Reduce chest pain using modified silicone fluted drain tube for chest drainage after video-assisted thoracic surgery (VATS) lung resection
Introduction
Minimally invasive surgical techniques, particularly video-assisted thoracic surgery (VATS), have been performed more than 20 years. During that time, many advances have been made in the field of anesthesia, perioperative care, and postoperative (PO) rehabilitation. However, PO pain pattern and management of it are still incompletely explored. After VATS lung resection, placement of chest tube is routine. The aims are the monitoring of bleeding, the removal of fluids and air and to reexpand the residual lung routinely. While the procedure is performed under optimal conditions, which minimizes risks of PO complications, the chest pain in exist persistently. On the other hand, chest pain usually requires in-hospital special care, with the consequent costs implied.
Chest tube placement is one of the most important factors leading to the persistent chest pain after VATS lung resection, although the incision has been minimized. Clinical observation found that the majority of PO chest pain after lung resection occurred in the chest drainage site and the pain relief immediately after removal of chest drain tube. Therefore, any attempts at modification of chest drainage might decrease the likelihood of chest pain and decrease the necessity of hospitalization of patients.
A large bore [28−32] semi-rigid plastic chest tube is frequently advocated after thoracotomy, because the tube diameter is considered directly related to clearance of fluid and air, however, the large bore tubes pass through the intercostal spaces, create great discomfort for the patient who often experience pain, as a result there may prolong the hospital stay. Small caliber, flexible catheters (16 F) have successfully used for spontaneous pneumothorax and pleural effusion but no evidence of their effectiveness in patients after thoracotomy have been published.
We hypothesized that the application of silicone fluted drain tube to the chest drainage may improve the chest pain after VATS lung resection. Therefore, the principal objective of this prospective, randomized study was to assess the effect of modified silicone fluted drain tube application to chest tubes on the efficacy, the risk of complications and PO pain relief in VATS lung resection patients.
Patients and methods
Design of experiment, time and setting
A prospective, randomized and controlled clinical trial was carried out in the Department of Thoracic Surgery of Beijing Chaoyang Hospital between March 2015 and June 2015. The data were collected prospectively and the patients were randomly divided into experimental group (using the silicone fluted drain tubes for chest drainage) and control group (using a large bore semi-rigid plastic drain tubes for chest drainage).
Inclusive criteria
(I) Patients need VATS lobectomies, VATS wedge resection or lung and VATS lung biopsy, depending on their condition; (II) without cardiac dysfunction, liver dysfunction and renal dysfunction; (III) no pulmonary infection, pyothorax, malignant pleural tumor and pleuritis; (IV) preoperative blood routine tests and coagulation function of patients are normal; (V) with operative indication.
Exclusive criteria
(I) Fever [temperature (T) >37.5 °C]; (II) patients with human immunodeficiency virus (HIV), hepatitis B virus (HBV) and syphilis infection; (III) history of drug abuse (such as stimulants, sedatives and opioids); (IV) allergies to rubber products; (V) with psychiatric history; (VI) pregnant women or infants; (VII) the conditions of patients are too critical to appraise the performance of drain tubes; (VIII) malignant pleural effusion or intrapleural injection.
Protocol
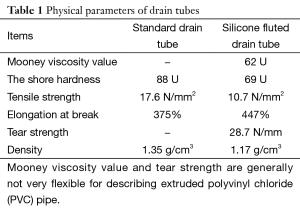
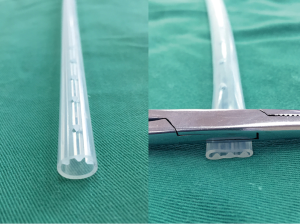
Patients hospitalized underwent preoperative examinations, according to the routine of the Department of Thoracic Surgery of our hospital. Examinations contained blood routine test, blood biochemical tests, coagulation function, HIV test, HBV test, Treponema pallidum test, electrocardiogram (ECG) and chest computed tomography (CT) scan. Then all enrolled patients received VATS lung resection (lobectomies or wedge resection). Once the thoracic procedure was completed, with special care to check hemostasis and to close any air leak, a silicone fluted drain tube (Table 1) was inserted through a 0.5-cm skin incision. To adapt silicone fluted drain tube for chest drainage, we made some modifications to the original design: (I) make a couple of side apertures, diameter 5 millimeters, 3 cm apart; (II) the last apertures were marked as triangle to fix drain tubes.
