Evaluating the efficacy and safety of percutaneous coronary intervention (PCI) versus the optimal drug therapy (ODT) for stable coronary heart disease: a systematic review and meta-analysis
Introduction
In patients with stable coronary artery disease, complicated chronic total occlusion (CTO) or significant coronary artery stenosis is a powerful factor leading to patient death (1-3). Approximately 20% of patients with stable coronary artery disease have CTO or significant coronary artery stenosis (4). Although the technology required for coronary CTO intervention has improved, only 5% of CTO patients are treated with percutaneous coronary intervention (PCI), the rest of the patients were treated with drugs (5). PCI is a treatment method for improving myocardial blood perfusion by dredging stenotic or even occluded coronary lumen through cardiac catheterization. Previous observational studies have shown that recanalization of CTO using PCI improves patient survival, reduces the need for coronary artery bypass grafting (CABG), and reduces the incidence of future myocardial infarction (MI) (6,7).
Therefore, although the guidelines recommend that CTO patients consider PCI to improve their survival and quality of life (8-10), the PCI rate of CTO patients is still very low. For CTO patients, the question of whether PCI or drug therapy should be the preferred treatment option remains controversial. Some research reports doubt the potential benefits of PCI (11-15). Therefore, the purpose of this meta-analysis is to compare the results of PCI and optimal drug therapy (ODT) on CTO lesions or significant coronary artery stenosis and provide a more comprehensive understanding of the effectiveness of each treatment. We present the following article in accordance with the PRISMA reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-222/rc).
Methods
Search strategy
The following databases were searched: PubMed, Cochrane Central Register of Controlled Trials, Embase, and Web of Science. Literature in all languages was included in the search. Meta-analyses, and systematic reviews were also hand-searched to find relevant literature that might have been missed by the initial search. The following search terms were used: “coronary heart disease”, “stable coronary heart disease”, “stable angina pectoris”, “percutaneous coronary intervention”, “PCI”, “percutaneous transluminal coronary angioplasty”, “drug therapy”, “optimized drug treatment” and “optimized drug therapy”. The retrieval time was from January 2010 to November 2021.
Inclusion and exclusion criteria
To be included in this meta-analysis, a study fulfilled the following inclusion criteria: (I) research involving patients with stable coronary heart disease who require medication or PCI; (II) research that measured and compared the difference between medication and PCI treatment results; and (III) the outcomes evaluated included all causes of mortality, cardiogenic death, stroke, cerebrovascular accident (CVA), MI, revascularization, and patient life quality. A study was excluded if it fulfilled the following exclusion criteria: (I) research subjects included underage patients; (II) the research included animal experiments; and/or (III) the study did not involve comparison of the efficacy of drug treatment and PCI.
Paper screening and data extraction
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement methodology was adhered to. According to Participants, Intervention, Control, Outcomes, Study (PICOS) criteria, two reviewers independently evaluated the title and abstract of each article to determine whether it was eligible to be selected for the study. If any reviewer believed that the article met the criteria, the full text was reviewed. If there was a disagreement about the qualifications of the article, the two reviewers discussed whether the qualifications of the article could be agreed. If the two reviewers failed to reach agreement, a third reviewer made the decision. If additional information was needed about the article, the reviewers contacted the author of the corresponding article.
The patients included in the articles were divided into two groups: the PCI group, and the ODT group. The data was also independently extracted by two reviewers in accordance with the pre-established data tables. Data for the author name, the country where the author’s paper is signed, publication time, journal name, and patient demographics were extracted. Data were also extracted for the probability of MI, mortality rate, number of stroke events, rate of revascularization, and patient quality of life. The two reviewers exchanged views on the data tables and discussed the differences in the data they extracted, and negotiate unified data.
Quality assessment
ReMan 5.3 was used to analysis the data including 1-year success rate, 2-year success rate, total sample size, and various subgroups. The weighted average success rate was calculated using Stata 15.0 software. The criteria for treatment success were based on clinical examination and imaging examination. Clinical examination criteria included the absence during follow-up of spontaneous pain, night pain, hot or cold pain, occlusion pain, percussion pain, gingival or sinus canal swelling, fistula, discomfort, and loosening. The imaging examination criteria included no new lesions, no transmission image of apex or reduction of original apical transmission image, and no closure of apical openings.
