 0.09 |
| Early postoperative complications | 0.26 | ||
| Yes | 0 | 5 | |
| No | 43 | 38 | |
| Hospitalization cost (CNY, mean ± SD) | 55634.74±6544.36 | 73380.35±8126.85 | <0.001 |
| Unplanned re-hospitalization | 0.36 | ||
| Yes | 2 | 0 | |
| No | 41 | 43 |
VATS, thoracoscopic assisted surgery group; RATS, robotic assisted surgery group; CNY, China Yuan; SD, standard deviation.
QoF and postoperative pain score
The RATS group performed better than VATS in postoperative pain; the visual analogue pain scores of the RATS group were lower than those of the VATS group at 1 day and 6 weeks postoperatively (2.53±0.86 vs. 3.88±0.88, P<0.001 and 0.35±0.65 vs. 0.74±0.88, P=0.02, Table 4).
Table 4
| Variables | VATS (n=43) | RATS (n=43) | P value |
|---|---|---|---|
| Global QoL | |||
| Baseline | 100 | 100 | |
| 6 weeks postoperatively (mean ± SD) | 93.02±15.21 | 98.64±5.73 | 0.03 |
| Physical function | |||
| Baseline | 100 | 100 | |
| 6 weeks postoperatively (mean ± SD) | 90.39±8.27 | 93.02±8.35 | 0.15 |
| Fatigue symptoms | |||
| Baseline | 0 | 0 | |
| 6 weeks postoperatively (mean ± SD) | 12.40±9.45 | 10.08±8.68 | 0.24 |
| Pain symptoms | |||
| Baseline | 0 | 0 | |
| 6 Weeks postoperatively (mean ± SD) | 10.85±10.21 | 6.20±8.15 | 0.02 |
| Dyspnea symptoms | |||
| Baseline | 0 | 0 | |
| 6 Weeks postoperatively (mean ± SD) | 22.49±23.82 | 20.15±18.02 | 0.61 |
| Pain score of VAS | |||
| 1 Day postoperatively (mean ± SD) | 3.88±0.88 | 2.53±0.86 | <0.001 |
| 6 Weeks postoperatively (mean ± SD) | 0.74±0.88 | 0.35±0.65 | 0.02 |
VATS, thoracoscopic assisted surgery group; RATS, robotic assisted surgery group; QoL, quality of life; VAS, visual analogue score; SD, standard deviation.
Furthermore, both groups had a response compliance of 100% for the QoL questionnaire (EORTC-C30). At the preoperative baseline level, there was no difference in scale scores between the two groups. At 6 weeks postoperatively, the QoL scores were higher in the RATS group than in the VATS (98.64±5.73 vs. 93.02±15.21, P=0.03). The difference was most evident in the pain symptoms scale; the RATS group had lower pain scores compared to the VATS group (6.20±8.15 vs. 10.85±10.21, P=0.02). While the scores for the physical function, fatigue symptoms and dyspnea symptoms were approximate in the two groups (Table 4).
Unplanned re-hospitalization rate
The unplanned re-hospitalization rate at 6 weeks postoperatively was 0 in the RATS group, compared to 4.7% (2/43) in the VATS group (P=0.36, Table 3). Both patients in the VATS group were readmitted because of a medium amount of pleural effusion what was not chylothorax and pyothorax, and cured by thoracic close drainage and conservative treatment.
Discussion
In this study, the perioperative effect of the two groups was analyzed, and there were no statistical differences in the intraoperative blood loss, number of dissecting lymph nodes and dissecting stations, hospitalization time, thoracic drainage indwelling time, drainage volume on day 1 postoperatively, total postoperative drainage, or postoperative complications between the group. We found that both RATS and VATS were safe and effective procedures, with a similar curative effect. However, we observed that the operation time of RATS was shorter, with a statistically decrease of 21 minutes compared to VATS. Also, the thoracic drainage indwelling time in RATS was reduced by 0.5 days, and the total postoperative drainage was decreased by 97 mL; however, these two advantages were not statistically significant. With increased surgical cases and improvements of the surgical technology, these trends may become statistically significant. Following the advent of VATS, patients gradually underwent minimally invasive surgery, with VATS becoming the key surgical approach at present (8). RATS is a novel revolutionary surgical platform, and there is still a debate about whether the robotic surgical system offers significant advantages. According to the findings of this study, the perioperative safety and treatment effects of RATS was not inferior to those of VATS.
In this study, patients received the EORTC-C30 questionnaire to determine their QoL scores. We found that both groups exhibited a degree of fatigue and dyspnea. Meanwhile, the physical function category scores decreased, and the scores of fatigue and dyspnea symptom increased in both groups although the differences were not statistically significant. Notably, the QoL scores were markedly better in the RATS group than in the VATS group at 6 weeks postoperatively. For lung cancer patients, in addition to survival, having the ability to enjoy a useful and fulfilling life is also a crucial goal of treatment (9). From the short-term follow-up data examined in this study, it is clear that the superior QoF in the RATS group was due to the reduction in postoperative pain, which was confirmed by the EORTC-C30 pain symptom scale as well as the postoperative VAS pain score.
There was no statistical difference in the unplanned re-hospitalization rate between two groups, but the RATS group exhibited a lower trend. This was likely due to the rotation of the machine arm wrist for a better operating angle, which could avoid energy collateral damage against the surrounding lung tissue or bronchus (10). To control the hospitalization costs and hospital stay, patients had the potential to be discharged when unstable or underprepared, and may have been accidentally re-hospitalized due to delayed postoperative complications. Pulmonary complications after lobectomy/segmentectomy are common, and are related to higher mortality rates and longer hospitalization times (11). Some scholars have proposed that segmentectomy causes higher rates of persistent pulmonary air leakage (4). In this study, RATS showed a promising potential to reduce the rate of 30-day unplanned re-hospitalization rate, and this favorable effect could last up to 6 months. Despite the considerable expenses of robotic surgery, the total hospitalization time and costs over the 6-month postoperative period might be similar to that of VATS (given its higher rates of unplanned hospital readmission).
