Operative endoscopy of the airway
Introduction
Since its first description in 1897 (1), when Gustav Killian bronchoscopically extracted a piece of bone from the airway of a patient, bronchoscopy has undergone extensive evolution and currently resides as one of the thoracic surgeons’ most important and useful tools. Endoscopy of the airway affords the surgeon multiple diagnostic and therapeutic options for a variety of disease states. This review describes the various current uses, equipment, and technical considerations for surgical airway endoscopy.
Equipment
The most fundamental instruments needed for airway endoscopy are a bronchoscope and a light source. Both rigid and flexible bronchoscopes are widely available for use by the thoracic surgeon. Each has distinct advantages and disadvantages and the preferred approach is generally dictated by the procedural goals, but often both techniques are used in conjunction. It is therefore imperative that the thoracic surgeon develops a level of comfort with both flexible and rigid bronchoscopic methods to achieve optimal outcomes.
Flexible bronchoscopy is performed using a small caliber endoscope, which can be inserted nasally or orally, in the awake or anesthetized patient. The flexible bronchoscope offers excellent visualization of the proximal and distal airways and contains a working port, which can accommodate a variety of instruments that can be used for diagnostic and therapeutic purposes. Flexible bronchoscopy is generally well tolerated, which makes it useful when multiple repeated interventions are required. The learning curve for flexible bronchoscopy is fairly shallow and, therefore, many practitioners easily develop a level of comfort with its use.
Rigid bronchoscopy, in contrast, is more technically demanding to master, but affords the bronchoscopist many more diagnostic and therapeutic options. However, it does require an anesthetized patient and demands experience with airway intubation, as insertion of the rigid bronchoscope may be technically challenging when anatomical challenges exist. Therefore, preoperative assessment is important. History should include inquiry regarding neck and cervical spine issues, and physical examination should assess for neck mobility, body habitus, and airway quality.
Anesthesia
Communication between the anesthesia and surgical teams is absolutely critical when undertaking any airway procedure; there is probably no other surgical procedure that requires more coordination of anesthesiologist and surgeon than co-management of a threatened airway. Prior to induction of anesthesia, it is important to conduct a preoperative “timeout” with the surgical, anesthesia, and nursing teams to discuss the operative plan, specific patient anatomy, and ensure all necessary equipment are available and operational. The surgeon is at the bedside when the patient is induced and is prepared to establish emergent airway access with a rigid bronchoscope if necessary, as deep anesthesia may lead to loss of a patent airway. This is particularly important in the case of any obstructive airway lesion.
When rigid bronchoscopy is indicated, a totally intravenous general anesthesia is preferred with deferral of paralysis until the surgeon and anesthesiologist are mutually in agreement that a stable airway is achieved or achievable. There are a variety of ventilatory approaches that have been well described, including spontaneous assisted ventilation (2), jet ventilation (3), apneic ventilation (4), and closed system ventilation. In most cases the simplest and most reliable is standard closed system ventilation, treating the rigid bronchoscope as an endotracheal tube, with pauses in ventilation when the bronchoscope is opened for suctioning, biopsy, or stent placement. Although jet ventilation is popular, it is an unnecessary encumbrance to the procedure and adds noise and aerosolized blood and secretions that are annoying to the operator and team. Limiting the fraction of delivered oxygen to less than 50% is often necessary, particularly when utilizing the neodymium-doped yttrium aluminium garnet (Nd:YAG) laser or electrocautery to prevent combustion.
Procedural basics
Insertion of the flexible bronchoscope is rarely demanding and can be accomplished via nasal and oral routes. Local anesthesia is paramount and there are a variety of approaches to achieve an adequate level of patient tolerance. When using a trans-nasal approach in an awake patient, it is useful to anesthetize the nasal passages with topical lidocaine jelly or 10% liquid cocaine, which mitigates much of the discomfort attributed to insertion of the bronchoscope. Aerosolized 4% lidocaine can be administered transorally with an atomizer. After insertion of the bronchoscope, the vocal cords are observed and anesthetized under direct visualization with topical injectable lidocaine. Depending on level of stimulation and patient tolerance, it is often useful to anesthetize the carina and distal airways as well to avoid coughing during the procedure.