Full table
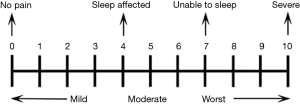
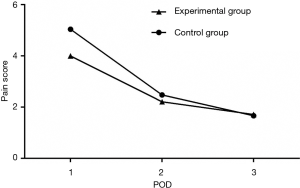
In the PO period, the drains and the chest drainage unit were checked twice a day for tidaling, bubbling, or fluid level in the waterseal chamber by a surgeon, and checked again by nurses during their rounds. The daily outputs were recorded. Especially pain was assessed at 7:00 A.M. on first to fifth PO day, using a visual analog scale (VAS) (1,2) (Figure 1). When responding to a VAS item, patients specified their pain intensity by indicating a position along a continuous line between two end-points. The left extremity of line indicates the absence of pain and the right extremity indicates the worst pain ever experienced. In order to accurately evaluate the operative pain, analgesic is not allowed 12 hours before pain assessment or the patient would be excluded. Allowed analgesics include tramadol, bucinnazine or pethidine. The drainage was removed when the daily production was less than 150−200 mL of clear fluid without bubbles at cough, whereas the X-ray showed a full expansion of the residual lung.
Statistical analysis
All data were analyzed with a statistical software package (SPSS for Windows version 17.0; SPSS, Chicago, IL, USA). Values were expressed as mean ± standard deviation for continuous variables, and as frequencies and percentages for categorical variables. Mean values were compared using an independent t-test. While a rank sum test were used if data don’t follow a normal distribution. Categorical variables were analyzed using Fisher’s exact test and chi-square test. All statistical tests were two-sided; P<0.05 was considered to be statistically significant.
Ethics statement
This study was approved by the institutional review board of the Beijing Chaoyang Hospital (2015-Sci-3) and was registered with the Chinese Clinical Trial Registry (ChiCTR-IOR-15006121). This study was carried out according to the principles of the Declaration of Helsinki, 2000. We performed a prospective, randomized, controlled study, and informed written consent was obtained from each patient before inclusion in the study.
Results
General data of the patients
Between March 2015 and June 2015, a total of 50 consecutive patients underwent lung resections (wedge resection or lobectomy). Owing to exclusive criteria, three patients were excluded from the study for injecting talc intrapleurally. The remaining 47 patients were included in the final analysis. Patients’ mean age at the time of surgery was 36.6±15.8 years for control group and 42.6±21.2 years for experimental group. There were 26 males (55.3%) and 21 females (44.7%). The pathologic diagnosis included pneumothorax, benign pulmonary disease, and lung cancer. The two groups were comparable in terms of mean age, gender, type of surgical procedures and disease distribution. Baseline data for both groups are presented in Table 2.
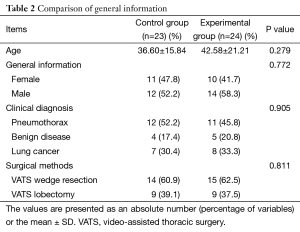
Full table
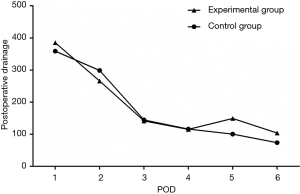
Postoperative (PO) drainage management
The volumes of drainage from day 1 to day 6 after surgery were shown in Figure 2. There was no statistical difference between the two groups. It revealed a significant trend toward less pain in the experimental group at the early postoperatively when compared to control group (Figure 3). While the gap of pain score was likely to narrow with time gradually and these situations were not prominent between the two groups to the day 5th after surgery. The rate of fever (T >37.4 °C) were slightly higher in control group, although the difference was not statistically significant (87.0% vs. 45.8%; P=0.05). Nevertheless, the rate of moderate fever (T >38.4 °C) of both groups were approximate yet. To analyze the raw data, it found that application of the modified silicone fluted drain tube was superior in the risk of mild pneumothorax. But the results were not statistically significant (P=0.212).
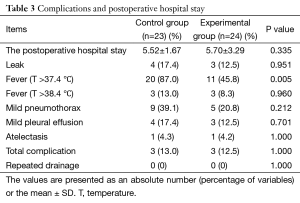
There were no major PO complications in both groups (Table 3). The mild complications in both control group and experimental group were comparable in terms of air leak (17.4% vs. 12.5%, P=0.951), pneumothorax (39.1% vs. 20.8%, P=0.212), pleural effusion (17.4% vs. 12.5%, P=0.701), and atelectasis (4.3% vs. 4.2%, P=1.00). Morbidity rate was 13% in control group and 12.5% in experimental group (P=1.00). No patients required repeated drainage after their drain removed. Patients in experimental group were discharged after a mean of 5.52 days and in control group after a mean of 5.70 days (P=0.335).
Full table
Discussion
After a thoracic surgical procedure, the pleural space often requires chest tube drainage for either air or fluid. However, chest tube management is determined primarily by habit and personal experience rather than a scientifically valid foundation. A large bore (28−32 F) semi-rigid plastic tube is usually used as standard procedure for drainage of the pleural space after lung resection. The chest drainage is aimed at monitoring bleeding, the removal of blood, fluid and air, and to allow the full expansion of the residual lung and to reestablish correct ventilatory mechanics by restoration of negative intrapleural pressure.
