
Ambulatory oxygen therapy with documented self-monitoring of oxygen use improves health status among patients with chronic obstructive pulmonary disease
Introduction
Hypoxemia can occur in association with end-stage chronic obstructive pulmonary disease (COPD), impairing quality of life and increasing mortality (1-3). Long-term home oxygen therapy is recommended for patients with chronic respiratory conditions if their arterial oxygen partial pressure (PaO2) is at least 55 mmHg with an oxygen saturation (SaO2) less than 88%, or if their PaO2 is between 55 and 60 mmHg or an SaO2 of 89%, with pulmonary hypertension, peripheral edema from congestive heart failure, or erythrocytosis (hematocrit >55%) (4). Previous studies have demonstrated a survival benefit associated with home oxygen therapy (5,6).
In Korea, national health care insurance has reimbursed the cost of home oxygen therapy since 2006 (7). However, a survey of COPD patients using home oxygen therapy revealed that low adherence levels, poor quality of life, and high health care service utilization (8). Also, physicians have noted a gap between the prescription and actual use of medical oxygen in real-world practice (9). Due to a lack of information about actual oxygen use, some physicians have made efforts to advocate for the development of oxygen therapy management strategies (10), but the educational materials that patients can easily access is still insufficient.
Therefore, we planned a pilot study to aid the development of a new strategy guiding home oxygen administration. This study aimed to explore the usefulness of this new strategy in terms of the patients’ well-being and oxygen use patterns. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1878/rc).
Methods
Study design and population
We previously reported on the status of home oxygen therapy for COPD patients in Korea (8). From the patients who participated in our previous study, we randomly selected 30 to participate in this pilot study. We asked the participants about the usefulness of the new strategy after 1 month of implementation.
New strategy for home oxygen therapy
Our new home oxygen service strategy was motivated by a self-management tool for patients with diabetes and hypertension. Although long-term home oxygen treatment increases the survival rate of COPD patients with severe hypoxemia, patient education on this topic is inadequate, even for those already receiving home oxygen treatment.
The proposed new home oxygen service strategy consists of three parts: (I) patient education materials; (II) self-monitoring with an “oxygen note”; and (III) provision of ambulatory oxygen. The educational materials cover the basic concept of oxygen therapy, background information about oxygen concentrators, cleaning and maintenance methods for oxygen generators, ambulatory oxygen, safety issues surrounding oxygen therapy, oxygen use when traveling (road or air travel), and the costs associated with oxygen therapy. The materials include illustrations to aid with understanding. Three pulmonology specialists participated in the development of the educational materials.
We also developed an oxygen note. Three COPD management experts developed the oxygen note, which is composed of three sections. The first section (“Guide for Correct Home Oxygen Treatment”) consists of brief guidance about oxygen therapy. The second section consists of a patient-specific data entry form to be filled out by the patient. Patients using home oxygen services are to keep a log of their SaO2, as well as their daily oxygen administration time and amount, similar to the logs kept by patients with diabetes mellitus and hypertension documenting their blood sugar levels and blood pressure, respectively. We believe this to be the essential component of the oxygen note. The third section consists of a patient evaluation form (to be filled out by a visiting nurse) and a safety evaluation form (to be filled out by oxygen providers). The participants of this pilot study documented their SaO2 (at rest, during sleep, and during ambulation) and oxygen use times and amounts on the daily sheets. We provided ambulatory oxygen devices and pulse oximeters to help the patients maximize their daily activity levels and self-monitor their SaO2.
Evaluation of a 1-month trial of the new management strategy
After a 1-month trial of the new management strategy, we used a structured questionnaire to query the participants about the strategy’s usefulness and effect on their health. We used the EuroQoL-5 Dimension (EQ-5D) and COPD assessment test (CAT) tools to assess general health status and COPD-related health status, respectively. The modified Medical Research Council (mMRC) dyspnea scale was used to rate dyspnea severity. We also evaluated the actual use of home oxygen and ambulatory oxygen therapy as well as the patients’ satisfaction with educational materials and oxygen notes.
