
A systematic review and meta-analysis of the effect of transitional care interventions on the prognosis of patients with heart failure
Introduction
Most cardiovascular-related diseases eventually turn into heart failure (1). The incidence rate and mortality of heart failure are increasing due to the acceleration of the ageing process (2). The treatment of this disease requires enormous medical resources, resulting in a corresponding economic burden. Patients with heart failure need complex treatment schemes and long-term follow-up strategies (2). A previous study had demonstrated that 20% of patients with heart failure are re-hospitalized within 1 month after discharge, while the proportion is as high as 34% within 3 months after discharge (3). Heart failure, unlike other diseases, has a higher rate of readmissions. However, lack of self-management awareness, weak family support, and lack of knowledge of the early symptoms of disease monitoring all negatively impact the prognosis of patients with heart failure, especially repeated hospitalization (4).
Transitional care usually refers to the continuation from hospital to family, including the discharge plan, referral, and constant follow-up and guidance after patients return to family or community, which can fill the missing section of nursing intervention from hospital to family. The main goal of transitional care is to promote the rehabilitation of patients and reduce the need for rehospitalization due to the deterioration of their condition (5). Transitional nursing intervention on patients with heart failure has been controversial, especially in all-cause readmission rates, emergency visit rates, emergency admission rates and mortality. However, the results of different studies deviate from each other. A previous study had shown that transitional care only reduces the heart failure-specific readmission rate (4). At present, there is a lack of solid evidence to confirm the positive impact of transitional care on patients with heart failure. Therefore, this study conducted a meta-analysis to explore the impact of transitional nursing on the prognosis of patients with heart failure and provide a reference basis for clinical decision-making. We present the following article in accordance with the PRISMA reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-102/rc).
Methods
Literature retrieval
Literature searches were conducted in PubMed, MEDLINE, Embase, and CENTRAL databases. The search terms were: (“transitional care” or “extended care” or “hospital-to-home intervention” or “continuity of care”) and (“heart failure” or “cardiac failure”). The date of literature search was October 12, 2021.
Literature screening
The inclusion criteria refer to PICOS principles: (I) The subjects were patients with heart failure; (II) In the study, the experimental group implemented continuous care (TC), and the control group implemented routine care (UC). Transitional nursing intervention refers to the implementation of continuous nursing intervention for patients from hospital to family, led by nurses, including discharge plan formulated by the hospital, continuous follow-up and guidance after patients return to family or community; Routine nursing refers to receiving nursing intervention during hospitalization and no nursing intervention after discharge; (III) the observation indicators included readmission rate, emergency visit rate, and mortality of patients with heart failure; (IV) The study type was an RCT; (V) the statistical data in the literature could calculate the odds ratio (OR) and 95% confidence interval (CI); (VI) The time interval of literature publication is after January 2000. The exclusion criteria were as follows: (I) The literature had research design defects or statistical method errors that could not be corrected. The error evaluation of Statistical Methods refers to common statistical errors (6); (II) the main content of the literature was not in line with the research direction of this paper; (III) the specific scheme of transitional nursing intervention was not described; (IV) the subjects had no clear diagnostic criteria; (V) in addition to nursing intervention, the subjects also received other intervention measures affecting the research results; (VI) the baseline data of the control group and the experimental group were poorly balanced; (VII) the data was incomplete and could not be supplemented by contacting the author.
Literature data sorting
A researcher independently extracted the data of the included literature, including the author, title, publication time, patient baseline data, intervention measures, and observation indicators. Two other researchers checked the extracted data and information. When there were different opinions on literature data extraction, the 3 researchers discussed and resolved any differences.
Literature quality evaluation
In this paper, three researchers used Cochrane bias risk assessment to evaluate the quality of the literature included in the study. The literature quality can be divided into three categories: low overall bias risk, high overall bias risk and unknown bias risk. The researchers independently evaluated the literature quality. In case of inconsistency in the judgment results of literature quality, the results agreed by researchers after discussion shall be adopted.
