
Uniportal thoracoscopic pulmonary segmentectomy provides good perioperative results and early postoperative recovery
Introduction
Uniportal video-assisted thoracoscopic surgery (U-VATS) was first introduced and applied to anatomical lung resection 10 years ago (1,2); however, its potential advantages over other VATS techniques remains controversial (3-10). A reduction in the number of wounds may help reduce postoperative pain, as well as offer cosmetic benefits (5,6,9,10), but achieving this requires specialist surgical techniques. Furthermore, recent years have seen an increase in opportunities to perform segmentectomy for early-stage primary lung cancer instead of lobectomy (11-14); therefore, more complicated surgical procedures are now required.
Segmentectomy is usually divided into single and complex segmentectomies, depending on the technical characteristics. Simple segmentectomies are relatively less challenging technically, involving the dissection of only one intersegmental plane containing the superior segment of the lower lobe (S6) and the basilar segment of each side (the left upper division and left lingual segment). Complex segmentectomies can be more challenging to perform as vessels and bronchi must be dissected to the periphery and include several intersegmental planes in three dimensions. Although several reports have described complex segmentectomy to be equally safe as simple segmentectomy (15,16), whether U-VATS complex segmentectomy can also be performed just as safely is unclear.
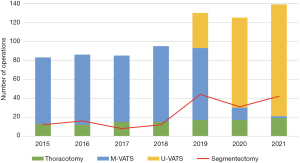
In our previous report in 2021 (17), we established a technique for VATS anatomical lung resection, and U-VATS anatomical lung resection has been performed since February 2019. Since, the number of cases has steadily increased (Figure 1). In this study, we compare the perioperative results from U-VATS segmentectomy performed at our institution with those using the conventional method [hybrid/multiportal VATS (H/M-VATS) segmentectomy], as well as evaluated the safety and usefulness of U-VATS segmentectomy. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-555/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the institutional ethics board of Japanese Red Cross Maebashi Hospital (approval No. 2020-52). The need to obtain individual patient consent for participation in this research was waived due to the retrospective nature of the analysis.
Patient selection
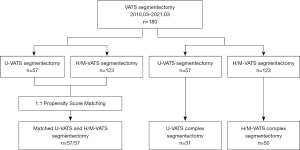
Data from consecutive patients who underwent anatomical pulmonary segmentectomy for lung lesions at our institution between March 2010 and March 2021 were evaluated retrospectively. We divided the patients into the U-VATS and H/M-VATS groups. Perioperative results were compared between these groups after matching for patient background characteristics. Cases of segmentectomy were then selected from each group, and the perioperative results were compared using the same method (Figure 2).
The criteria for selecting patients for segmentectomy at our institution are (I) clinical stage 0–IA1 (Tis-1aN0M0) primary lung cancer confirmed by careful preoperative staging using computed tomography (CT) and/or positron emission tomography/CT (also known as intentional limited surgery); (II) clinical stage IA2–IB (T1b-2aN0M0) primary lung cancer in patients who cannot tolerate radical surgery due to complications and/or poor pulmonary function (passive limited surgery); and (III) metastatic or benign lung tumors for which a sufficient margin was difficult to secure during wedge resection due to the tumor location and size.
Surgical procedures
All surgeries were performed under general anesthesia with the patient in the lateral decubitus position and under differential lung ventilation. Automatic staplers were usually used for vessel and bronchial transections, but suture ligation using 3-0 silk was performed depending on the vessel diameter or the angle of stapler insertion. For segment identification, an inflation-deflation technique or jet ventilation technique was used initially. However, after May 2020, this was replaced by intravenous administration of indocyanine green and a near infrared light thoracoscope. The intersegmental plane was divided using electrocautery or a stapler. Electrocautery was frequently used until 2015 (in almost all hybrid and a portion of multiportal cases), and the decision to use this technique was made by the surgeon. Two-thirds of the outer area in an intersegmental plane was divided by electrocautery, and the remaining deep parenchyma was further divided using staplers. The use of staplers has increased since 2016, including in the uniportal approach, in which staplers are solely used for almost all cases. Intentional limited surgery is often performed for only pure or part-solid ground-glass nodules with a size of the solid part ≤1 cm, and thus it would be uncommon to perform lymphadenectomy in these cases. In almost all cases, hilar lymph nodes were sampled.
