Non-intubated combined with video-assisted thoracoscopic in carinal reconstruction
Introduction
Carinal reconstruction is a highly challenging surgery for most thoracic surgeons. In the past, it needed to be completed via large incisions or even under extracorporeal circulation. Furthermore, postoperative anastomotic leak, anastomotic stricture, and infections can also be problematic. Along with advances in surgical techniques and equipment, complete video-assisted thoracoscopic surgery (VATS) carinal reconstruction has become possible. In particular, the presence of tracheal tube during anastomosis results in poor surgical field and high anastomotic tension, which directly increases the surgical difficulty and prolong the operative time. Thus, in this article we describe the application of a novel non-intubated complete VATS carinal reconstruction surgery.
Case presentation
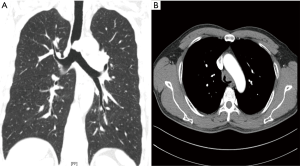
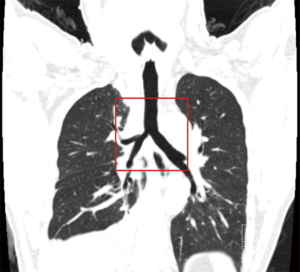
A 45-year-old male patient was admitted due to recent chest tightness and pain. He had been diagnosed with adenoid cystic carcinoma (ACC) of the trachea by branchofiberoscopy one year before. Chest computed tomography (CT) showed a nodule measuring about 1.7 cm × 1.4 cm located on the left wall of the lower trachea, 1 cm away from the carina. Biopsy of the tracheal mucosa 1 cm away from the upper edge of the mass showed no definite tumor cell infiltration (Figure 1). Preoperative pulmonary function tests prompted that the patient had extremely severe obstructive ventilation dysfunction, with an FEV1 of 0.76 L and diffusing capacity of 121%. Distant metastasis was ruled out by preoperative examinations.
The body mass index (BMI) was 24.38 and the American Society of Anesthesiologists (ASA) score was 2. Endotracheal intubation may easily lead to tumor hemorrhage and even suffocation, and endotracheal intubation may also affect the anastomosis procedure; therefore, we decided to carry out non-intubated VATS carinal reconstruction.
Pre-anesthesia preparation included the use of midazolam (0.06 mg/kg) and atropine (0.01 mg/kg) 30 min before surgery; then, thoracic epidural block was performed at T6−7 level using 0.25% ropivacaine. Intravenous anesthesia was performed using remifentanil (0.05 mg/kg/min), dexmedetomidine (0.5–1.0 μg/kg/hr), and propofol (1.5–2.5 ug/mL). The patient had spontaneous breathing. Oxygen was delivered via the laryngeal mask to maintain the blood oxygen concentration above 90%. The electrocardiogram (ECG), blood pressure, blood oxygen, arterial blood gas, and urine volume were closely monitored during the surgery.
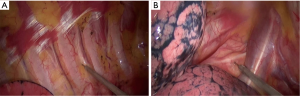
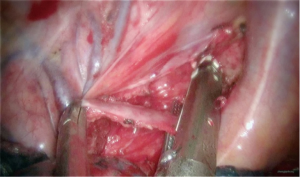
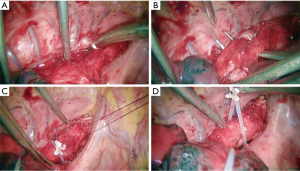
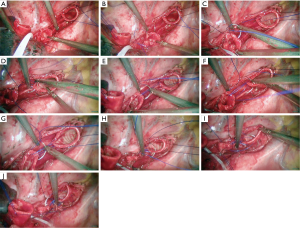
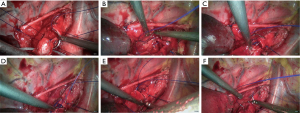
The surgical incisions were selected as follows: (I) observation port: in the 6th intercostal space at anterior axillary line, about 12 mm in length; 30° 3D thoracoscope (Aesculap, Germany) was used; (II) auxiliary operation port: at posterior line, 10 mm in length; and (III) main operation port: in the 4th intercostal space between anterior axillary line and mid-axillary line, about 4 cm in length (Figure 2). Local anesthesia with lidocaine was performed before incision creation. After entering the pleural cavity, we blocked the intercostal nerve and the vagus nerve using 0.25% ropivacaine and 1% lidocaine suspension (Figure 3). The hilar structures were released firstly, during which the Azygos vein was transected (Figure 4), the paratracheal and subcarinal lymph nodes were dissected, and the connective tissues at the lower trachea and around the left and right main bronchus were dissociated (Figure 5). During the surgery, the blood supply of the trachea should be carefully protected and any injury to the vagus nerve should be avoided. Before opening the airway, the surgical field must be kept clean. The right main bronchus was transected at the site near the carina, whereas the left main bronchus was transected at the site 1 cm away from the carina (Figure 6). The site of trachea transection was 1 cm above the tumor (Figures 7,8). Intraoperative frozen-section histopathology was performed to ensure that there was no tumor cell infiltration at the stumps.