Statistical analysis
According to the Cochrane ROB 2.0 principle, and heterogeneity between studies was assessed using I2 statistics, with 25%, 50%, and 75% representing low, medium, and high heterogeneity, respectively. If I2<50% and P>0.1 between studies, a fixed effect model was used. If I2>50% and P<0.1 from chi-square analysis showed study heterogeneity, meta-analysis was performed using a random effects model and the possible source of heterogeneity was assessed using subgroup analysis. Sensitivity analysis removed the included literature one by one to determine whether the pooled effect values were stable and reliable.
Results
Search results and study characteristics
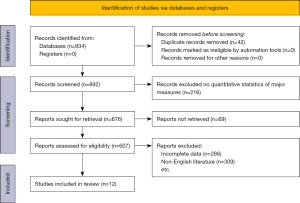
There were 934 records confirmed from the database, 42 duplicate records were removed, 892 records were obtained by screening, 676 records were obtained after 216 records were excluded due to data unclear, and 607 articles were obtained after retrieval. After excluding reviews, case reports, articles without study indicators, articles that did not meet the criteria, and incomplete data articles according to the inclusion and exclusion criteria, 12 available articles were finally obtained. The process is shown in Figure 1. Among the 12 articles available, 9 articles reported cardiac infarction, 10 articles reported mortality events, 6 articles reported stroke events, 8 articles reported revascularization, and only 2 articles reported the quality of patient life. All selected articles contained a clear diagnosis and clear inclusion and exclusion criteria. The basic characteristics included articles are shown in Table 1.
Table 1
| Author | Country | Year | Journal | PCI group (n) | ODT group (n) |
|---|---|---|---|---|---|
| Choi et al. (16) | Korea | 2021 | Texas Heart Institute Journal | 388 | 343 |
| Choi et al. (11) | Korea | 2017 | Journal of the American Heart Association | 305 | 335 |
| Choo et al. (12) | Korea | 2019 | Journal of Cardiology | 424 | 474 |
| De Bruyne et al. (17) | Belgium | 2014 | The New England Journal of Medicine | 447 | 441 |
| Guo et al. (18) | China | 2018 | Hellenic Journal of Cardiology | 125 | 201 |
| Juricic et al. (19) | Serbia | 2021 | International Heart Journal Association | 50 | 50 |
| Ladwiniec et al. (13) | UK | 2015 | Heart | 405 | 667 |
| Rha et al. (20) | Korea | 2018 | Yonsei Medical Journal | 412 | 410 |
| Tao et al. (21) | China | 2016 | Journal of Geriatric Cardiology | 143 | 98 |
| Werner et al. (14) | Germany | 2018 | European Heart Journal | 259 | 137 |
| Xaplanteris et al. (22) | Belgium | 2018 | The New England Journal of Medicine | 447 | 441 |
| Yang et al. (23) | Korea | 2016 | Circulation Journal | 883 | 664 |
PCI, percutaneous coronary intervention; ODT, optimal drug therapy.
Risk of bias
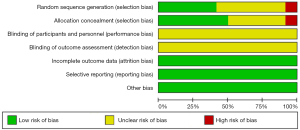
Only 6 articles described random sequence generation, and 6 articles did not describe random sequence generation. Seven articles reported allocation concealment, and 5 articles did not report allocation concealment. None of the articles reported the double-blind evaluation of personnel and participants and the blinded outcome. All articles described incomplete outcome data, selective reporting, and other biases. The evaluation results are shown in Figure 2.

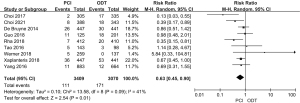
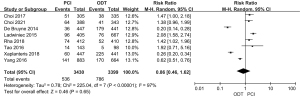
Incidence of cardiac infarction
According to the study screening criteria, a total of 9 articles were included in the analysis of the probability of MI in PCI and ODT for patients with stable coronary heart disease. The cases included 3,409 patients treated with PCI and 3,070 patients treated with ODT. The analysis results showed (P=0.09; I2=41%; RR =0.63; 95% CI: 0.45–0.90; Figure 3), indicating that the probability of MI between the two groups was heterogenous, so the random effects model was used for combined analysis. The comprehensive effect size test result was Z=2.54 and P=0.01, therefore the meta-analysis results showed that the PCI and ODT for their respective treatment groups had statistically significant effects on MI.