Heterogeneity test and publication bias test
The Chi-square test was used to assess heterogeneity. When I2 corrected by degrees of freedom was more than 50% and P<0.1, this indicated heterogeneity among the literature. Subgroup analysis was used to explore the causes of heterogeneity. When I2≤50% and P≥0.1 after degrees of freedom correction, there was no heterogeneity among the literature. Egger test was used to examine the publication bias.
Heterogeneity source analysis
Suppose there was heterogeneity among the literature after excluding the low-quality literatures. In that case, the heterogeneity test was carried out again, and the combined analysis model was selected according to the test results. If the results did not change significantly, indicating that the sensitivity was low and the results were credible. If there was a clear and significant change in the source of the intervention, suggesting that there was a significant change in the potential effect of the intervention. If there was a significant change in the source of the intervention, it indicates a significant change in the potential impact of the intervention.
Effect model selection and forest map drawing
According to the results of the heterogeneity test and heterogeneity source analysis, the merger effect model was selected. There was no heterogeneity among the studies finally included in the analysis, and the fixed effect model was used. Finally, there was heterogeneity among the studies included in the analysis, and the reason for the heterogeneity is not found. Therefore, the random effect model was used. The summary effect results were displayed in the form of forest map.
Statistical analysis
Data were statistically analyzed by Cochrane software RevMan 5.3. OR value and 95% CI were used to describe the count data. P<0.05 indicated that the difference was statistically significant.
Results
Retrieval results and literature quality evaluation
Based on the relevant subject words, 1,017 studies related to the prognosis of heart failure after transitional care intervention were retrieved. According to the literature screening criteria, this study further screened 18 studies for meta-analysis (7-24). The flow chart of literature screening is shown in Figure 1. A total of 4,123 patients with heart failure were included in the 18 studies, comprising 1,914 (46.42%) patients receiving the transitional nursing intervention and 2,209 (53.58%) patients receiving the routine nursing intervention. The patients’ clinical information is shown in Table 1. Among the 18 articles, 13 articles showed an overall low risk of bias and 5 articles showed an overall high risk of bias.
Table 1
| Study | Study design | No. of patients | Readmission | Emergency visit | Mortality cases | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TC | UC | TC | UC | TC | UC | TC | UC | |||||
| Anderson et al. (10), 2005 | RCT | 44 | 77 | 5 | 34 | – | – | – | – | |||
| Angermann et al. (18), 2012 | RCT | 352 | 363 | 119 | 112 | – | – | – | – | |||
| Atienza et al. (19), 2004 | RCT | 164 | 174 | – | – | – | – | 39 | 51 | |||
| Bowles et al. (8), 2011 | RCT | 101 | 116 | 23 | 26 | – | – | – | – | |||
| Blue et al. (22), 2001 | RCT | 84 | 81 | – | – | – | – | 25 | 25 | |||
| Domingues et al. (11), 2011 | RCT | 48 | 63 | 20 | 23 | 4 | 8 | – | – | |||
| Ducharme et al. (16), 2005 | RCT | 115 | 115 | – | – | 69 | 72 | – | – | |||
| Harrison et al. (21), 2002 | RCT | 80 | 77 | – | – | 23 | 35 | – | – | |||
| Kulshreshtha et al. (24), 2010 | RCT | 114 | 139 | – | – | 22 | 34 | – | – | |||
| Kwok et al. (7), 2008 | RCT | 49 | 56 | 23 | 32 | – | – | – | – | |||
| Lee et al. (20), 2019 | RCT | 159 | 329 | 18 | 103 | 3 | 36 | – | – | |||
| Naylor et al. (23), 2004 | RCT | 118 | 121 | 45 | 61 | – | – | 11 | 13 | |||
| Nucifora et al. (17), 2006 | RCT | 99 | 101 | – | – | – | – | 14 | 8 | |||
| Stauffer et al. (13), 2011 | RCT | 56 | 84 | 5 | 12 | 1 | 6 | – | – | |||
| Thompson et al. (14), 2005 | RCT | 58 | 48 | 13 | 21 | – | – | – | – | |||
| Tsuyuki et al. (9), 2004 | RCT | 140 | 136 | – | – | 41 | 69 | – | – | |||
| Wong et al. (15), 2016 | RCT | 43 | 41 | 14 | 25 | – | – | 3 | 6 | |||
| Yu et al. (12), 2015 | RCT | 90 | 88 | 19 | 39 | 6 | 14 | 2 | 6 | |||
TC, transitional care; UC, usual care.