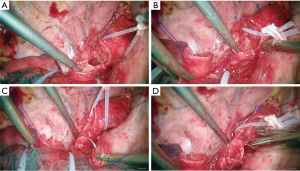
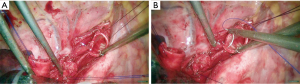
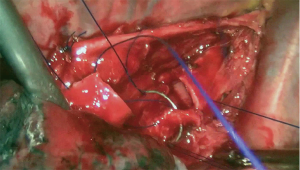
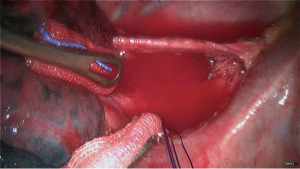
During the carinal reconstruction, the lower segment of trachea and the posterior wall of left main bronchus were continuously anastomozed using 2–0 Prolene sutures (Figure 9), followed by the anastomosis of the anterior wall, during which a 1.2-cm orifice was remained (Figure 10). Then, the right main bronchus and the orifice were continuously anastomozed using 2–0 Prolene sutures (Figures 11,12). Since there was no tracheal tube, the surgical field was clearly exposed, making the anastomosis less difficult. The whole anastomosis process lasted 36 min. An air-leak test using normal saline proved the integrity of the anastomosis (Figure 13). The intraoperative blood loss was about 80 mL. Two chest tubes (#22 and #30, respectively) were placed on the right-upper and lower pleural cavity after the surgery. The forward head posture was maintained after surgery, with the jaw being fixed with the breast skin using two stitches. A second chest CT on the 12th postoperative day showed that the anastomosis was patent (Figure 14). Then, the cervical sutures were removed, and the patient was discharged. Postoperative pathology showed that the tumor had invaded the whole tracheal wall, while no metastasis in mediastinal or hilar lymph node was seen. Under non-intubated anesthesia with spontaneous breathing, VATS carinal reconstruction was successfully performed on August 27th 2015 (Figure 15).
Discussion
In 1957, Mathey et al. first described the carinal reconstruction surgery (2). Since then, surgical treatment of lesion at this site has increasingly been reported in literature. However, this technique is highly challenging and risky and requires the close cooperation from experienced anesthesiologists; therefore, it has not been widely applied in clinical settings. However, in some large medical centers, complete VATS carinal reconstruction has become possible (3). Tracheal intubation on an operating table is an idea method to avoid hypercapnia and hypoxemia throughout the surgery (4). However, both the tracheal intubation via the transglottis that is performed at the beginning and the intubation of the contralateral bronchus via incision on the operating table will influence the surgical operation and result in inadequate surgical exposure. In addition, endotracheal intubation on the operating table also increases the difficulty of surgical anastomosis.
In our center, awake surgeries have been carried out in more than 1,000 cases, with their feasibility and safety well explored (5). Since the awake technique was reported by Pompeo et al. (6) in 2004, it has increasingly been applied in routine thoracic surgeries including lung wedge resection, resection of bullae, and pulmonary lobectomy (7,8). During the carinal reconstruction, exposure and anastomosis of the stumps are the most important steps (9,10). In the past, the tracheal tube needs to be delivered to the contralateral bronchus to ensure ventilation during the endotracheal intubation, resulting in poor exposure of surgical field during the anastomosis between the contralateral bronchus and tracheal end; in addition, the presence of tracheal tube also increases the anastomotic tension, making the surgery even more difficult.
Then, how about the surgery performed in non-intubated patients? In our current case, after the trachea was cut open and the mass was harvested, high-flow air was delivered via the laryngeal mask to ensure a high oxygen concentration in the pleural cavity. The patient’s own physical needs drive the intercostal muscles and diaphragm to move, enabling the high-concentration oxygen to effectively enter the bilateral main bronchi for oxygenation, followed by the discharge of carbon dioxide. If the blood oxygen decreases during the surgery, the oxygen supply from the ventilator may be increased; if necessary, a thin tube may be inserted into the left main bronchus on the operating table to achieve high-frequency ventilation. However, this procedure was not needed in our current case. Notably, since the blood and secretions can not be suctioned in an awake patient, the operator must carry out adequate hemostasis before anastomosis, so as to ensure the cleanness of the surgical field. Bronchial suspension is another key step to reduce blood inflow.
Appropriate patient selection, improved anesthesia management, and more sophisticated surgical techniques are key factors in ensuring the success of carinal reconstruction and reducing postoperative complications and deaths (11). It is also urgently needed to make the surgical operations simpler and safer. Non-intubated anesthesia enables the clearer exposure of stumps and thus dramatically facilitates the surgical anastomosis for most thoracic surgeons. It is a feasible and safe surgical anesthesia mode for selected patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Peng G, Cui F, He J, et al. Non-intubated combined with video-assisted thoracoscopic in carinal reconstruction. Asvide 2016;3:156. Available online: http://www.asvide.com/articles/911
- Mathey J, Binet JP, Galey JJ, et al. Tracheal and tracheobronchial resections; technique and results in 20 cases. J Thorac Cardiovasc Surg 1966;51:1-13. [PubMed]
- Xu X, Chen H, Yin W, et al. Thoracoscopic half carina resection and bronchial sleeve resection for central lung cancer. Surg Innov 2014;21:481-6. [Crossref] [PubMed]
- Blasberg JD, Wright CD. Surgical considerations in tracheal and carinal resection. Semin Cardiothorac Vasc Anesth 2012;16:190-5. [Crossref] [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]
- Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. [Crossref] [PubMed]
- Kiss G, Castillo M. Non-intubated anesthesia in thoracic surgery-technical issues. Ann Transl Med 2015;3:109. [PubMed]
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Jiang F, Xu L, Yuan F, et al. Carinal resection and reconstruction in surgical treatment of bronchogenic carcinoma with carinal involvement. J Thorac Oncol 2009;4:1375-9. [Crossref] [PubMed]
- Xu Q, Deng Y, Fu S, et al. A novel tracheobronchial reconstruction for right upper lung carcinoma involving the lower trachea: preliminary results. Ann Thorac Surg 2012;93:1070-4. [Crossref] [PubMed]
- Weder W, Inci I. Carinal resection and sleeve pneumonectomy. Thorac Surg Clin 2014;24:77-83. [Crossref] [PubMed]