Mortality rate
A total of 10 articles were included to analyze the impact of PCI and ODT on the mortality of stable coronary heart disease. These articles included 4,113 patients treated with PCI and 4,010 patients treated with ODT. The heterogeneity analysis results showed (P=0.04; I2=49%; RR =0.51; 95% CI: 0.40–0.64; Figure 4), indicating a certain degree of heterogeneity in mortality between the two groups, therefore a random effects model was used for combined analysis. The comprehensive effect size test result was Z=5.77 and P<0.00001, so the meta-analysis results indicated that the PCI and ODT treatment for their respective groups had statistically significant effects on mortality.

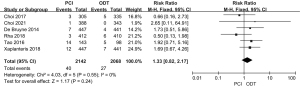
Stroke incidence
A total of 6 articles were included to analyze the impact of PCI and ODT of stable coronary heart disease on the occurrence of stroke. The articles included 2,142 patients treated with PCI and 2,068 patients treated with ODT. The heterogeneity analysis results showed (P=0.55; I2=0%; RR =1.33; 95% CI: 0.82–2.17; Figure 5), indicating that there was a certain homogeneity in the probability of stroke between the two groups, therefore the fixed effects model was used for joint analysis. The results of the comprehensive effect size test were Z=1.17 and P=0.24, therefore the meta-analysis results implied that the effects of PCI and ODT for their respective treatment groups on stroke incidence was not statistically significant.
Revascularization
A total of 8 articles were included that analyzed the impact of PCI and ODT on stable coronary heart disease on revascularization. The articles included 3,430 patients treated with PCI and 3,399 patients treated with ODT. The heterogeneity analysis results showed (P<0.00001; I2=97%; RR =0.86; 95% CI: 0.46–1.62; Figure 6), indicating that there was a certain heterogeneity in revascularization between the two groups, therefore the random effects model was used for combined analysis. The result of the comprehensive effect size test was Z=0.46 and P=0.65, therefore the meta-analysis results implied that PCI and ODT treatment had no statistically significant effects on revascularization for their respective treatment groups.
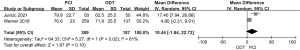
Quality of life
Only 2 articles included analyzed the impact of PCI and ODT of stable coronary heart disease on the quality of life of patients. The articles included 309 patients treated with PCI and 187 patients treated with ODT. The analysis results heterogeneity showed (P=0.02; I2=81%; MD =10.44; 95% CI: −1.84 to 22.73; Figure 7), indicating that there was a certain heterogeneity in the quality of life of patients between the two groups, therefore the random effects model was used for combined analysis. The comprehensive effect size test result was Z=1.67 and P=0.10, therefore the meta-analysis results implied that PCI and ODT treatment had no statistically significant impact on the quality of life of patients in their respective treatment groups.
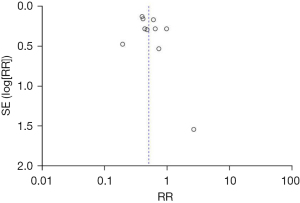
Publication bias
The mortality rate with the largest number of included research articles was selected for publication bias analysis. The funnel plot of mortality showed asymmetry, implying that there may be publication bias (Figure 8) and with a P value <0.05.
Risk of bias
In the included studies, 5 articles had a low risk of random sequence generation bias (14,16,17,19,22), 1 article had a high risk of random sequence generation bias (21), and 6 articles had an unclear risk of random sequence generation bias (11-13,18,20,23). The hidden bias of allocation for 6 articles was low risk (14,16,17,19,20,22), the for 1 article was high risk (21), and for 5 articles was unclear (11-13,18,23). The blinding bias of participants and personnel and the risk of blinding bias in outcome assessment in all articles was unclear. In addition, all studies were judged to have a low-risk of incomplete outcome data bias, selective reporting bias, and other biases (Figure 9).
Discussion
The incidence of stable coronary heart disease in the male population is 2–11%, the incidence in the female population is 3–9%, and the incidence is closely related to the increase in age (24). With the continuous development of PCI equipment and technology, the symptoms, quality of life, and prognosis of patients with stable coronary heart disease have been significantly improved (25). With the continuous improvement of the clinical application and treatment strategies of new drugs, drug therapy has also made significant progress in the treatment of stable angina pectoris (26-28). Although PCI is a minimally invasive operation, complications and even death may occur during and after the operation. PCI has complications such as stent shedding, stent thrombosis, and contrast nephropathy. In addition, drug therapy is still needed after PCI to prevent complications after PCI, which makes PCI surgery much higher risk and cost than drug therapy. In the selection of treatment strategies for stable coronary heart disease for patients with CTO, whether the efficacy of PCI treatment is better than drug treatment has always been a hot topic of discussion.