H/M-VATS was performed mainly by three senior surgeons, two of whom also perform U-VATS. The overall surgical approach, particularly in terms of multiportal VATS (M-VATS) vs. U-VATS, was decided by each individual surgeon.
U-VATS procedure
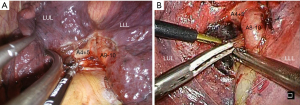
U-VATS for anatomical lung resection was first used in February 2019. Details of the U-VATS procedure have been described previously (17). Briefly, the operator must stand on the ventral side of the patient with an assistant on the dorsal side. A 3.5–4.0 cm skin incision is created in the fourth or fifth intercostal space in the anterior axillary line, and an XS Alexis wound retractor (Applied Medical, Rancho Santa Margarita, CA, USA) is fitted. A 10 mm 30° thoracoscope is then fixed on the dorsal side of the wound margin, securing a space on the ventral side for the surgeon to operate using surgical instruments (Figure 3A). The chest drain is placed on the ventral side of the wound.
H/M-VATS procedure
At our institution, hybrid VATS was performed from 2010 to 2012. In this procedure, an 8.0 cm skin incision is created within the fourth or fifth intercostal space along the mid-axillary line, and the surgeon is positioned directly from the wound. A 10-mm-diameter flexible camera is inserted through a 1.5 cm skin incision in the anterior axillary line of the sixth intercostal space. A thoracic drain is placed through a port in the sixth intercostal space along the anterior axillary line.
At this institution, M-VATS for anatomical lung resection was first performed during 2012. A 2.0 cm skin incision is created in the fourth intercostal space along the anterior axillary line and a 1.5 cm skin incision in the sixth intercostal space along the anterior axillary line, and an XXS Alexis wound retractor is fixed for each wound. A 10 mm flexible camera is inserted via the 1.5 cm skin incision in the sixth intercostal space on the anterior axillary line. When four ports are used, an additional 15 mm skin incision is made in the seventh intercostal space below the scapula for use as the assistant’s port (Figure 3B). The chest drain is placed via the port in the sixth intercostal space along the anterior axillary line.
Postoperative management
The chest drainage tube was removed after confirming both the absence of air leakage and a discharge volume of less than 300 mL. Postoperative complications were evaluated using the Common Terminology Criteria for Adverse Events (version 5.0). Major complications were defined as a requirement for additional treatment. After discharge, patients were followed up in the outpatient clinic on postoperative day 7, then again at 1 month, 3 months, and every 6 months thereafter.
Statistical analysis
Propensity score matching was performed between the U-VATS and H/M-VATS groups to minimize bias. We performed a one-to-one matching analysis between U-VATS and H/M VATS groups on the basis of estimated propensity scores of each patient. Application of propensity score matching involves estimation of the propensity score followed by matching of patients according to their estimated propensity score and comparison of outcomes in matched patients. Propensity scores were calculated using a logistic regression model that included the following variables: age, sex, disease, tumor location, and type of segmentectomy (simple or complicated).
Fisher’s exact test was applied to compare categorical variables. Student’s t-test and the Mann-Whitney U test were used to compare continuous variables. Values of P<0.05 were considered statistically significant.
All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, EZR is a modified version of R Commander designed to add statistical functions frequently used in biostatistics.
Results
A total of 180 patients underwent pulmonary segmentectomy during the study period at this institution, comprising 57 cases in the U-VATS group and 123 cases in the H/M-VATS group (Figure 2). The characteristics of all patients (95 males, 52.8%; 85 females, 47.2%; mean age, 69.1 years; range, 29–84 years) are shown in Table 1. There were 110 cases of primary lung cancer, consisting of 62 and 48 cases that received intentional and passive limited surgery, respectively. Before matching, there were slightly more patients with primary lung cancer in the U-VATS group than H/M-VATS group (P=0.014). After matching for age, sex, disease, tumor location and segmentectomy subtype, the two groups were compared (Table 1).