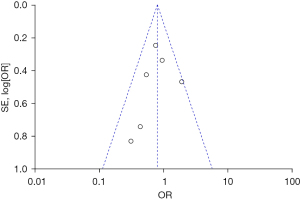
Effect of transitional care interventions on the readmission rate
Among the 18 studies, 11 investigated the effect of transitional care interventions on the readmission rate of patients with heart failure, including 1,118 patients receiving transitional nursing and 1,386 patients receiving routine nursing. There was heterogeneity among the 11 studies (χ2=41.75, P<0.00001, I2=76%). The analysis of heterogeneity sources indicated that the results were robust and the source of heterogeneity was unknown, thus the random effect model was used. The combined effect amount OR =0.63 (95% CI: 0.53, 0.76), and the test of overall effect Z=5.07 (P<0.00001), as shown in Figure 2. The analysis showed that the readmission rate of patients with heart failure receiving transitional care was lower than that in patients receiving routine care. The funnel plot showed that the data points were distributed on both sides, within the confidence interval, and were roughly symmetrical, indicating no obvious publication bias, as shown in Figure 3.


Effect of transitional care interventions on the emergency visit rate
Eight of the 18 studies investigated the effect of transitional care interventions on the emergency visit rate of patients with heart failure, including 802 patients who received transitional nursing and 1,031 patients who received routine nursing. There was no heterogeneity among studies (χ2=11.35, P=0.12, I2=38%), and the fixed effect model was used. The combined effect amount OR =0.51 (95% CI: 0.40, 0.66), and the test of overall effect Z=5.22 (P<0.00001), as shown in Figure 4. The analysis showed that the emergency visit rate of heart failure patients receiving transitional care was lower than that of patients receiving routine care. The funnel plot showed that the data points were distributed on both sides, within the confidence interval, and were roughly symmetrical, indicating no obvious publication bias, as shown in Figure 5.


Effect of transitional care interventions on mortality
Six of the 18 studies investigated the effect of transitional care interventions on the mortality of patients with heart failure, including 661 patients who received transitional nursing and 606 patients who received routine nursing. There was no heterogeneity among the 6 studies (χ2=6.61, P=0.25, I2=24%), and the fixed effect model was used. The combined effect amount OR =0.80 (95% CI: 0.58, 1.09), and the test of overall effect Z=1.43 (P=0.15), as shown in Figure 6. The analysis showed that there was no significant difference in mortality between patients with heart failure receiving transitional care and patients receiving routine care. The funnel plot showed that the points were distributed on both sides, within the confidence interval, and were roughly symmetrical, indicating no obvious publication bias, as shown in Figure 7.

Discussion
There is no unified standard for the clinical care intervention of patients with heart failure. A previous study believed that transitional care intervention and self-management of heart failure can significantly improve the prognosis of patients (7). Therefore, to provide a reference basis for the care intervention of patients with heart failure, this study comprehensively included relevant literature for meta-analysis. The convenience of transitional care intervention and the corresponding clinical efficacy have been improved in recent years. Therefore, we searched the literature on the impact of transitional care interventions on the prognosis of patients with heart failure after 2000. The time limit of this study is significantly different from other similar studies. The primary etiology of heart failure is complex and diverse. Our research does not focus on heart failure caused by a specific disease but includes relevant studies on multidisciplinary heart failure for comprehensive analysis.