The rigid bronchoscope is significantly more challenging to insert, but having a comfort with endotracheal intubation, a reliable plan, and an understanding of alternate methods will lead to a high degree of success. There are several described methods for rigid scope insertion, including use of a laryngoscope to directly visualize the vocal cords, or following the pathway of the endotracheal tube in an already intubated patient. The most straightforward technique is to directly intubate the trachea using the rigid bronchoscope, using the scope to identify the vocal cords, and directly pass through them in order to establish a bronchoscopically controlled airway. Positioning of the patient varies depending on several patient factors (e.g., age, obesity, anatomy), and either flexion or extension of the neck may be beneficial in different circumstances. In general, the best position for the initial intubation is similar to that used by the anesthesiologists for intubation, i.e. the neck flexed and chin pulled back, the so-called “sniffing position”. Once intubated however, it is often easier to access the lower airways with a change of this position into one of neck extension to more easily align the upper and lower airway. For intubation, the endoscopist stands directly above the patient’s head and, after the patient is preoxygenated, a soft guard is placed on the upper teeth. The endotracheal tube or laryngeal mask airway (LMA) is withdrawn and the rigid bronchoscope is inserted orally with the right hand, while the left hand stabilizes the scope and protects against leverage on the teeth at the level of the patient’s mouth. The rigid scope is carefully inserted along the posterior aspect of the tongue, then, gently lifting upward, the epiglottis is brought into view and the scope used to elevate the epiglottis. This allows visualization of the vocal cords, which are intubated after rotating the bronchoscope 90 degrees and inserting the leading beveled edge to limit trauma to the vocal cords. A common error is extending the scope too far under the epiglottis and actually passing the arytenoids, lifting the larynx, and visualizing the esophagus rather than the vocal cords (yet this modification is exactly how to perform rigid esophagoscopy). If insertion is challenging, the patient is re-oxygenated and the oropharynx is suctioned clean before additional attempts at intubation are made. Occasionally repositioning the patient, adding a shoulder roll, or using an alternate method of intubation is necessary.
After successful insertion of the rigid bronchoscope, ventilation is initiated and the airway anatomy is assessed. The next section of this review highlights some of the most common diagnostic and therapeutic uses of airway endoscopy and describes the technical aspects and limitations of these techniques.
Airway obstruction
Stenosis
Often, airway obstruction is an urgent or emergent predicament and requires a thoughtful and sometimes rapid approach to restore airway patency. Emergency surgical management is rarely indicated, as endoscopy is nearly always able to stabilize and temporarily palliate both benign and malignant sources of airway obstruction and can often provide both temporizing and definitive treatment.
Benign stenoses are frequently iatrogenic, occurring after prolonged intubation, tracheostomy, lung transplantation, tracheal resection, and sleeve resection, but can also be caused by extrinsic compression, rare benign tumors, infectious/inflammatory processes, or foreign bodies (Table 1). Malignant stenoses have a variety of etiologies related to primary airway tumors, adjacent cancers invading or compressing the airway, and metastatic disease. Just as there are a variety of etiologies of airway stenoses, there are numerous endoscopic techniques to treat them. To achieve consistent and durable results, it is essential for the thoracic surgeon to be familiar with a full repertoire of techniques, described below.
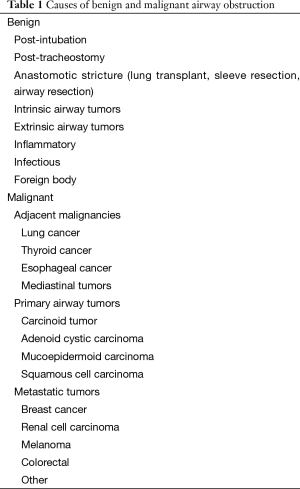
Full table
Balloon dilation was first described in 1984 (5) and has evolved into a highly useful technique for relief of benign, and some malignant, airway stenoses. The significant advantages of balloon catheter dilation are the deliverability through the flexible bronchoscope, ease of use, control of the dilation diameter, and the ability to perform as an outpatient procedure. The major limitation is durability, which is variable, and often necessitates frequent repeat dilations. Fortunately, repeated balloon dilation, particularly using flexible bronchoscopy, is well tolerated and, depending on the underlying etiology, can occasionally achieve prolonged period of airway patency. Dilation is safe and severe complications are extremely rare, but overdilation may cause airway laceration and hemorrhage and in some cases airway rupture or even pulmonary artery injury (6-8). Success of balloon dilation is most often seen in patients with short-segment fibrotic stenoses and in these patients, immediate relief of symptoms is observed while the patient is in the post-anesthesia care unit. While dilation has been described in non-anesthetized patients, the use of general anesthesia reduces pain and allows easy transition to other techniques if necessary. Patients with idiopathic laryngotracheal stenosis often can have prolonged periods of palliation (12–24 months) that avoids or delays the need for surgical reconstruction. However, post-intubation stenoses are usually palliated only briefly (days to weeks) and dilation simply serves for airway stabilization and semi-elective planning for tracheal resection and reconstruction. Paradoxically, post-tracheostomy stomal stenoses rarely benefit from dilatation, usually because the membranous wall is uninvolved and highly compliant, meaning that the dilatation only expands the normal membranous wall that recoils back to its normal position as soon as the dilation is completed. Finally, extrinsic airway compression is rarely improved by dilatation alone, usually requiring endoluminal stenting to establish stable palliation.