In thoracoscopic surgery, the three axes (operator’s line of sight, thoracoscopic observation axis, and operating axis) cannot coincide. If the operating axis deviates from the midline, which would make the operation difficult and lead to fatigue. Robotic surgery has an advantage that could coincide the three axes to the midline, which was more ergonomic. When the minimally invasive surgery was done by RATS, the operating feeling of the surgeon was more likely as thoracotomy surgery. In addition, the Da Vinci robot surgical system has a 3D stereoscopic imaging system, a unique internal wrist rotation system (10), as well as an automatic filtering function, and performing surgery in a seated position could reduce the fatigue associated with longer surgeries.
However, current robotic surgical systems still have some drawbacks. Firstly, the lack of force feedback, which can be dangerous if the surgeon’s hand makes unintentional movements (12). Secondly, the layout of the operation ports is relatively fixed and limited, and is not as flexible or versatile as that of VATS. Furthermore, unplanned intraoperative conversion to thoracotomy is an essential issue for RATS (13). During RATS, the operator is not present near the operating table, which results in potential hazards in cases of accidental bleeding. Finally, the hospitalization costs associated with RATS were considerably higher than those of VATS, which is likely due to the fact that VATS equipment is relatively inexpensive and the instruments can be used repeatedly.
In conclusion, despite its high costs, robotic surgery for lobectomy and segmentectomy exhibits similar perioperative safety and short-term efficacy to thoracoscopic surgery. Meanwhile, robotic surgery offers great potential for reducing the operation time and the rate of unplanned re-hospitalizations, as well as improving the QoF of patients. If the patients’ economic condition was allowed, Robot was preferred.
Acknowledgments
Funding: This work was supported in part by the Major Science and Technology Project of Changzhou Health Commission (No. ZD202104), and the Youth Talent Science and Technology Project of Changzhou Health Commission (No. QN202017).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-238/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-238/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-238/coif). LZ and QW report funding from the Major Science and Technology Project of Changzhou Health Commission (No. ZD202104), and the Youth Talent Science and Technology Project of Changzhou Health Commission (No. QN202017). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the Third Affiliated Hospital of Soochow University (Approval No. 2021 technology 97) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhang N, Nan A, Chen L, et al. Circular RNA circSATB2 promotes progression of non-small cell lung cancer cells. Mol Cancer 2020;19:101. [Crossref] [PubMed]
- Hoy H, Lynch T, Beck M. Surgical Treatment of Lung Cancer. Crit Care Nurs Clin North Am 2019;31:303-13. [Crossref] [PubMed]
- Adizie JB, Khakwani A, Beckett P, et al. Stage III Non-small Cell Lung Cancer Management in England. Clin Oncol (R Coll Radiol) 2019;31:688-96. [Crossref] [PubMed]
- Suzuki K, Saji H, Aokage K, et al. Comparison of pulmonary segmentectomy and lobectomy: Safety results of a randomized trial. J Thorac Cardiovasc Surg 2019;158:895-907. [Crossref] [PubMed]
- Veronesi G, Novellis P, Voulaz E, et al. Robot-assisted surgery for lung cancer: State of the art and perspectives. Lung Cancer 2016;101:28-34. [Crossref] [PubMed]
- Hu X, Wang M. Efficacy and Safety of Robot-assisted Thoracic Surgery (RATS) Compare with Video-assisted Thoracoscopic Surgery (VATS) for Lung Lobectomy in Patients with Non-small Cell Lung Cancer. Comb Chem High Throughput Screen 2019;22:169-78. [Crossref] [PubMed]
- Guo F, Ma D, Li S. Compare the prognosis of Da Vinci robot-assisted thoracic surgery (RATS) with video-assisted thoracic surgery (VATS) for non-small cell lung cancer: A Meta-analysis. Medicine (Baltimore) 2019;98:e17089. [Crossref] [PubMed]
- Vannucci F, Gonzalez-Rivas D. Is VATS lobectomy standard of care for operable non-small cell lung cancer? Lung Cancer 2016;100:114-9. [Crossref] [PubMed]
- Morrison EJ, Novotny PJ, Sloan JA, et al. Emotional Problems, Quality of Life, and Symptom Burden in Patients With Lung Cancer. Clin Lung Cancer 2017;18:497-503. [Crossref] [PubMed]
- Huang J, Li J, Li H, et al. Continuous 389 cases of Da Vinci robot-assisted thoracoscopic lobectomy in treatment of non-small cell lung cancer: experience in Shanghai Chest Hospital. J Thorac Dis 2018;10:3776-82. [Crossref] [PubMed]
- Cao C, Louie BE, Melfi F, et al. Impact of pulmonary function on pulmonary complications after robotic-assisted thoracoscopic lobectomy. Eur J Cardiothorac Surg 2020;57:338-42. [Crossref] [PubMed]
- Zuo S, Wang Z, Zhang T, et al. A novel master-slave intraocular surgical robot with force feedback. Int J Med Robot 2021;17:e2267. [Crossref] [PubMed]
- Huang J, Li C, Li H, et al. Robot-assisted thoracoscopic surgery versus thoracotomy for c-N2 stage NSCLC: short-term outcomes of a randomized trial. Transl Lung Cancer Res 2019;8:951-8. [Crossref] [PubMed]