Table 1
| Variables | All (n=180) | Before matching | After matching | |||||
|---|---|---|---|---|---|---|---|---|
| U-VATS (n=57) | H/M-VATS (n=123) | P | U-VATS (n=57) | H/M-VATS (n=57) | P | |||
| Age | 69.1±13 | 70.2±11 | 68.6±13 | 0.427 | 70.2±11 | 70.9±14 | 0.778 | |
| Sex, male | 95 (52.8) | 30 (52.6) | 65 (52.8) | 1.000 | 30 (52.6) | 33 (57.9) | 0.707 | |
| Disease | 0.014 | 0.163 | ||||||
| Primary lung cancer | 110 (61.1) | 42 (73.7) | 68 (55.3) | 42 (73.7) | 49 (86.0) | |||
| Metastatic tumor | 33 (18.3) | 4 (7.0) | 29 (23.6) | 4 (7.0) | 4 (7.0) | |||
| Others | 37 (20.6) | 11 (19.3) | 26 (21.1) | 11 (19.3) | 4 (7.0) | |||
| Tumor location | 0.169 | 0.948 | ||||||
| Right upper lobe | 38 (21.1) | 17 (29.8) | 21 (17.1) | 17 (29.8) | 15 (26.3) | |||
| Right lower lobe | 53 (29.4) | 18 (31.6) | 35 (28.5) | 18 (31.6) | 17 (29.8) | |||
| Left upper lobe | 62 (34.4) | 15 (26.3) | 47 (38.2) | 15 (26.3) | 18 (31.6) | |||
| Left lower lobe | 27 (15.0) | 7 (12.3) | 20 (16.3) | 7 (12.3) | 7 (12.3) | |||
| Kinds of segmentectomy | 0.107 | 1.000 | ||||||
| Simple | – | 26 (45.6) | 73 (59.3) | 26 (45.6) | 27 (47.4) | |||
| Complex | – | 31 (54.4) | 50 (40.7) | 31 (54.4) | 30 (52.6) | |||
Data are shown as number (%) or mean ± standard deviation. VATS, video-assisted thoracoscopic surgery; U-VATS, uniportal VATS; H/M-VATS, hybrid/multiportal-VATS.
Comparison of perioperative outcomes between the U-VATS and H/M-VATS groups after matching
A comparison of the perioperative outcomes between the U-VATS and H/M VATS groups after matching are shown in Table 2. The operation time was significantly shorter in the U-VATS group than H/M VATS group (141±46 vs. 174±45 min, P<0.001). The postoperative drainage duration (1.5±1.2 vs. 2.3±1.8 days, P=0.007) and postoperative hospital stay (3.4±2.0 vs. 4.6±2.5 days, P=0.006) were also significantly shorter in the U-VATS group. There were no significant differences in the rates of blood loss, major intraoperative bleeding, conversion to thoracotomy, postoperative complications, or re-hospitalization within 30 days after discharge.
Table 2
| Variables | U-VATS (n=57) | H/M-VATS (n=57) | P |
|---|---|---|---|
| Operative time (min) | 141±46 | 174±45 | <0.001 |
| Blood loss (mL) | 41±83 | 28±45 | 0.288 |
| Intraoperative significant bleeding | 4 (7.0) | 6 (10.5) | 0.742 |
| Conversation to thoracotomy | 3 (5.3) | 1 (1.8) | 0.618 |
| Postoperative drainage (days) | 1.5±1.2 | 2.3±1.8 | 0.007 |
| Postoperative hospital stay (days) | 3.4±2.0 | 4.6±2.5 | 0.006 |
| Postoperative complications | 5 (8.8) | 3 (5.3) | 0.716 |
| Re-hospitalization within 30 days of discharge | 1 (1.8) | 1 (1.8) | 1.000 |
Data are shown as mean ± standard deviation or number (%). VATS, video-assisted thoracoscopic surgery; U-VATS, uniportal VATS; H/M-VATS, hybrid/multiportal-VATS.
Postoperative complications occurred in five patients (8.8%) within the U-VATS group and three patients (5.3%) within the H/M-VATS group, including atrial fibrillation in one patient, prolonged air leakage in three patients, delayed pneumothorax in two patients, and hypoxemia in two patients.
Comparison of perioperative outcomes between U-VATS and H/M-VATS complex segmentectomies
The sites of the resected complex segmentectomies in each group are shown in Table 3. There was no significant difference in the resected segment site between the groups. The perioperative outcomes of U-VATS and H/M-VATS complex segmentectomies are compared in Table 4. The operation time was significantly shorter in the U-VATS group than H/M-VATS group (146±34 vs. 185±47 min, P<0.001). The duration of postoperative drainage (1.5±1.3 vs. 2.2±1.2 days, P=0.021) and postoperative hospital stay (3.0±1.4 vs. 4.9±2.1 days, P<0.001) were also significantly shorter in the U-VATS group. There were no significant differences in the rates of blood loss, major intraoperative bleeding, rate of conversion to thoracotomy, postoperative complications, or re-hospitalization within 30 days after discharge.