The incidence of bronchial stenosis after lung transplantation has been reported to be approximately 8% (9,10). Often this is discovered in the first couple months after transplantation. For patients who develop early anastomotic stricture after lung transplantation, the timing of therapeutic intervention is important. It is preferable to delay intervention until 6 weeks after the initial operation, if possible, to allow for anastomotic maturity and integrity. Treatment often requires debridement of granulation tissue combined with balloon dilation, which often needs to be repeated at 1–4 weeks intervals depending on the severity of the obstruction and the patient’s symptoms. Stenting may also be appropriate in some patients (described in more detail below). Similar principles apply to other airway anastomotic strictures, e.g., those after tracheal resection or sleeve lobectomy. However, individualization is important to assure a stable airway and distal airway continuity.
Endobronchial tumors
Endobronchial tumors are uncommon, but when they occur they are a common cause of airway obstruction. Pathologies include primary airway tumors, such as adenoid cystic carcinoma and squamous cell carcinoma in the trachea and carina, or carcinoid tumors in central airways below the carina. Mechanical tumor core out is useful for initial management of both benign and malignant tumors, particularly in patients who are not candidates for surgical resection, or those who present with a threatened airway or post-obstructive symptoms that need management prior to definitive resection. For example, core-out of an endoluminal tumor is a valuable strategy for patients with obstruction resulting from carcinoid tumors, which allows for both a definitive biopsy, as well as clearance of obstructive pneumonitis along with better definition of tumor margins prior to a possible sleeve resection. Core out may be accomplished using either flexible or rigid bronchoscopic techniques. However, rigid bronchoscopy is significantly superior to flexible techniques because of its simplicity, speed, versatility and the surgeon’s ability to apply a variety of techniques via the rigid bronchoscope in order to restore airway patency. In addition, should bleeding arise during the core out procedure, the rigid bronchoscope is a much more effective means to aspirate blood and obtain hemostasis. The rigid scope can readily compress bleeding mucosa, allows for delivery of larger caliber suction devices to improve visualization, and use of other modalities to achieve hemostasis.
The method most useful for tumor core out begins with insertion of the rigid bronchoscope and complete visualization the tumor, its pedicle, and the distal airway to delineate the full extent of tumor involvement. The tumor pedicle is then engaged with the tip of the rigid endoscope, which frequently easily dislodges the tumor, and the tumor fragment is removed and debridement completed with biopsy forceps. If bleeding occurs, it generally stops spontaneously, but on occasion compression using the scope or application of topical dilute epinephrine may be a useful adjunct. In rare cases of more severe hemorrhage, electrocautery or Nd:YAG laser application may be an effective means of hemostasis. Historically, it was considered a contraindication to endoscopically biopsy carcinoids and other well-vascularized tumors for fear of massive hemorrhage, but this has been disproven and even well vascularized tumors such as renal cell carcinomas can be safely cored out.
Adjunct techniques for airway obstruction
Laser
The Nd:YAG laser is a useful tool for select cases of airway obstruction. Laser vaporization is a helpful adjunct to mechanical core-out in cases of incomplete tumor debridement, when the location of the tumor is more distal or inaccessible, and also in cases of airway granulations. We employ the Nd:YAG laser with a power setting of 35 watts and a 0.5-s pulse duration for this purpose. As mentioned, the Nd:YAG laser can be useful to control bleeding after biopsy or tumor removal, but is rarely needed for this purpose.
Stenting
Stenting is a useful adjunct to many of the above techniques and in many cases achieves durable results, but stent complications are frequent. Frequently, airway stenting is performed because of surgical ineligibility due to inadequate physiological reserve in patients that might otherwise be candidates for resection. Airway stenting is nearly always combined with other bronchoscopic modalities for treating the endoluminal lesion, which can include (I) core out and mechanical debridement; (II) airway dilation; (III) resection with different energy sources or cryotherapy; and (IV) endoluminal brachytherapy or photodynamic therapy. Stenting should be considered when there is persistent symptomatic airway narrowing after other interventions such as core-out or dilatation, typically when the diameter of an affected airway remains <50% of normal diameter. Stenting is usually the only endoluminal option for patients with extrinsic airway compression, long-segment inflammatory stenosis, or residual obstruction from endoluminal tumor.