Statistical analysis
Data were analyzed using SPSS for Windows, version 23.0 (IBM Corp., Armonk, NY, USA). Categorical and continuous data are presented as n (%) and mean ± standard deviation. Differences in continuous variables, such as each component of the CAT score and the duration and flow rate of home oxygen use, were analyzed using independent t-tests. P values less than 0.05 were considered statistically significant.
Ethical statement
This study was approved by the institutional review board of Hallym University Sacred Hospital (IRB No. 2016-I020), Anyang, South Korea. All patients provided written informed consent before enrollment. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Results
Baseline participant characteristics
Of the 30 patients initially enrolled in the study, one was unable to complete the questionnaire because of hospitalization due to pneumothorax at the end of the 1-month trial. Therefore, 29 patients completed this pilot study. The mean age was 69.6±9.7 years (range, 50–85 years), and the majority of participants (n=18, 62.1%) were men. Twenty-eight patients (96.6%) had a CAT score of 10 or higher and an mMRC score of 2 or higher. Twenty-two patients (75.9%) met the respiratory impairment criteria for reimbursement via the national health insurance system (Table 1) (11).
Table 1
| Characteristics | Value |
|---|---|
| Total | 29 (100.0) |
| Age, years | 69.6±9.9 |
| Sex, male | 18 (62.1) |
| mMRC ≥2 | 28 (96.6) |
| CAT score ≥10 | 28 (96.6) |
| Respiratory impairment (+)* | 22 (75.9) |
Data are expressed as mean ± standard deviation (SD) or N (%). *, respiratory impairment: respiratory impairment grading according to The Act on Welfare of Persons with Disabilities. CAT, COPD assessment test; COPD, chronic obstructive pulmonary disease; mMRC, modified medical research council dyspnea scale.
Changes in dyspnea and quality of life
After the trial period, 10 (34.5%) and 23 (79.3%) patients exhibited improved mMRC and CAT scores, respectively (Table 2). In particular, the proportion of patients with severe dyspnea (mMRC grade 4) decreased markedly (62.1% → 41.4%) (Figure 1). Regarding changes in general health status according to the EQ-5D, 12 patients (41.4%) improved in terms of the mobility and self-care domains, and 3 patients (10.3%) reported deteriorations in both domains. Additionally, 9 patients (31.0%) reported improvements in routine activities, 8 (27.6%) in pain or discomfort, and 11 (37.9%) in anxiety or depression (Table 2). In terms of the individual components of the CAT score overall, patients reported meaningful improvements in the “cough”, “sputum”, “chest tightness”, “dyspnea on exertion”, “sleep”, and “energy” items. However, the “activity at home” and “leaving home” components did not improve significantly despite the provision of ambulatory oxygen (Table 3).
Table 2
| Variables | Aggravated | Not changed | Improved |
|---|---|---|---|
| mMRC | 13.8 | 51.7 | 34.5 |
| CAT | 17.2 | 3.4 | 79.3 |
| EQ-5D: mobility | 10.3 | 48.3 | 41.4 |
| EQ-5D: self-care | 10.3 | 48.3 | 41.4 |
| EQ-5D: usual activities | 6.9 | 62.1 | 31.0 |
| EQ-5D: pain/discomfort | 6.9 | 65.5 | 27.6 |
| EQ-5D: anxiety/depression | 17.2 | 44.8 | 37.9 |
mMRC, modified medical research council dyspnea scale; CAT, COPD assessment test; COPD, chronic obstructive pulmonary disease; EQ-5D. EuroQol-5 dimension.
