Efficacy and safety of human fibrinogen-thrombin patch (Tachosil®) in the management of diffuse bleeding after chest wall and spinal surgical resection for aggressive thoracic neoplasms
Introduction
In order to obtain a successful surgical outcome, a proper and effective haemostasis is crucial in all fields of surgery. Major bleeding is usually controlled by standard surgical techniques (e.g., coagulation, ligation of blood vessels, clips) whilst a diffuse bleeding represents a serious problem that usually cannot be managed in the same way. Among the new systems aiding the control of bleeding, fibrin sealants (FS) play an important role, which has been recognized in a vast range of surgical fields. FS are generally made by two major components, fibrinogen and thrombin. Through the fibrinogen activation by thrombin, FS mimic the coagulation cascade final process with the formation of a semi-rigid clot (1). The recognition of FS haemostatic action allowed their use across several fields of surgery including abdominal and hepatic, urologic, cardiovascular and thoracic ones (2).
Several articles (3-5) reported the efficacy of TachoSil® (Takeda Austria GmbH, Linz, Austria) in reducing the risk of postoperative air leak after pulmonary resections, even in high-risk patients (6) although its haemostatic properties were only occasionally demonstrated in General Thoracic Surgery.
We aimed to report the successful haemostatic activity of TachoSil® in cases of diffuse bleeding after surgical resection of locally invasive primary lung cancers and malignant recurrent solitary fibrous tumor (SFT) of the pleura. For this purpose, we evaluated: (I) the amount of pleural fluid in each postoperative day; (II) the day of chest drainage removal; (III) the radiological presence of thoracic hematoma/haemothorax at the postoperative bedside chest X-ray.
Case presentation
Between March 2013 and December 2014 three patients (all males, mean age 71.6 years) underwent a surgical resection of two primary lung cancers and one malignant recurrent SFT of the pleura, with chest wall and spine invasion. All patients received induction chemotherapy (platinum based cycles) and radiotherapy (45 Gy). All the interventions were conducted through a posterolateral thoracotomy. In all three cases we were able to perform a right upper lobectomy with chest wall resection (median number of resected ribs: 4) and with a partial resection of the vertebral body (Figures 1-3). A systematic lymphadenectomy was achieved in all three patients. In one patient (Figure 3), spinal instrumentation stabilization was required due to the enlarged spinal resection.
A diffuse bleeding on the resected spine body surface was observed in all cases, and it was managed through traditional haemostatic aids, such as hot swabs and electrocautery, followed by the apposition of large sized TachoSil® (mean number: 2). At the end of the surgery, two 28-Ch chest drains, one anterior and one posterior, were connected to a digital evaluation of air leak (DrentechTM Palm Evo; Redax, Poggio Rusco, MN, Italy) and placed under suction.
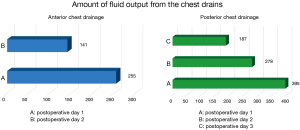
Our department policy for chest drain removal is as follows: (I) no air leak; (II) overall output ≤250 mL/24 hours; (III) no active bleeding or presence of chylous liquid; (IV) complete re-expansion of lung parenchyma at the postoperative bedside chest X-ray. The anterior chest tubes were removed in the second postoperative day, the posterior ones in day three.
At postoperative day one and two, the mean fluid output from the anterior chest drain was 225 mL [standard deviation (SD): 57 mL] and 142 mL (SD: 43 mL), respectively, whereas the mean fluid output from the posterior chest drain at postoperative day 1, 2 and 3 was as follow: 395 mL (SD: 26 mL), 278 mL (SD: 30 mL) and 187 mL (SD: 25 mL). Figure 4 shows the amount of pleural fluid output from each chest drain.
No radiological signs of haemothorax or thoracic hematoma were found at the chest X-ray of all three patients. Patients were discharged from the hospital in 8th, 7th and 10th postoperative day, respectively.
Discussion
This brief report demonstrates TachoSil®’s efficacy to control diffuse bleeding in an unusual field of General Thoracic Surgery. To the best of our knowledge this is the first time in which this FS was used on the bleeding surface of resected vertebral bodies invaded by primary lung cancer and SFT of the pleura.
In fact, due to the preoperative induction treatment (chemotherapy and radiotherapy) to which our patients were submitted to, they were considered at high-risk for bleeding. Chest drainages were removed in 2nd and 3rd postoperative day in all cases and no radiological signs of haemothorax or hematoma were found at the postoperative chest X-ray.
The haemostatic efficacy of TachoSil® has been seldom reported in other surgical fields.
Only one randomized controlled study that compared TachoSil® with the Argon beamer as a haemostatic aid during elective hepatic surgery has been published (7). In this study, Authors demonstrated that TachoSil® was significantly superior in the time of haemostasis (3.9 vs. 6.3 min) and that the postoperative haematic output was significantly lower in the group of patients treated with TachoSil®. In order to reduce the risk of reoperation for secondary haemorrhage, the Brussels paediatric liver transplant team recommended its use on the split liver surface (8).
Lorenz et al. (9) used TachoComb® in case of pancreatic resections for carcinoma, chronic pancreatitis and necrotizing ones and, especially in the latter ones, were able to demonstrate its efficacy in controlling the retroperitoneal bleeding.