We found that transitional care intervention can reduce the readmission rate and emergency visit rate, but it has no significant effect on the mortality of patients. A study had pointed out that patients with chronic heart failure lack a reasonable self-management scheme and a well-established family expenditure system after discharge (3). Thus, their condition cannot be effectively controlled. Over a short period, their condition will worsen again, further leading to an increase in the number of readmissions. Proper and timely transitional care intervention can solve this problem. Transitional care intervention can help patients control exacerbation factors and improve their ability to identify the early symptoms of heart failure deterioration. Therefore, when the early signs of heart failure occur, they can receive treatments in time.
However, the differences in the specific measures of transitional care intervention in this study should be noted, including disease-related education for patients and their families, formulation of a personalized nursing plan at discharge, and follow-up after discharge. Feltner et al. also conducted relevant research in which they specifically compared the effects of different transitional intervention strategies on the readmission rate of patients with multidisciplinary heart failure (25). The home visit program reduced all-cause readmissions and heart failure-specific readmissions. Structured telephone support intervention can reduce heart failure-specific readmission but cannot reduce all-cause readmission (25). A study also pointed out that the readmission rate of patients with heart failure is related to the follow-up time and frequency of transitional care intervention. The higher the follow-up frequency and the longer the follow-up duration, the lower the readmission rate (20). A study had confirmed that transitional care can reduce the all-cause readmission rate of patients and reduce the readmission rate of patients with heart failure (11).
A study had investigated mortality stratified by type of transitional care intervention and time of outcome. Compared with routine care, home visit intervention reduced mortality (14). Remote monitoring and major educational interventions did not reduce mortality. However, in our study, we did not find that transitional intervention significantly impacted the mortality of patients with heart failure. The results may be related to the insufficient inclusion of time factors in the literature we analyzed. A study had pointed out that the 3-year survival rate of heart failure patients with transitional care intervention is higher than that of patients with routine care (22).
It is worth noting that in some current studies, the leaders of transitional care intervention are not nurses but pharmacists. A study had shown that transitional care intervention led by pharmacists can reduce the 30-day all-cause readmission rate of patients with congestive heart failure. However, the cost-benefit comparison results are not clear (26).
In conclusion, our study shows that transitional care intervention can reduce the readmission rate and emergency visit rate, but has no significant effect on the mortality of patients. This study suggests establishing a transitional care intervention system for patients with heart failure.
Acknowledgments
Funding: The project was supported by Hainan Province Clinical Medical Center.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-102/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-102/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Metra M, Teerlink JR. Heart failure. Lancet 2017;390:1981-95. [Crossref] [PubMed]
- Chaudhry MA. Heart Failure. Curr Hypertens Rev 2019;15:7. [Crossref] [PubMed]
- Mosterd A, Cost B, Hoes AW, et al. The prognosis of heart failure in the general population: The Rotterdam Study. Eur Heart J 2001;22:1318-27. [Crossref] [PubMed]
- Mai Ba H, Son YJ, Lee K, et al. Transitional Care Interventions for Patients with Heart Failure: An Integrative Review. Int J Environ Res Public Health 2020;17:2925. [Crossref] [PubMed]
- Coleman EA, Boult CAmerican Geriatrics Society Health Care Systems Committee. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc 2003;51:556-7. [Crossref] [PubMed]