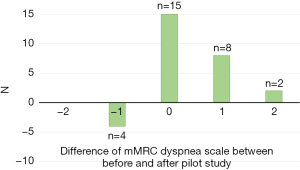
Table 3
| Variables | Before pilot study | After pilot study | P value |
|---|---|---|---|
| Cough | 3.17±1.20 | 1.69±1.28 | <0.001 |
| Sputum | 3.62±1.01 | 2.45±1.30 | 0.002 |
| Chest tightness | 3.28±1.56 | 2.55±1.39 | 0.033 |
| Dyspnea on exertion | 4.83±0.47 | 2.55±1.38 | <0.001 |
| Activity at home | 3.83±1.20 | 3.28±1.73 | 0.083 |
| Leaving home | 4.28±1.07 | 4.00±1.28 | 0.185 |
| Sleep | 3.31±1.71 | 2.48±1.70 | 0.035 |
| Energy | 4.03±1.09 | 3.45±1.40 | 0.042 |
| Total | 30.3±6.1 | 24.7±6.9 | 0.001 |
Data are expressed as mean ± standard deviation. CAT, COPD assessment test; COPD, chronic obstructive pulmonary disease.
Changes in home oxygen use patterns
The patterns of home oxygen changed over the course of the trial period, with significant increases in both the mean time and amount of ambulatory oxygen used. However, when patients were at rest, the mean oxygen use time and flow rate decreased. There were no significant changes in oxygen use during sleep (Table 4).
Table 4
| Variables | Before pilot study | After pilot study | P value |
|---|---|---|---|
| At rest | |||
| Duration (hours) | 15.6±8.21 | 11.2±6.40 | 0.014 |
| Flow rate (L/min) | 2.08±1.63 | 1.81±0.58 | 0.203 |
| During exercise | |||
| Duration (hours) | 1.08±2.26 | 3.05±4.76 | 0.025 |
| Flow rate (L/min) | 0.51±0.80 | 1.77±0.96 | <0.001 |
| During sleep | |||
| Duration (hours) | 7.41±2.85 | 7.84±3.65 | 0.301 |
| Flow rate (L/min) | 1.62±0.63 | 1.74±0.65 | 0.239 |
Data are expressed as mean ± standard deviation.
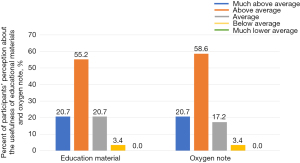
During the trial period, all participants completed their oxygen notes every day. More than three-quarters of the participants thought that the educational materials and oxygen note were helpful (Figure 2). Even though about half of the participants (n=14, 48.3%) perceived that they used the home oxygen by the end of the trial period than they did before the study, only 2 of these 14 participants documented actual increases in supplemental oxygen use.
Discussion
For this study, we developed a new home oxygen therapy management strategy for COPD patients. Our pilot study used educational materials and an oxygen note for self-monitoring and enhancing the patients’ knowledge and self-management skills. Our new strategy improved dyspnea and quality of life among the COPD patients who participated in the study, especially the most dyspneic patients. Moreover, this pilot study brought about changes in the patients’ oxygen use patterns.
Dyspnea is a typical COPD symptom that leads to activity limitations and worsens quality of life. Mitigating dyspnea is critical in COPD management (12-14). Home oxygen therapy is well known to decrease mortality rates in selected COPD populations (5,6). Additionally, it improves dyspnea and the quality of life in COPD patients (15). Our pilot study confirmed these findings, that is, improving dyspnea and quality of life. Our new strategy improved dyspnea in 34.5 % of enrolled patients and the proportion of the patients with mMRC 4 of dyspnea. Additionally, the strategy improved the quality of life according to data collected using the CAT and EQ-5D tools. The participants reported improvements in the mobility, self-care, and routine activity domains of the EQ-5D. The total and respiratory symptom domains of the CAT also improved in magnitude by more than the minimal clinically important difference (16). The CAT is a short, simple assessment tool for evaluating the symptom burden of COPD in daily clinical practice to check health status assessment and communicate between patients and healthcare providers. The CAT score is known to be associated with the mMRC dyspnea score, the degree of anxiety and depression, activity scale (e.g. incremental shuttle walk test) (17). The improvement of CAT score in our study suggests that our new home oxygen strategy may have significant psychological and physical effects on patients with COPD.
