Breast cancer manifested by hematologic disorders
Abstract
Breast cancer is the most common type of cancer in women. However, it is very rarely manifested as hematologic disorders. A 35-year-old woman was admitted because of disseminated intravascular coagulation. Examinations revealed the presence of breast cancer in her left breast; therefore, paclitaxel was administered weekly. Although disseminated intravascular coagulation was controlled, pulmonary dysfunction due to lymphangitis carcinomatosa suddenly occurred 10 weeks after treatment. Pulmonary dysfunction was effectively treated with epirubicin and cyclophosphamide. Twenty-three weeks after treatment, the patient developed liver dysfunction accompanied with jaundice due to progressive metastatic lesions in the liver; liver dysfunction improved after the administration of vinorelbine. Subsequently, because of the recurrence of pulmonary dysfunction, rechallenge with epirubicin and cyclophosphamide was performed and was effective; however, this therapy was discontinued because of its adverse effects. She expired of liver failure 33 weeks after the occurrence of disseminated intravascular coagulation. Metastatic tumors in the bone marrow, lung, and liver showed different sensitivities to different anti-cancer agents. We report a case of breast cancer manifested by hematologic disorders which was treated by a sequential chemotherapy.
Key words: Breast cancer; disseminated intravascular coagulation; multiple organ metastases
Introduction
Bone marrow metastasis may be a different clinical entity from usual bone metastases. Although it is reported that breast cancer cells were found subclinically in the bone marrow by autopsy (1), cases of breast cancer manifesting as hematologic disorders due to disseminated carcinomatosis in the bone are rare (2-5). The prognosis of these cases is dismal. Cytotoxic anticancer agents are the only effective treatment for improving the life-threatening conditions of hematologic crisis (6), although ineffective agents may be fatal by worsening hematologic disorders.
In this report, we describe a case of breast cancer manifested by disseminated intravascular coagulation (DIC); the patient was treated with several anticancer agents sequentially starting from weekly administration of paclitaxel.
Case report
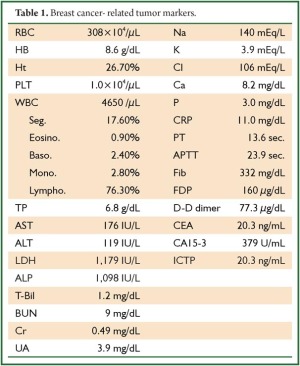
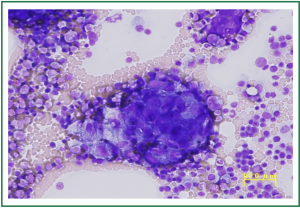
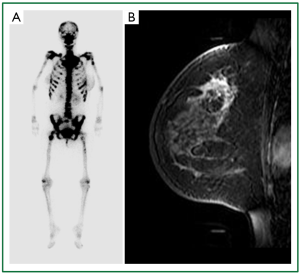
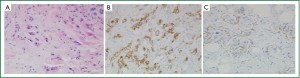
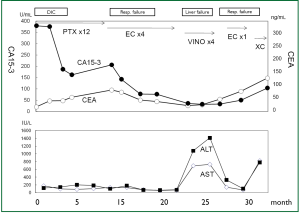
A 35-year-old woman was emergently admitted because of DIC (Table 1). Except for back pain and purpura on the legs, she did not have any physical abnormalities, even on her breasts. Because her condition suggested the presence of hematologic disease, bone marrow aspiration cytology was performed, and a few nests of adenocarcinoma were detected (Figure 1). A bone scintigram showed a so-called “beautiful bone” finding (Figure 2A), suggesting massive involvement of the bone. The elevation of breast cancer-related tumor markers (Table 1) suggested the presence of breast cancer with bone marrow dissemination. Therefore, radiological examinations were performed for detecting breast cancer. Magnetic resonance imaging (MRI) revealed an enhanced area in the upper-outer quadrant of the left breast (Figure 2B), although the findings of mammography and ultrasonography were not definitive. A core needle biopsy was performed on her left breast; examination of the biopsy specimen revealed invasive ductal carcinoma that was estrogen receptor-negative, progesterone receptor-negative, and HER2-negative (Figures 3,4). On the basis of these findings and her hematologic condition, weekly administration of paclitaxel (80 mg/m2) was chosen as the treatment. The clinical course of this case is summarized in Figure 5. Chemotherapy was performed along with treatments for DIC, including platelet transfusion. After 6 cycles of paclitaxel treatment, she recovered from DIC and was discharged from the hospital. The CA15-3 level, which had dramatically decreased after treatment, started to increase again during paclitaxel treatment. After 10 weeks, the patient complained of dyspnea. A chest radiograph revealed that the disease had recurred as lymphangitis carcinomatosa in the lung. Because the hematological conditions had been completely restored, a combined therapy of epirubicin (90 mg/m2) and cyclophosphamide (600 mg/m2) (EC) was administered. EC improved her respiratory function dramatically and was administered for 4 cycles. Twenty-three weeks after treatment, she developed a spike fever and liver dysfunction accompanied with jaundice. Worsening liver metastases were the most likely causes of cholangitis, because computed tomography (CT) revealed the appearance of a mass lesion in the left lobe of the liver. Dissemination in the liver had been suspected because of the constant elevation of transamylases since admission. We decided that EC was effective for the treatment of disease in the lung but not in the liver; therefore, vinorelbine (40 mg/m2) was chosen as the next regimen. Laboratory data showed that the liver function dramatically improved after 4 cycles of treatment. After 27 weeks, the respiratory function worsened again with a recurrence of lymphangitis carcinomatosa. Although rechallenge with EC improved dyspnea, the adverse effects of this treatment, including leukocytopenia, were too severe to continue this regimen. A combination of capecitabine and cyclophosphamide was started as an alternative therapy. Liver dysfunction progressed gradually. The patient died of liver failure after 33 weeks of administration of therapy.