Table 3
| Variables | U-VATS (n=31) | H/M-VATS (n=50) | P |
|---|---|---|---|
| Locations | 0.660 | ||
| Left side, n (%) | 7 (22.6) | 18 (36.0) | |
| Upper lobe | 7 (22.6) | 16 (32.0) | |
| S1+2 | 3 (9.7) | 9 (18.0) | |
| S3 | 3 (9.7) | 5 (10.0) | |
| S3+4+5 | 1 (3.2) | 2 (4.0) | |
| Lower lobe | 0 | 2 (4.0) | |
| S8+9 | 0 | 1 (2.0) | |
| S9+10 | 0 | 1 (2.0) | |
| Right side, n (%) | 24 (77.4) | 32 (64.0) | |
| Upper lobe | 16 (51.6) | 21 (42.0) | |
| S1 | 3 (9.7) | 2 (4.0) | |
| S1+3 | 3 (9.7) | 0 | |
| S2 | 6 (19.4) | 8 (16.0) | |
| S3 | 4 (12.9) | 7 (14.0) | |
| Others including subsegment | 0 | 4 (8.0) | |
| Lower lobe | 8 (25.8) | 11 (22.0) | |
| S7+8 | 1 (3.2) | 2 (4.0) | |
| S7+8+9 | 1 (3.2) | 0 | |
| S8 | 1 (3.2) | 0 | |
| S8+9 | 0 | 1 (2.0) | |
| S9+10 | 5 (16.1) | 8 (16.0) |
VATS, video-assisted thoracoscopic surgery; U-VATS, uniportal VATS; H/M-VATS, hybrid/multiportal-VATS.
Table 4
| Variables | U-VATS (n=31) | H/M-VATS (n=50) | P |
|---|---|---|---|
| Operation time (min) | 146±34 | 185±47 | <0.001 |
| Blood loss (mL) | 17±34 | 34±52 | 0.120 |
| Intraoperative significant bleeding | 0 | 4 (8.0) | 0.292 |
| Conversation to thoracotomy | 0 | 2 (4.0) | 0.522 |
| Postoperative drainage (days) | 1.5±1.3 | 2.2±1.2 | 0.021 |
| Postoperative hospital stay (days) | 3.0±1.4 | 4.9±2.1 | <0.001 |
| Postoperative complications | 3 (9.7) | 4 (8.0) | 1.000 |
| Re-hospitalization within 30 days of discharge | 1 (3.2) | 2 (4.0) | 1.000 |
Data are shown as mean ± standard deviation or number (%). VATS, video-assisted thoracoscopic surgery; U-VATS, uniportal VATS; H/M-VATS, hybrid/multiportal-VATS.
Postoperative complications occurred in three patients (9.7%) in the U-VATS group and four patients (8.0%) in the H/M-VATS group and comprised prolonged air leak in four patients, delayed pneumothorax in one patient and hypoxemia in two patients.
Oncological outcomes in primary lung cancer patients
During the observation period, seven patients developed lung cancer recurrence, comprising local recurrence in five patients (staple line recurrence in three patients and ipsilateral intrathoracic lymph nodes metastasis in two patients) and distant metastasis in two patients. All seven patients were in the H/M-VATS group, and only one underwent intentional limited surgery.
Discussion
The recent transition at our institution from hybrid to M-VATS and subsequently to U-VATS has been successful, and U-VATS segmentectomy has been performed without the problems often associated with other VATS procedures, even in cases requiring complex segmentectomy. The postoperative complication rates were quite low, thereby enabling an early recovery.
Several previous reports have indicated reduced invasiveness of pulmonary segmentectomy compared with lobectomy, with equal oncological outcomes (11-14). Therefore, the use of pulmonary segmentectomy for small-sized non-small cell lung cancer is expected to increase. However, the results of a Japanese randomized control trial comparing lobectomy with segmentectomy (JCOG0802/WJOG4607L) (18) are awaiting publication. Since the advantages of pulmonary segmentectomy are now known, this surgical procedure should be performed via not only minithoracotomy or the conventional multiportal approach but also the uniportal approach, which is emerging worldwide. Our results indicate that U-VATS pulmonary segmentectomy is feasible. Moreover, complex segmentectomy, which is considered technically difficult, was also safely performed in this study. Thus, highly experienced surgeons can perform any type of segmentectomy appropriately via the uniportal approach.