Adherence to home oxygen is crucial for hypoxemic COPD patients to improve survival. Previous studies have demonstrated that maintaining oxygen therapy for at least 15–18 hours per day yields survival benefits (5,6). However, the exact duration required to lower the risk of death is not known. Furthermore, there are often significant discrepancies between prescribed oxygen use durations and actual use (8). We designed an oxygen note for self-monitoring to minimize this difference. However, the self-reported mean oxygen use time during rest decreased over the course of the study period. Only two patients increased their oxygen use times, even though 14 patients thought that they had increased their oxygen use times. Therefore, we could not determine the patient’s exact oxygen use times based solely on the patients’ statements, and we need more objective monitoring tools to increase adherence to oxygen.
Low adherence resulting from an inadequate understanding of oxygen therapy negatively affects the clinical outcomes associated with oxygen therapy (18). An accurate understanding of the treatment, awareness of its benefits, and regular follow-up and support from oxygen therapy providers are critical factors for increasing long-term adherence to oxygen therapy (19,20). Despite the decrease in the mean oxygen self-administration time, all of the participants used the oxygen note every day during the trial period. This everyday self-monitoring using the oxygen note, along with the concise guidance regarding oxygen therapy in the oxygen note, evidently improved the patients’ awareness of the principles and importance of oxygen treatment. Therefore, we think our findings emphasize the importance of education for patients requiring ambulatory oxygen therapy, similar to the educational requirements for patients with other chronic diseases.
Patient education is an essential component of efficient chronic disease management (21,22). However, the reality of patient education about oxygen therapy in Korea is disappointing (9). Therefore, we developed educational materials about home oxygen therapy covering basic concepts, background information about oxygen concentrators, cleaning and maintenance methods for oxygen generators, ambulatory oxygen, safety issues surrounding oxygen therapy, oxygen use when traveling, and the costs associated with oxygen therapy. As printed materials are relatively low-cost and potentially useful tools for patient self-education (23), we provided the participants with printed versions of the educational materials. We think that these educational materials, along with the oxygen note, improved the patients’ awareness of oxygen therapy and helped them use the home oxygen more effectively. Indeed, most of the COPD patients who participated in this study reported that our educational materials were helpful for their self-management.
As this was a pilot study, the number of patients who participated in this study was small and the study was conducted for one-month. During this study, it was conducted as an observational study and was just checked about the improvement of dyspnea scale or quality of life using a questionnaire survey. Therefore, we can’t show the detailed protocol including the intervention. It needs to be proven through a larger, prospective study in the future. However, the study demonstrated the importance of patient education and a potential role of self-monitoring using the oxygen note. Furthermore, our study suggested the necessity of developing devices to monitor adherence to home oxygen therapy.
Conclusions
We developed and evaluated a new home oxygen service strategy. The new home oxygen service strategy improved both the duration of oxygen usage and the health status of COPD patients. Future larger-scale, longer-term prospective research is warranted to validate our proposed strategy. We think that this strategy can be an appropriate management plan for COPD patients undergoing home oxygen therapy.
Acknowledgments
Funding: This study was supported by grants from the Korea Centers for Disease Control and Prevention and study code was 2015-E330011-00.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1878/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1878/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1878/coif). CKR and KSJ serve as unpaid editorial board members of Journal of Thoracic Disease. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the institutional review board of Hallym University Sacred Hospital (IRB No. 2016-I020), Anyang, South Korea. All patients provided written informed consent before enrollment.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim V, Benditt JO, Wise RA, et al. Oxygen therapy in chronic obstructive pulmonary disease. Proc Am Thorac Soc 2008;5:513-8. [Crossref] [PubMed]
- Kent BD, Mitchell PD, McNicholas WT. Hypoxemia in patients with COPD: cause, effects, and disease progression. Int J Chron Obstruct Pulmon Dis 2011;6:199-208. [PubMed]
- Gulbas G, Gunen H, In E, et al. Long-term follow-up of chronic obstructive pulmonary disease patients on long-term oxygen treatment. Int J Clin Pract 2012;66:152-7. [Crossref] [PubMed]
- Hardinge M, Annandale J, Bourne S, et al. British Thoracic Society guidelines for home oxygen use in adults. Thorax 2015;70:i1-43. [Crossref] [PubMed]
- Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Nocturnal Oxygen Therapy Trial Group. Ann Intern Med 1980;93:391-8. [Crossref] [PubMed]
- Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Party. Lancet 1981;1:681-6. [PubMed]
- Lee K. Home oxygen therapy in patients with chronic obstructive pulmonary disease. The Korean Journal of Medicine 2007;73:353-60.