There is no standard definition of stable coronary artery disease (CAD). The trials included in this meta-analysis have different angiographic definitions of significant coronary artery stenosis, and only a few studies clearly describe the clinical symptoms of angina. Therefore, it may not reflect the stable CAD patients of the same population included in other trials. In addition, with advances in medical therapy, high-dose statins, and antiplatelet therapy have been used as standard care. Some studies (29,30) are recently published trials and show that there is no significant difference in all-cause mortality between PCI and ODT treatments. This lack of difference may underscore the progress and increasing use of effective medications for patients with stable CAD.
Research has reported that PCI is not significantly better than the best medical treatment to reduce the risk of all-cause mortality, cardiogenic death, and MI risk. However, another study confirmed that successful PCI treatment in CTO patients is associated with a higher long-term survival rate and a reduced risk of MI (31). Our meta-analysis used 12 studies, and the results of the analysis support that CTO patients benefit more after PCI treatment, and the mortality and MI rate of patients who underwent ODT was higher than those treated with PCI. The results of our meta-analysis at least have no evidence that PCI is not suitable for the treatment of CTO but shows that there may be some benefits. Our analysis results are consistent with some conclusions already reported (32).
This meta-analysis has several limitations. First, the literature included in this meta-analysis had research flaws, such as inconsistent types of stents used by patients, differences in drugs and dosages taken, and different follow-up times. Second, with the development of medical technology, some of the included trials cannot represent the curative effect of the currently defined treatment, which limits the results of the study. Third, the severity of vascular disease in patients with stable coronary heart disease varied, and the basic data included in the study was insufficient for further subgroup analysis. An explicit systematic review and meta-analysis were useful to evaluate the effect of PCI compared with ODT in patients with stable coronary heart disease. Large-scale, multi-center clinical studies are still needed to evaluate the efficacy of PCI and ODT in patients with stable coronary heart disease.
Conclusions
For patients with stable coronary heart disease and chronic coronary total occlusions, PCI is better than ODT at reducing the incidence of cardiogenic death and MI. However, PCI was not found to reduce the incidence of stroke. While our findings suggest that the incidence of revascularization and the improvement of the quality of life of patients are better with PCI than ODT, further studies are needed to confirm the efficacy of these treatments.
Acknowledgments
Funding: This work was funded by the National Natural Science Foundation of China (No. 81700297), and the Undergraduate Training Program for Innovation and Entrepreneurship, Soochow University (No. 202110285053).
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-222/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-222/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Claessen BE, Dangas GD, Weisz G, et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur Heart J 2012;33:768-75. [Crossref] [PubMed]
- Claessen BE, van der Schaaf RJ, Verouden NJ, et al. Evaluation of the effect of a concurrent chronic total occlusion on long-term mortality and left ventricular function in patients after primary percutaneous coronary intervention. JACC Cardiovasc Interv 2009;2:1128-34. [Crossref] [PubMed]
- Hoebers LP, Vis MM, Claessen BE, et al. The impact of multivessel disease with and without a co-existing chronic total occlusion on short- and long-term mortality in ST-elevation myocardial infarction patients with and without cardiogenic shock. Eur J Heart Fail 2013;15:425-32. [Crossref] [PubMed]
- Azzalini L, Jolicoeur EM, Pighi M, et al. Epidemiology, Management Strategies, and Outcomes of Patients With Chronic Total Coronary Occlusion. Am J Cardiol 2016;118:1128-35. [Crossref] [PubMed]
- Brilakis ES, Banerjee S, Karmpaliotis D, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv 2015;8:245-53. [Crossref] [PubMed]
- Christakopoulos GE, Christopoulos G, Carlino M, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol 2015;115:1367-75. [Crossref] [PubMed]