The U-VATS group showed superior results to the H/M-VATS group, specifically with regards to operative time. Many previous reports comparing perioperative outcomes between U-VATS and M-VATS revealed that operative time is often faster with U-VATS. It was therefore concluded that U-VATS is a more useful approach than M-VATS, although U-VATS is still considered technically difficult due to interference among instruments and the limited insertion angles caused by inserting all instruments including the thoracoscope from a single small wound (19-22). However, in many of those studies, U-VATS was established after heavy use of thoracotomy or M-VATS. This may cause a bias in the U-VATS results due to a relatively recent learning curve. Our previous study demonstrated the learning curve of thoracoscopic lobectomy for in a single surgeon, and we conclude that implementation of U-VATS dose not negatively affect the learning curve of thoracoscopic lobectomy (23). Nevertheless, it is difficult to empirically determine if U-VATS is superior to M-VATS as a thoracoscopic approach considering that U-VATS was not performed until a later time period. Therefore, we focused on assessing whether U-VATS can be implemented successfully with not only lobectomy but also segmentectomy.
Postoperative drainage duration and postoperative hospital stay were both significantly shorter in the U-VATS group. This is likely because postoperative management has been more aggressive in recent years. For example, earlier removal of the drainage tube and shorter hospital stay are now recommended. Early removal of the chest drainage tube after lung resection has been reported to reduce postoperative pain and improve respiratory function, and is thought to help improve respiratory status and prevent complications (24,25). Therefore, regardless of the thoracotomy type (M-VATS vs. U-VATS), drainage tubes are now removed earlier. Changes in the method of intersegmental division might also have an effect. Electrocautery was often used in the H/M-VATS group, and as reported before (26), this may have affected the difference in drainage duration. Moreover, the enhanced recovery after surgery program (a multidisciplinary clinical care bundle that optimizes pre-, intra-, and postoperative care) was adopted by this institution in 2015, and it may have also contributed to early postoperative recovery and shorter hospitalization. Another important factor is the potential for reduced postoperative pain with U-VATS. As reported previously (27), U-VATS creates only a small wound in the anterior axillary line, which has a relatively wide intercostal space and may therefore produce less pressure on the intercostal nerves, leading to reduce postoperative pain compared with M-VATS, which creates a second wound in the posterior axillary line. Reduced postoperative pain may in turn lead to an earlier recovery and a shortened hospital stay.
There are a few important limitations to this study. First, this was a retrospective, single-center, observational cohort study. Second, since the research period was >10 years, perioperative results were affected by the proficiency of the surgeons and changes in perioperative management, as stated above. Third, after the introduction of U-VATS in 2019, the decision of whether to use U-VATS vs. M-VATS was made by each surgeon for each case, so selection bias may have been present. Finally, due to the short follow-up in the U-VATS group, long-term prognoses could not be examined. In the case of intentional limited surgery for malignant diseases, proving curability is important.