Stenting of airway lesions requires a thorough understanding of the various advantages and disadvantages of the available airway endoprostheses. The ideal endoprosthesis is a stent that is (I) easily deployed and adjusted but does not readily migrate; (II) resists compressive forces yet does not erode or breach the native airway mucosa; (III) conforms to the airway contour without kinking or bending; (IV) elicits minimal foreign body reaction and prevents tissue ingrowth or granulation; and (V) allows mucociliary clearance to decrease mucous impaction. Unfortunately, the ideal airway endoprosthesis is not presently available. Current airway stents have some of these properties, but none have all.
There are basically two main categories of airway stents: solid silicone and expandable, and selections from both categories should be readily available for deployment in any given clinical scenario. The main advantages of silicone stents are that they are inexpensive to manufacture; once positioned they are easy to adjust and remove; and relatively well tolerated with minimal reactivity for granulation formation. These stents come in a variety of different diameters and lengths. The disadvantages of silicone stents are that they are stiff and more difficult to deploy, requiring general anesthesia, intubation, and skill with rigid bronchoscopy. However, a considerable amount of sheer force may be required to push the stent across a tight stenosis or stricture, which can traumatize the airway. There are times that silicone stents may not generate sufficient radial force for some strictures or extrinsic compression from tumor. They also do not seat well in malacic segments or conform to longer tortuous stenotic segments, and thus will commonly migrate from position causing itself airway obstruction. It is important to be aware that silicone stents can ignite with laser treatment, which often is used to treat airway granulation.
Expandable bare metal airway stents have a more favorable inner luminal to outer luminal diameter ratio than silicone stents, and are easier to deliver, using flexible bronchoscopy with or without fluoroscopy under topical or general anesthesia. Once delivered, these stents are extremely stable and there is low likelihood of dislodgment or migration. Expandable metal stents can generate considerable radial force which may be favored in fibrotic strictures. Uncovered metal stents theoretically allow mucosal neoepithelialization with the reported possibility to resume mucociliary clearance and also allow ventilation of lobar orifices across the open interstices. However, in reality this potential benefit is far overshadowed by tissue ingrowth and granulation through the interstices that frequently occurs due to the foreign body reaction to the stent. This often results in obstruction of the stent itself, yet once embedded in the airway wall the bare metal stents are extremely difficult to remove without causing significant secondary airway damage. Recurrent obstruction from tissue or tumor ingrowth through the metal interstices can require repeated debridement or even repeat stenting within the stent. Expandable stents also can exert considerable radial force, and therefore, may erode through the airway into adjacent structures and risk creating a possible life-threatening bronchovascular fistula. As a result of these known shortcomings and complications, the United States Food and Drug Administration (FDA) issued a warning that bare metal airway stents should be avoided in the management of benign airway stenosis.
The experience of airway interventionalists and the complications of bare expandable metal stents led to the development of 3rd generation covered expandable stents. These are easier to adjust and remove than uncovered stents. The Polyflex® self-expandable stent is composed of a polyester mesh with a silicone coating, while the Aero® stent consists of a metal nitinol framework covered completely with polyurethane.
We have observed a high rate (94%) of symptomatic improvement in patients with the use of stents to treat benign and malignant airway stenoses (11). In our series, 15% of patients required multiple stents for relief of the obstruction and 41% required multiple endoscopic procedures to maintain symptomatic improvement.
Microdebriders, photodynamic therapy, cryotherapy
There are a host of other methods that have been described to relieve airway stenosis, including electrocautery debridement, mechanical endobronchial microdebriders, photodynamic therapy, and cryosurgical techniques. These methods have been described in the literature with variable results. Microdebriders were initially developed for use in otolaryngology, but have recently been applied to obstructing airway tumors. The microdebrider combines a rotating blade with a suction cannula and has proven to be an effective and low-risk means of tumor removal (12,13). Photodynamic therapy relies on the administration of a photosensitizing substance followed by the application of light at a specific wavelength to an endoluminal tumor. The result is tumor destruction and it has been shown to be an effective means of restoring airway patency (14). However, due to the post-procedure edema that develops, it should not be used in patients with high-grade obstruction. In addition, the patient must undergo repeat bronchoscopy in the days following the procedure to remove sloughed off tissue, which may itself lead to airway compromise, and systemic photosensitivity for several weeks is very limiting for patients. Cryoablation involves the use of a cryogen, most commonly nitrous oxide, to cause localized tissue necrosis and has shown to be as effective as other modalities in symptom relief, although durability is marginal (15).