- Hoebers LP, Claessen BE, Elias J, et al. Meta-analysis on the impact of percutaneous coronary intervention of chronic total occlusions on left ventricular function and clinical outcome. Int J Cardiol 2015;187:90-6. [Crossref] [PubMed]
- Kearney K, Hira RS, Riley RF, et al. Update on the Management of Chronic Total Occlusions in Coronary Artery Disease. Curr Atheroscler Rep 2017;19:19. [Crossref] [PubMed]
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011;58:e44-122. [Crossref] [PubMed]
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165. [Crossref] [PubMed]
- Choi SY, Choi BG, Rha SW, et al. Percutaneous Coronary Intervention Versus Optimal Medical Therapy for Chronic Total Coronary Occlusion With Well-Developed Collaterals. J Am Heart Assoc 2017;6:006357. [Crossref] [PubMed]
- Choo EH, Koh YS, Seo SM, et al. Comparison of successful percutaneous coronary intervention versus optimal medical therapy in patients with coronary chronic total occlusion. J Cardiol 2019;73:156-62. [Crossref] [PubMed]
- Ladwiniec A, Allgar V, Thackray S, et al. Medical therapy, percutaneous coronary intervention and prognosis in patients with chronic total occlusions. Heart 2015;101:1907-14. [Crossref] [PubMed]
- Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J 2018;39:2484-93. [Crossref] [PubMed]
- Henriques JP, Hoebers LP, Råmunddal T, et al. Percutaneous Intervention for Concurrent Chronic Total Occlusions in Patients With STEMI: The EXPLORE Trial. J Am Coll Cardiol 2016;68:1622-32. [Crossref] [PubMed]
- Choi JY, Rha SW, Choi BG, et al. Percutaneous Coronary Intervention for Chronic Total Occlusion in Single Coronary Arteries. Tex Heart Inst J 2021;48:e197023. [Crossref] [PubMed]
- De Bruyne B, Fearon WF, Pijls NH, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 2014;371:1208-17. [Crossref] [PubMed]
- Guo L, Zhong L, Chen K, et al. Long-term clinical outcomes of optimal medical therapy vs. successful percutaneous coronary intervention for patients with coronary chronic total occlusions. Hellenic J Cardiol 2018;59:281-7. [Crossref] [PubMed]
- Juricic SA, Tesic MB, Galassi AR, et al. Randomized Controlled Comparison of Optimal Medical Therapy with Percutaneous Recanalization of Chronic Total Occlusion (COMET-CTO). Int Heart J 2021;62:16-22. [Crossref] [PubMed]
- Rha SW, Choi BG, Baek MJ, et al. Five-Year Outcomes of Successful Percutaneous Coronary Intervention with Drug-Eluting Stents versus Medical Therapy for Chronic Total Occlusions. Yonsei Med J 2018;59:602-10. [Crossref] [PubMed]
- Tao T, Wang H, Wang SX, et al. Long-term outcomes of high-risk elderly male patients with multivessel coronary disease: optimal medical therapy versus revascularization. J Geriatr Cardiol 2016;13:152-7. [PubMed]
- Xaplanteris P, Fournier S, Pijls NHJ, et al. Five-Year Outcomes with PCI Guided by Fractional Flow Reserve. N Engl J Med 2018;379:250-9. [Crossref] [PubMed]
- Yang JH, Kim BS, Jang WJ, et al. Optimal Medical Therapy vs. Percutaneous Coronary Intervention for Patients With Coronary Chronic Total Occlusion - A Propensity-Matched Analysis. Circ J 2016;80:211-7. [Crossref] [PubMed]
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation 2013;127:e6-e245. [Crossref] [PubMed]
- Gorenoi V, Hagen A. Perkutane Koronarintervention zusätzlich zu optimaler medikamentöser Therapie bei stabiler koronarer Herzkrankheit, DMW - Deutsche Medizinische Wochenschrift 2014;139:1039-45. [Crossref] [PubMed]
- Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2012;126:e354-471. [PubMed]
- Task Force Members. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949-3003. [Crossref] [PubMed]
- Risos L, Berkenboom G. Revascularization versus medical treatments in stable coronary artery disease: predicting the future of novel drug therapies for stable angina. J Cardiovasc Pharmacol 2014;63:213-7. [Crossref] [PubMed]
- Pijls NH, Fearon WF, Tonino PA, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol 2010;56:177-84. [Crossref] [PubMed]
- Pursnani S, Korley F, Gopaul R, et al. Percutaneous coronary intervention versus optimal medical therapy in stable coronary artery disease: a systematic review and meta-analysis of randomized clinical trials. Circ Cardiovasc Interv 2012;5:476-90. [Crossref] [PubMed]
- Gao L, Wang Y, Liu Y, et al. Long-term clinical outcomes of successful revascularization with drug-eluting stents for chronic total occlusions: A systematic review and meta-analysis. Catheter Cardiovasc Interv 2017;89:574-81. [Crossref] [PubMed]
- Ma Y, Li D, Li J, et al. Percutaneous coronary intervention versus optimal medical therapy for patients with chronic total occlusion: a meta-analysis and systematic review. J Thorac Dis 2018;10:2960-7. [Crossref] [PubMed]
(English Language Editor: C. Mullens)