In conclusion, U-VATS segmentectomy appears as safe and feasible as H/M-VATS segmentectomy, even for complex segmentectomy cases. An experienced surgeon can make a smooth transition to U-VATS. A larger number of cases from multiple centers should be examined, with further investigation into long-term prognosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-555/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-555/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-555/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-555/coif). HI serves as an unpaid editorial board member of Journal of Thoracic Disease from August 2020 to July 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Japanese Red Cross Maebashi Hospital (No. 2020-52), The need to obtain individual patient consent for participation in this research was waived due to the retrospective nature of the analysis.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- McElnay PJ, Molyneux M, Krishnadas R, et al. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. Eur J Cardiothorac Surg 2015;47:912-5. [Crossref] [PubMed]
- Perna V, Carvajal AF, Torrecilla JA, et al. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg 2016;50:411-5. [Crossref] [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg 2016;49:i37-41. [PubMed]
- Dai F, Meng S, Mei L, et al. Single-port video-assisted thoracic surgery in the treatment of non-small cell lung cancer: a propensity-matched comparative analysis. J Thorac Dis 2016;8:2872-8. [Crossref] [PubMed]
- Akter F, Routledge T, Toufektzian L, et al. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact Cardiovasc Thorac Surg 2015;20:550-5. [Crossref] [PubMed]
- Al-Ameri M, Sachs E, Sartipy U, et al. Uniportal versus multiportal video-assisted thoracic surgery for lung cancer. J Thorac Dis 2019;11:5152-61. [Crossref] [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Yang X, Li M, Yang X, et al. Uniport versus multiport video-assisted thoracoscopic surgery in the perioperative treatment of patients with T1-3N0M0 non-small cell lung cancer: a systematic review and meta-analysis. J Thorac Dis 2018;10:2186-95. [Crossref] [PubMed]
- Okada M, Koike T, Higashiyama M, et al. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 2006;132:769-75. [Crossref] [PubMed]
- Suzuki K, Koike T, Asakawa T, et al. A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol 2011;6:751-6. [Crossref] [PubMed]
- Tosi D, Nosotti M, Bonitta G, et al. Anatomical segmentectomy versus pulmonary lobectomy for stage I non-small-cell lung cancer: patients selection and outcomes from the European Society of Thoracic Surgeons database analysis. Interact Cardiovasc Thorac Surg 2021;32:546-51. [Crossref] [PubMed]
- Nomori H, Yamazaki I, Machida Y, et al. Lobectomy versus segmentectomy: a propensity score-matched comparison of postoperative complications, pulmonary function and prognosis. Interact Cardiovasc Thorac Surg 2022;34:57-65. [Crossref] [PubMed]
- Handa Y, Tsutani Y, Mimae T, et al. Surgical Outcomes of Complex Versus Simple Segmentectomy for Stage I Non-Small Cell Lung Cancer. Ann Thorac Surg 2019;107:1032-9. [Crossref] [PubMed]
- Okubo Y, Yoshida Y, Yotsukura M, et al. Complex segmentectomy is not a complex procedure relative to simple segmentectomy. Eur J Cardiothorac Surg 2021;61:100-7. [Crossref] [PubMed]
- Matsuura N, Igai H, Ohsawa F, et al. Safety and feasibility of uniportal video-assisted thoracoscopic uncommon segmentectomy. J Thorac Dis 2021;13:3001-9. [Crossref] [PubMed]
- Nakamura K, Saji H, Nakajima R, et al. A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol 2010;40:271-4. [Crossref] [PubMed]
- Hernandez-Arenas LA, Purmessur RD, Gonzalez-Rivas D. Uniportal video-assisted thoracoscopic segmentectomy. J Thorac Dis 2018;10:S1205-14. [Crossref] [PubMed]
- Xie D, Wu J, Hu X, et al. Uniportal versus multiportal video-assisted thoracoscopic surgery does not compromise the outcome of segmentectomy. Eur J Cardiothorac Surg 2021;59:650-7. [Crossref] [PubMed]
- Chen YY, Huang WL, Chang CC, et al. Uniportal versus Multiportal Thoracoscopic Complex Segmentectomy: Propensity Matching Analysis. Ann Thorac Cardiovasc Surg 2021;27:237-43. [Crossref] [PubMed]
- Han KN, Kim HK, Choi YH. Comparison of single port versus multiport thoracoscopic segmentectomy. J Thorac Dis 2016;8:S279-86. [PubMed]
- Igai H, Kamiyoshihara M, Furusawa S, et al. The learning curve of thoracoscopic surgery in a single surgeon and successful implementation of uniportal approach. J Thorac Dis 2021;13:4063-71. [Crossref] [PubMed]
- Refai M, Brunelli A, Salati M, et al. The impact of chest tube removal on pain and pulmonary function after pulmonary resection. Eur J Cardiothorac Surg 2012;41:820-2; discussion 823. [Crossref] [PubMed]
- Shen C, Che G. No drains in thoracic surgery with ERAS program. J Cardiothorac Surg 2020;15:112. [Crossref] [PubMed]
- Yazawa T, Igai H, Numajiri K, et al. Comparison of stapler and electrocautery for division of the intersegmental plane in lung segmentectomy. J Thorac Dis 2021;13:6331-42. [Crossref] [PubMed]
- Matsuura N, Igai H, Ohsawa F, et al. Uniport vs. multiport video-assisted thoracoscopic surgery for anatomical lung resection-which is less invasive? J Thorac Dis 2021;13:244-51. [Crossref] [PubMed]