- Kim JK, Jang SH, Park S, et al. Current Situation of Home Oxygen Therapy for Chronic Obstructive Pulmonary Disease Patients in Korea. J Korean Med Sci 2020;35:e12. [Crossref] [PubMed]
- Kim Y, Kim HI, Park JY, et al. Korean physician prescription patterns for home oxygen therapy in chronic obstructive pulmonary disease patients. Korean J Intern Med 2022;37:119-26. [Crossref] [PubMed]
- Suntharalingam J, Wilkinson T, Annandale J, et al. British Thoracic Society quality standards for home oxygen use in adults. BMJ Open Respir Res 2017;4:e000223. [Crossref] [PubMed]
- Ministry of Government Legislation. National Law Information Center. Enforcement Rule of The Act on Welfare of Persons with Disabilities. Accessed April 22, 2019. Available online: http://www.law.go.kr/lsInfoP.do?lsiSeq=206271&efYd=20190101#0000
- Selecky PA, Eliasson CA, Hall RI, et al. Palliative and end-of-life care for patients with cardiopulmonary diseases: American College of Chest Physicians position statement. Chest 2005;128:3599-610. [Crossref] [PubMed]
- Lanken PN, Terry PB, Delisser HM, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med 2008;177:912-27. [Crossref] [PubMed]
- Marciniuk DD, Goodridge D, Hernandez P, et al. Managing dyspnea in patients with advanced chronic obstructive pulmonary disease: a Canadian Thoracic Society clinical practice guideline. Can Respir J 2011;18:69-78. [Crossref] [PubMed]
- Ekström M, Ahmadi Z, Bornefalk-Hermansson A, et al. Oxygen for breathlessness in patients with chronic obstructive pulmonary disease who do not qualify for home oxygen therapy. Cochrane Database Syst Rev 2016;11:CD006429. [Crossref] [PubMed]
- Vitacca M, Malovini A, Balbi B, et al. Minimal Clinically Important Difference in Barthel Index Dyspnea in Patients with COPD. Int J Chron Obstruct Pulmon Dis 2020;15:2591-9. [Crossref] [PubMed]
- Dodd JW, Hogg L, Nolan J, et al. The COPD assessment test (CAT): response to pulmonary rehabilitation. A multicentre, prospective study. Thorax 2011;66:425-9. [Crossref] [PubMed]
- Ringbaek TJ, Lange P. The impact of the Danish Oxygen Register on adherence to guidelines for long-term oxygen therapy in COPD patients. Respir Med 2006;100:218-25. [Crossref] [PubMed]
- Cullen DL. Long term oxygen therapy adherence and COPD: what we don't know. Chron Respir Dis 2006;3:217-22. [Crossref] [PubMed]
- Katsenos S, Constantopoulos SH. Long-Term Oxygen Therapy in COPD: Factors Affecting and Ways of Improving Patient Compliance. Pulm Med 2011;2011:325362. [Crossref] [PubMed]
- Epping-Jordan JE, Pruitt SD, Bengoa R, et al. Improving the quality of health care for chronic conditions. Qual Saf Health Care 2004;13:299-305. [Crossref] [PubMed]
- Holman H, Lorig K. Patients as partners in managing chronic disease. Partnership is a prerequisite for effective and efficient health care. BMJ 2000;320:526-7. [Crossref] [PubMed]
- Harris M, Smith B, Veale A. Printed patient education interventions to facilitate shared management of chronic disease: a literature review. Intern Med J 2005;35:711-6. [Crossref] [PubMed]