Several case reports were published in cardiac surgery: the successful defect repair with TachoSil® as an alternative to infarctectomy and myocardial suture has been reported (10,11). Also, TachoComb® was successfully used in case of cardiac penetrating trauma (12) or following atrio-ventricular disruption during mitral valve surgical repair (13).
The successful management of bleeding following a partial nephrectomy for renal cell carcinoma has been reported in a multicentre prospective randomized trial in which TachoSil® proved to be significantly superior than the standard sutures to achieve haemostasis (14).
On the other hand, TachoSil® has been routinely used in General Thoracic Surgery to control postoperative air leaks, especially in high-risk patients (e.g., severe emphysema; re-interventions). In fact, not only TachoSil® reduces the air leak volume, but allows an early removal of chest drains, a speedy recovery and an early discharge from the hospital (3,4,6). Such results have a significant impact on the reduction of both risk of postoperative clinical complications (15,16) and the overall hospitalization costs (17).
In conclusion, this is the first report of TachoSil®’s efficacy to control diffuse bleeding in the resected chest wall and vertebral body surface invaded by thoracic malignancies (primary lung cancer and recurrent malignant SFT of the pleura). A more substantial diffusion of this product seems appropriate in General Thoracic Surgery, not only in air leak control, but also to reduce the risk of chest wall or pulmonary parenchyma bleeding following major invasive surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Radosevich M, Goubran HI, Burnouf T. Fibrin sealant: scientific rationale, production methods, properties, and current clinical use. Vox Sang 1997;72:133-43. [PubMed]
- Sierra DH. Fibrin sealant adhesive systems: a review of their chemistry, material properties and clinical applications. J Biomater Appl 1993;7:309-52. [PubMed]
- Anegg U, Lindenmann J, Matzi V, et al. Efficiency of fleece-bound sealing (TachoSil) of air leaks in lung surgery: a prospective randomised trial. Eur J Cardiothorac Surg 2007;31:198-202. [PubMed]
- Droghetti A, Schiavini A, Muriana P, et al. A prospective randomized trial comparing completion technique of fissures for lobectomy: stapler versus precision dissection and sealant. J Thorac Cardiovasc Surg 2008;136:383-91. [PubMed]
- Marta GM, Facciolo F, Ladegaard L, et al. Efficacy and safety of TachoSil® versus standard treatment of air leakage after pulmonary lobectomy. Eur J Cardiothorac Surg 2010;38:683-9. [PubMed]
- Filosso PL, Ruffini E, Sandri A, et al. Efficacy and safety of human fibrinogen-thrombin patch (TachoSil®) in the treatment of postoperative air leakage in patients submitted to redo surgery for lung malignancies: a randomized trial. Interact Cardiovasc Thorac Surg 2013;16:661-6. [PubMed]
- Frilling A, Stavrou GA, Mischinger HJ, et al. Effectiveness of a new carrier-bound fibrin sealant versus argon beamer as haemostatic agent during liver resection: a randomised prospective trial. Langenbecks Arch Surg 2005;390:114-20. [PubMed]
- Lacanna F, Brunati A, Reding R. A new biological mesh for cut surface hemostasis in liver transplantation using technical variants. Pediatr Transplant 2008;12:520-1. [PubMed]
- Lorenz D, Scheele J. The use of collagen fleece (Tachocomb) in pancreatic surgery. Z Exp Chir Transplant Kunstliche Organe 1990;23:93-4. [PubMed]
- Galajda Z, Fülöp T, Péterffy A. Subacute left ventricular rupture complicated by free wall rupture: repair with a TachoComb sheet and Tissucol glue. J Thorac Cardiovasc Surg 2002;123:1014-5; author reply 1015-6. [PubMed]
- Kudo M, Misumi T, Koizumi K, et al. A surgical case of ventricular septal perforation after repairing left ventricular free wall rupture. Ann Thorac Cardiovasc Surg 2005;11:121-4. [PubMed]
- Toda K, Yoshitatsu M, Izutani H, et al. Surgical management of penetrating cardiac injuries using a fibrin glue sheet. Interact Cardiovasc Thorac Surg 2007;6:577-8. [PubMed]
- Schuetz A, Schulze C, Wildhirt SM. Off-pump epicardial tissue sealing--a novel method for atrioventricular disruption complicating mitral valve procedures. Ann Thorac Surg 2004;78:569-73; discussion 573-4. [PubMed]
- Siemer S, Lahme S, Altziebler S, et al. Efficacy and safety of TachoSil as haemostatic treatment versus standard suturing in kidney tumour resection: a randomised prospective study. Eur Urol 2007;52:1156-63. [PubMed]
- Refai M, Brunelli A, Salati M, et al. The impact of chest tube removal on pain and pulmonary function after pulmonary resection. Eur J Cardiothorac Surg 2012;41:820-2; discussion 823. [PubMed]
- Brunelli A, Cassivi SD, Halgren L. Risk factors for prolonged air leak after pulmonary resection. Thorac Surg Clin 2010;20:359-64. [PubMed]
- Brunelli A, Salati M, Refai M, et al. Risk-adjusted econometric model to estimate postoperative costs: an additional instrument for monitoring performance after major lung resection. J Thorac Cardiovasc Surg 2007;134:624-9. [PubMed]