Tracheomalacia
Patients are sometimes referred to thoracic surgeons with a diagnosis of tracheomalacia based on cross-sectional imaging, physical exam findings, or bronchoscopy assessment. However, cross sectional imaging cannot reliably confirm the diagnosis (16). When tracheomalacia is suspected, careful evaluation of the airway using flexible bronchoscopy in the awake, locally anesthetized patient is necessary for diagnosis. This allows for direct, dynamic visualization of the airway. When tracheomalacia is present, the endoscopist will visualize airway collapse generally in the anterior-posterior dimension. Asking the patient to forcibly exhale or cough will often accentuate these findings.
Endoscopic findings often do not support a diagnosis of tracheomalacia, and in these patients, other etiologies are sought for the patient’s symptoms. Normal patients have some degree of antero-posterior collapse during forced expiratory maneuvers, and this is accentuated in patients with the small airway obstruction of asthma or COPD due to the increased expiratory effort and pressure differences in these pathologies. It is important to not over-diagnose tracheomalacia, although distinguishing it as a primary cause or incidental finding associated with dyspnea is often difficult and may warrant an empiric trial of stenting. If the diagnosis is confirmed, the preferred initial treatment is airway stenting. Stent choice depends on the extent of the affected airways. For isolated tracheomalacia, a tubular tracheal stent may be effective. When the tracheomalacia is in the distal trachea or extends beyond the level of the carina, a Y-stent (DynamicTM Y stent, Boston Scientific, Marlborough, MA) should be used. It is important to directly visualize the takeoff of the right upper bronchus and ensure that the stent does not cover this orifice. It is usually necessary to trim the right mainstem portion of the y-stent, on the lateral aspect to maintain patency of the right upper lobe bronchus. Silicone stents have been shown to have excellent short- and even long-term success in treatment of tracheomalacia, although numerous complications such as stent migration, infection, and obstruction have been described (17,18).
Advanced diagnostic techniques
Patients who present with non-small cell lung cancer (NSCLC) and other pulmonary or mediastinal masses often require tissue biopsy for diagnosis and staging. Traditionally, biopsy has frequently been accomplished using image-guided techniques, or in the case of paratracheal masses and lymphadenopathy, via mediastinoscopy. While these techniques are still often utilized and necessary, less invasive endoscopy techniques are evolving.
Endobronchial ultrasound (EBUS)
Early descriptions of EBUS demonstrated promise with this minimally invasive technology (19), but as the technology and equipment have evolved in the last decade, the diagnostic potential has increased dramatically. Perhaps the central advantage of EBUS is that is allows for transbronchial fine needle aspiration of centrally located mediastinal lymph nodes and other masses. As operators have gained experience, the diagnostic accuracy has increased. In patients with mediastinal adenopathy, meta-analysis demonstrates sensitivity and specificity approaching 92% and 100%, respectively (20). When EBUS is used for staging in patients with NSCLC, accuracy remains high, but the negative predictive value is only 89% (21). Therefore, a negative pathologic finding necessitates another biopsy method, most often, mediastinoscopy. When combined with rapid on-site cytopathologic evaluation (ROSE), the diagnostic accuracy is increased (22,23), although ROSE is not available at all centers. EBUS can successfully evaluate lymph node stations 2, 3, 4, 7, 10, and 11 (24,25).
The technical aspects of EBUS are challenging, but the learning curve can be overcome, and EBUS affords the thoracic surgeon a useful and less invasive diagnostic tool when compared to traditional mediastinoscopy. Using the preoperative cross sectional imaging as a reference, the EBUS scope is advanced to the area in question and the lymph node to be biopsied is identified using the displayed ultrasound image. Usually the lymph node(s) is clearly identified on the ultrasound display, but if the image is not clear, color Doppler may be helpful to rule out a vascular structure prior to biopsy. After identification of the target lesion, a 21-guage fine needle aspiration system is advanced through the working port of the EBUS scope. After advancing the needle into the lymph node, the internal wire is withdrawn, suction is applied, and several quick passes are made with the needle through the lymph node. The aspirated material can either be immediately analyzed (ROSE) or examined as a permanent specimen. It is common that EBUS operators examine only radiologically suspicious lymph nodes identified on CT or PET. However, mediastinal lymph node staging requires thorough evaluation of all visible N2 lymph nodes in order to identify possible occult N2 and/or N3 disease. EBUS is an enormous advance in minimally invasive mediastinal staging. However, inadequate sampling and a high false negative rate warrants proceeding to mediastinoscopy in patients with a suspicious or high-risk mediastinum, but a negative EBUS.