However, large bore chest drainages pass through the intercostal spaces, create great discomfort for the patient who often experiences pain; as a result there may be restriction of deep breathing, sputum retention and atelectasis.
Although minimally invasive thoracic surgery (VATS) is claimed to be less painful, the use of a large bore chest tubes greatly reduce the benefits of a less invasive procedure. The main cause of chest pain is due to pleural and intercostal nerves stimulated by the standard drain (a large bore semi-rigid plastic chest tube), especially when patients coughed or performed PO mobilization. As a result patients suffered severe drains-related chest pain and PO exercises were hindered usually.
Thoracic surgeons have made great efforts to improve PO chest pain after thoracic surgery including reducing duration of chest drainage and using small bore tube (3-5). In 2000 two studies have reported using small, flexible, fluted drains after cardiac surgery (6,7). Later in 2005 Terzi and Icard proved spiral drains to be at least as safe and effective as conventional tubes after lung surgery (8,9). But few studies which have dealt with drainage-related pain have analyzed the problem of structure and texture of drain tube, which always affects the sensations of patients and the early PO exercises.
The use of silicone fluted drain tube has been reported after neurosurgery and breast surgery, but using similar drain tubes after thoracic surgery has never been reported. Because of its three longitudinal supporting structures over the entire length, 1 mm height and spaced 1 mm apart characteristically, and silicone materials (Shore A 69I U), silicone fluted drain tube can avoid higher pressure on ribs and provide adequate drainage (Figure 4). And the supporting structure design allows for a total lack of collapsing as contraction of the intercostal muscles due to coughing or deep breathing. All the drainage flows into the longitudinal grooves, then a smooth transition of silicone fluted drain tube can be easily connected to extracorporeal drain tube. In our study, no drain was found obstructed and no patients requires supplement drainage for pneumothorax or pleural effusion. In addition no serious adverse event has been observed, including but not limited to foreign body reaction and allergy. To be adapted to chest drain, silicone fluted drain tubes were modified in some details, including making a few of side apertures (10) and marking the last aperture. Besides, low-dose radiograph should be better avoided for PO assessment, due to absence of radiographic mark line.
Through this prospective, randomized and controlled study, modified silicone fluted drain tube was confirmed as practical as standard drain tube in monitoring of bleeding and the removal of fluids and air for chest drainage. No patients developed drains-related complications such as sepsis, obstruction, pleural effusion or slipping off of drain tube. Moreover application of the modified silicone fluted drain tube was superior in the risk of mild fever (T >37.4 °C) and mild pneumothorax, though the difference was not significant statistically. Importantly, this study shows that the pain intensity is significantly lower in the experimental group, especially at the early stage PO, suggested the ideal rehabilitation.
In conclusion, we suggested that the application of modified silicone fluted drain tube is recommended in thoracic drainage post-VATS lung resection, as a simple and effective way, and importantly it helps to improve the comfort of operated patients, while the modification of drainage policy did not increase procedure and management difficulty.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Scott J, Huskisson EC. Graphic representation of pain. Pain 1976;2:175-84. [PubMed]
- Gagliese L, Weizblit N, Ellis W, et al. The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain 2005;117:412-20. [PubMed]
- Mongardon N, Tremey B, Marty J. Thoracentesis and chest tube management in critical care medicine: a multicenter survey of current practices. Chest 2010;138:1524-5. [PubMed]
- Mueller XM, Tinguely F, Tevaearai HT, et al. Impact of duration of chest tube drainage on pain after cardiac surgery. Eur J Cardiothorac Surg 2000;18:570-4. [PubMed]
- Alex J, Ansari J, Bahalkar P, et al. Comparison of the immediate postoperative outcome of using the conventional two drains versus a single drain after lobectomy. Ann Thorac Surg 2003;76:1046-9. [PubMed]
- Lancey RA, Gaca C, Vander Salm TJ. The use of smaller, more flexible chest drains following open heart surgery: an initial evaluation. Chest 2001;119:19-24. [PubMed]
- Obney JA, Barnes MJ, Lisagor PG, et al. A method for mediastinal drainage after cardiac procedures using small silastic drains. Ann Thorac Surg 2000;70:1109-10. [PubMed]
- Icard P, Chautard J, Zhang X, et al. A single 24F Blake drain after wedge resection or lobectomy: a study on 100 consecutive cases. Eur J Cardiothorac Surg 2006;30:649-51. [PubMed]
- Terzi A, Feil B, Bonadiman C, et al. The use of flexible spiral drains after non-cardiac thoracic surgery. A clinical study. Eur J Cardiothorac Surg 2005;27:134-7. [PubMed]
- Apostolakis EE, Baikoussis NG. Single or double drain after lung resections? Eur J Cardiothorac Surg 2009;36:424; author reply 425. [PubMed]