Full table
Discussion
In patients with cancer, the pathogenic mechanism of hematologic disorders such as DIC is not clearly understood. Diffuse bone marrow metastases may cause damage to vascular endothelial cells, excess thromboplastic activity, and the presence of tissue thromboplastin-like substances, resulting in abnormalities of the coagulation-fibrinolytic system (4,5). From the clinical viewpoint, most cases of cancer-associated hematologic disorders have been reported in patients with gastric and breast cancer (5-7). At present, administration of effective anti-cancer drugs is the only treatment for prolonging the survival time (6); however, the diseases are not completely curable.
In the present case, the initial treatment of weekly administration of PAC was effective in treating the bone marrow lesion. Hematologic disorders did not recur during the entire course afterwards. From the clinical viewpoint, we decided that weekly administration of PAC was the best regimen for treating this type of condition. Considering the condition of hematologic crisis, drugs like anthracycline and docetaxel, which are administered at the highest dose at every 3 weeks, were difficult to use in the condition of DIC. If an anticancer drug was not effective in this case, the administration of the drug may have worsened her hematologic condition.
During paclitaxel treatment, the levels of tumor markers were elevated again; this was followed by respiratory and liver dysfunction. EC was effective in the lung but not in the liver, whereas vinorelbine was effective in the liver but not in the lung. Hematologic disorders due to bone marrow dissemination were controlled by all the 3 regimens used. Retrospective examination showed that the efficacies of drugs were different at various metastatic sites. This is partly because the characteristics of cancer cells may change at different metastatic sites. The phenomena of epithelial-mesenchymal interaction and transition suggest that the microenvironment affects the phenotype of cancer cells at each metastatic site (8).
All 3 drugs were temporally effective in preventing the occurrence of critical conditions in the present case. At present, it is almost impossible to cure metastatic diseases. Further, this case was categorized as a case of triple-negative breast cancer, probably of the basal phenotype, for which no specific therapy is available. Recently, however, basic and clinical evidence has shown that novel agents like PARP-1 inhibitor and DNA-damaging agents, i.e., cisplatin, are specifically effective for treating this subtype (9,10). These drugs may have improved survival in our patient. A subtype-oriented strategy will help to overcome the limitations of the present treatment for breast cancer.
This case suggests that a further understanding of biology and a new type of anti-cancer agents are required to prolong the survival of breast cancer cases manifested by hematologic disorders.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Galasko CS. Skeletal metastases. Clin Orthop Relat Res 1986;210:18-30.
- Chang YH, Hsieh RK, Chang MC, et al. Breast cancer with an unusual leukemia-like presentation: case report and literature review. Med Oncol 2008;25:100-3.
- Kressel BR, Ryan KP, Duong AT, et al. Microangiopathic hemolytic anemia, thrombocytopenia, and renal failure in patients treated for adenocarcinoma. Cancer 1981;48:1738-45.
- Chang JC, Naqvi T. Thrombotic thrombocytopenic purpura associated with bone marrow metastasis and secondary myelofibrosis in cancer. Oncologist 2003;8:375-80.
- Sallah S, Wan JY, Nguyen NP, et al. Disseminated intravascular coagulation in solid tumors: clinical and pathologic study. Thromb Haemost 2001;86:828-33.
- von Bubnoff N, Sandherr M, Schneller F, et al. Thrombotic thrombocytopenic purpura in metastatic carcinoma of the breast. Am J Clin Oncol 2000;23:74-7.
- Etoh T, Baba H, Taketomi A, et al. Diffuse bone metastasis with hematologic disorders from gastric cancer: clinicopathological features and prognosis. Oncol Rep 1999;6:601-5.
- Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest 2009;119:1420-8.
- Rottenberg S, Jaspers JE, Kersbergen A, et al. High sensitivity of BRCA1-deficient mammary tumors to the PARP inhibitor AZD2281 alone and in combination with platinum drugs. Proc Natl Acad Sci U S A 2008;105:17079-84.
- O’Shaughnessy J, Osborne C, Pippen J, et al. Efficacy of BSI-201, a poly (ADP-ribose) polymerase-1 (PARP1) inhibitor, in combination with gemcitabine/carboplatin (G/C) in patients with metastatic triple-negative breast cancer (TNBC): Results of a randomized phase II trial. J Clin Oncol 2009;27:18s:abstr 3.