Electromagnetic navigational bronchoscopy (ENB)
Bronchoscopy has played a role in the diagnosis of NSCLC and other tumors for many years, however diagnostic methods have been limited to lesions within the observable airways, bronchial brushings and washings, and fluoroscopy guided lung biopsy. EBUS may be a reasonable alternative for proximal tumors, but generally is not helpful for peripheral tumors. The development of ENB has allowed for diagnosis of lesions within the lung periphery that cannot be visualized with standard flexible bronchoscopy, and affords diagnostic accuracy that exceeds that of bronchial washing. Computed tomography (CT) guided fine needle aspiration or core needle biopsy has been the predominant method of biopsy for peripheral lung masses and nodules, with a sensitivity of approximately 90% (26,27). Unfortunately, this high sensitivity is also associated with high rate of pneumothorax (~25%), requiring tube thoracostomy in up to 5% (28,29). The risk is particularly high for patients with emphysema (29). ENB allows for biopsy of peripheral lung lesions with a diagnostic yield approaching 70% (30-32). The diagnostic power is improved when a bronchus sign is present (an observed bronchus leading directly to the lesion) (33) and with the use of ROSE (32). Complications are rare and the rate of pneumothorax is approximately 1–2% (30-32).
ENB, while effective and safe for diagnosis of peripheral lung masses, can be time consuming, as there are multiple phases to the procedure. The planning phase involves uploading a CT scan using the software from the ENB platform and virtually navigating to the lesion to identify the best pathway. With the patient positioned on a location board, the system is calibrated, the operator navigates to the lesion, and samples the lesion using one or more of a variety of instrument options. ENB can also be used to guide pulmonary resection through placement of fiducial markers or injection of blue dye.
Endobronchial valves
Lung volume reduction
The National Emphysema Treatment Trial (NETT) demonstrated the efficacy of lung volume reduction surgery (LVRS) in appropriately selected patients (34). However, in the NETT, mortality was 5.5% and morbidity was high with 59% of patients experiencing a significant complication (35). In an effort to provide similar benefit seen in the NETT with decreased risk and cost, several endobronchial valve systems were developed and designed to function as one-way valves that allow air to escape, but not enter, the airway in which they are placed (36). Early multicenter results demonstrated subjective improvement in symptoms and quality of life with no procedure-related mortality and a low incidence of adverse events (37). Despite this, a randomized, multicenter, double-blinded trial failed to demonstrate a clinically meaningful impact, even though there was a statistically significant improvement for patients who underwent endobronchial valve placement (38). While there is encouragement in the early experience with endobronchial valves as an alternative to LVRS, more studies are needed to gain a better understanding of appropriate patient selection and long-term efficacy.
Management of air leak
Air leaks are a frequently encountered phenomenon for the practicing thoracic surgeon and be a result of spontaneous pneumothorax, or iatrogenic, related to thoracic surgical procedures, pulmonary resection, or lung biopsy. Prolonged air leaks, lasting for more than 5–7 days after secondary spontaneous pneumothorax are not uncommon, particularly in patients with emphysema, 20% of who develop a prolonged leak (39,40). Pulmonary resection is also associated with a high incidence of air leak, with rates of 10% after lobectomy (41) and 45% after LVRS (42). Treatment of prolonged air leak remains a difficult challenge. Perhaps the most common approach is to delay removal of chest tubes until resolution of the air leak. This practice is appropriate for most air leaks, although it is often associated with patient discomfort and may potentially be a source of infection or empyema. Other techniques, such as blood patch, pleurodesis, and operative repair have been describe with varying degrees of success.
Due to the morbidity associated with prolonged air leaks and the lack of effective therapies, bronchoscopic solutions have been attempted. The Watanabe spigot was developed as an early bronchoscopic intervention and was met with some success, with stoppage of 40% of air leaks and reduction in another 38% (43). We and others have had success using endobronchial valves for this purpose (44). The technique involves selective airway occlusion with a balloon catheter while observing the air leak within the chest tube over a period of approximately 1–2 min. It is then possible to deploy and position the endobronchial valve in the affected airway or airways. This technique has been reported with high success rates, including complete or partial resolution in 48% and 45% of patients, respectively, for an overall effectiveness of 93% (45).
Conclusions
Airway endoscopy is an extremely useful tool in the diagnosis and treatment of a variety of thoracic pathologic conditions. Flexible and rigid bronchoscopes are widely available for use, although the rigid bronchoscope affords significantly more interventional opportunities. While mastery of rigid bronchoscopic techniques is challenging, it is a critical skill for practicing thoracic surgeons. Recently, bronchoscopy has continued to evolve into minimally invasive diagnostic and treatment options, such as ENB and endobronchial valves. Airway endoscopy promises to remain at the forefront of thoracic interventions as we continue onto the future.