- Sebastião YV, St Peter SD. An overview of commonly used statistical methods in clinical research. Semin Pediatr Surg 2018;27:367-74. [Crossref] [PubMed]
- Kwok T, Lee J, Woo J, et al. A randomized controlled trial of a community nurse-supported hospital discharge programme in older patients with chronic heart failure. J Clin Nurs 2008;17:109-17. [Crossref] [PubMed]
- Bowles KH, Hanlon AL, Glick HA, et al. Clinical effectiveness, access to, and satisfaction with care using a telehomecare substitution intervention: a randomized controlled trial. Int J Telemed Appl 2011;2011:540138. [Crossref] [PubMed]
- Tsuyuki RT, Fradette M, Johnson JA, et al. A multicenter disease management program for hospitalized patients with heart failure. J Card Fail 2004;10:473-80. [Crossref] [PubMed]
- Anderson C, Deepak BV, Amoateng-Adjepong Y, et al. Benefits of comprehensive inpatient education and discharge planning combined with outpatient support in elderly patients with congestive heart failure. Congest Heart Fail 2005;11:315-21. [Crossref] [PubMed]
- Domingues FB, Clausell N, Aliti GB, et al. Education and telephone monitoring by nurses of patients with heart failure: randomized clinical trial. Arq Bras Cardiol 2011;96:233-9. [Crossref] [PubMed]
- Yu DS, Lee DT, Stewart S, et al. Effect of Nurse-Implemented Transitional Care for Chinese Individuals with Chronic Heart Failure in Hong Kong: A Randomized Controlled Trial. J Am Geriatr Soc 2015;63:1583-93. [Crossref] [PubMed]
- Stauffer BD, Fullerton C, Fleming N, et al. Effectiveness and cost of a transitional care program for heart failure: a prospective study with concurrent controls. Arch Intern Med 2011;171:1238-43. [Crossref] [PubMed]
- Thompson DR, Roebuck A, Stewart S. Effects of a nurse-led, clinic and home-based intervention on recurrent hospital use in chronic heart failure. Eur J Heart Fail 2005;7:377-84. [Crossref] [PubMed]
- Wong FK, Ng AY, Lee PH, et al. Effects of a transitional palliative care model on patients with end-stage heart failure: a randomised controlled trial. Heart 2016;102:1100-8. [Crossref] [PubMed]
- Ducharme A, Doyon O, White M, et al. Impact of care at a multidisciplinary congestive heart failure clinic: a randomized trial. CMAJ 2005;173:40-5. [Crossref] [PubMed]
- Nucifora G, Albanese MC, De Biaggio P, et al. Lack of improvement of clinical outcomes by a low-cost, hospital-based heart failure management programme. J Cardiovasc Med (Hagerstown) 2006;7:614-22. [Crossref] [PubMed]
- Angermann CE, Störk S, Gelbrich G, et al. Mode of action and effects of standardized collaborative disease management on mortality and morbidity in patients with systolic heart failure: the Interdisciplinary Network for Heart Failure (INH) study. Circ Heart Fail 2012;5:25-35. [Crossref] [PubMed]
- Atienza F, Anguita M, Martinez-Alzamora N, et al. Multicenter randomized trial of a comprehensive hospital discharge and outpatient heart failure management program. Eur J Heart Fail 2004;6:643-52. [Crossref] [PubMed]
- Lee J, Reyes F, Islam M, et al. Outcomes of a Transitional Care Clinic to Reduce Heart Failure Readmissions at an Urban Academic Medical Center. Int J Clin Res Trials 2019;4:140. [Crossref] [PubMed]
- Harrison MB, Browne GB, Roberts J, et al. Quality of life of individuals with heart failure: a randomized trial of the effectiveness of two models of hospital-to-home transition. Med Care 2002;40:271-82. [Crossref] [PubMed]
- Blue L, Lang E, McMurray JJ, et al. Randomised controlled trial of specialist nurse intervention in heart failure. BMJ 2001;323:715-8. [Crossref] [PubMed]
- Naylor MD, Brooten DA, Campbell RL, et al. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc 2004;52:675-84. [Crossref] [PubMed]
- Kulshreshtha A, Kvedar JC, Goyal A, et al. Use of remote monitoring to improve outcomes in patients with heart failure: a pilot trial. Int J Telemed Appl 2010;2010:870959. [Crossref] [PubMed]
- Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med 2014;160:774-84. [Crossref] [PubMed]
- McKay C, Park C, Chang J, et al. Systematic Review and Meta-analysis of Pharmacist-Led Transitions of Care Services on the 30-Day All-Cause Readmission Rate of Patients with Congestive Heart Failure. Clin Drug Investig 2019;39:703-12. [Crossref] [PubMed]