Acknowledgements
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kollofrath O. Entfernung eines Knochenstücks aus dem rechten Bronchus auf natürlichem Wege und unter Anwendung der directen Laryngoscopie. MMW 1897;38:1038-9.
- Perrin G, Colt HG, Martin C, et al. Safety of interventional rigid bronchoscopy using intravenous anesthesia and spontaneous assisted ventilation. A prospective study. Chest 1992;102:1526-30. [PubMed]
- Sanders RD. Two ventilating attachments for bronchoscopes. Del Med J 1967;39:170-92.
- Frumin MJ, Epstein RM, Cohen G. Apneic oxygenation in man. Anesthesiology 1959;20:789-98. [PubMed]
- Cohen MD, Weber TR, Rao CC. Balloon dilatation of tracheal and bronchial stenosis. AJR Am J Roentgenol 1984;142:477-8. [PubMed]
- Hautmann H, Gamarra F, Pfeifer KJ, et al. Fiberoptic bronchoscopic balloon dilatation in malignant tracheobronchial disease: indications and results. Chest 2001;120:43-9. [PubMed]
- Kim JH, Shin JH, Song HY, et al. Tracheobronchial laceration after balloon dilation for benign strictures: incidence and clinical significance. Chest 2007;131:1114-7. [PubMed]
- Kim JH, Shin JH, Shim TS, et al. Deep tracheal laceration after balloon dilation for benign tracheobronchial stenosis: case reports of two patients. Br J Radiol 2006;79:529-35. [PubMed]
- Fernández-Bussy S, Majid A, Caviedes I, et al. Treatment of airway complications following lung transplantation. Arch Bronconeumol 2011;47:128-33. [PubMed]
- Thistlethwaite PA, Yung G, Kemp A, et al. Airway stenoses after lung transplantation: incidence, management, and outcome. J Thorac Cardiovasc Surg 2008;136:1569-75. [PubMed]
- Wood DE, Liu YH, Vallières E, et al. Airway stenting for malignant and benign tracheobronchial stenosis. Ann Thorac Surg 2003;76:167-72; discussion 173-4. [PubMed]
- Casal RF, Iribarren J, Eapen G, et al. Safety and effectiveness of microdebrider bronchoscopy for the management of central airway obstruction. Respirology 2013;18:1011-5. [PubMed]
- Lunn W, Garland R, Ashiku S, et al. Microdebrider bronchoscopy: a new tool for the interventional bronchoscopist. Ann Thorac Surg 2005;80:1485-8. [PubMed]
- Diaz-Jiménez JP, Martínez-Ballarín JE, Llunell A, et al. Efficacy and safety of photodynamic therapy versus Nd-YAG laser resection in NSCLC with airway obstruction. Eur Respir J 1999;14:800-5. [PubMed]
- Asimakopoulos G, Beeson J, Evans J, et al. Cryosurgery for malignant endobronchial tumors: analysis of outcome. Chest 2005;127:2007-14. [PubMed]
- Boiselle PM, O'Donnell CR, Bankier AA, et al. Tracheal collapsibility in healthy volunteers during forced expiration: assessment with multidetector CT. Radiology 2009;252:255-62. [PubMed]
- Ernst A, Majid A, Feller-Kopman D, et al. Airway stabilization with silicone stents for treating adult tracheobronchomalacia: a prospective observational study. Chest 2007;132:609-16. [PubMed]
- Murgu SD, Colt HG. Complications of silicone stent insertion in patients with expiratory central airway collapse. Ann Thorac Surg 2007;84:1870-7. [PubMed]
- Hürter T, Hanrath P. Endobronchial sonography in the diagnosis of pulmonary and mediastinal tumors. Dtsch Med Wochenschr 1990;115:1899-905. [PubMed]
- Chandra S, Nehra M, Agarwal D, et al. Diagnostic accuracy of endobronchial ultrasound-guided transbronchial needle biopsy in mediastinal lymphadenopathy: a systematic review and meta-analysis. Respir Care 2012;57:384-91. [PubMed]
- Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e142S-65S.
- Trisolini R, Cancellieri A, Tinelli C, et al. Randomized trial of endobronchial ultrasound-guided transbronchial needle aspiration with and without rapid on-site evaluation for lung cancer genotyping. Chest 2015;148:1430-7. [PubMed]
- Yarmus LB, Akulian J, Lechtzin N, et al. Comparison of 21-gauge and 22-gauge aspiration needle in endobronchial ultrasound-guided transbronchial needle aspiration: results of the American College of Chest Physicians Quality Improvement Registry, Education, and Evaluation Registry. Chest 2013;143:1036-43. [PubMed]
- Herth F, Becker HD, Ernst A. Conventional vs endobronchial ultrasound-guided transbronchial needle aspiration: a randomized trial. Chest 2004;125:322-5. [PubMed]
- Yasufuku K, Chiyo M, Koh E, et al. Endobronchial ultrasound guided transbronchial needle aspiration for staging of lung cancer. Lung Cancer 2005;50:347-54. [PubMed]
- Gould MK, Ananth L, Barnett PG, et al. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest 2007;131:383-8. [PubMed]
- Yao X, Gomes MM, Tsao MS, et al. Fine-needle aspiration biopsy versus core-needle biopsy in diagnosing lung cancer: a systematic review. Curr Oncol 2012;19:e16-27. [PubMed]
- Gould MK, Fletcher J, Iannettoni MD, et al. Evaluation of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:108S-130S.
- Laurent F, Michel P, Latrabe V, et al. Pneumothoraces and chest tube placement after CT-guided transthoracic lung biopsy using a coaxial technique: incidence and risk factors. AJR Am J Roentgenol 1999;172:1049-53. [PubMed]
- Eberhardt R, Anantham D, Herth F, et al. Electromagnetic navigation diagnostic bronchoscopy in peripheral lung lesions. Chest 2007;131:1800-5. [PubMed]
- Eberhardt R, Morgan RK, Ernst A, et al. Comparison of suction catheter versus forceps biopsy for sampling of solitary pulmonary nodules guided by electromagnetic navigational bronchoscopy. Respiration 2010;79:54-60. [PubMed]
- Wilson DS, Bartlett RJ. Improved Diagnostic Yield of Bronchoscopy in a Community Practice: Combination of Electromagnetic Navigation System and Rapid On-site Evaluation. J Bronchol 2007;14:227-32.
- Seijo LM, de Torres JP, Lozano MD, et al. Diagnostic yield of electromagnetic navigation bronchoscopy is highly dependent on the presence of a bronchus sign on CT imaging: results from a prospective study. Chest 2010;138:1316-21. [PubMed]
- Fishman A, Martinez F, Naunheim K, et al. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003;348:2059-73. [PubMed]
- Naunheim KS, Wood DE, Krasna MJ, et al. Predictors of operative mortality and cardiopulmonary morbidity in the National Emphysema Treatment Trial. J Thorac Cardiovasc Surg 2006;131:43-53. [PubMed]
- Ingenito EP, Wood DE, Utz JP. Bronchoscopic lung volume reduction in severe emphysema. Proc Am Thorac Soc 2008;5:454-60. [PubMed]
- Wood DE, McKenna RJ Jr, Yusen RD, et al. A multicenter trial of an intrabronchial valve for treatment of severe emphysema. J Thorac Cardiovasc Surg 2007;133:65-73. [PubMed]
- Wood DE, Nader DA, Springmeyer SC, et al. The IBV Valve trial: a multicenter, randomized, double-blind trial of endobronchial therapy for severe emphysema. J Bronchology Interv Pulmonol 2014;21:288-97. [PubMed]
- George RB, Herbert SJ, Shames JM, et al. Pneumothorax complicating pulmonary emphysema. JAMA 1975;234:389-93. [PubMed]
- Videm V, Pillgram-Larsen J, Ellingsen O, et al. Spontaneous pneumothorax in chronic obstructive pulmonary disease: complications, treatment and recurrences. Eur J Respir Dis 1987;71:365-71. [PubMed]
- Stolz AJ, Schützner J, Lischke R, et al. Predictors of prolonged air leak following pulmonary lobectomy. Eur J Cardiothorac Surg 2005;27:334-6. [PubMed]
- Ciccone AM, Meyers BF, Guthrie TJ, et al. Long-term outcome of bilateral lung volume reduction in 250 consecutive patients with emphysema. J Thorac Cardiovasc Surg 2003;125:513-25. [PubMed]
- Watanabe Y, Matsuo K, Tamaoki A, et al. Bronchial occlusion with endobronchial Watanabe spigot. J Bronchol 2003;10:264-67.
- Wood DE, Cerfolio RJ, Gonzalez X, et al. Bronchoscopic management of prolonged air leak. Clin Chest Med 2010;31:127-33. Table of Contents. [PubMed]
- Travaline JM, McKenna RJ Jr, De Giacomo T, et al. Treatment of persistent pulmonary air leaks using endobronchial valves. Chest 2009;136:355-60. [PubMed]


