Resection of the sidewall of superior vena cava using video-assisted thoracic surgery mechanical suture technique
Introduction
Lung cancer invading the superior vena cava (SVC) is a locally advanced condition, for which poor prognosis is expected with conservative treatment alone. Surgical resection of the lesion can rapidly relieve the symptoms and significantly improve survival for some patients, and long-term survivors are not uncommon. In the past, for cases with lung cancer invading SVC, traditional surgery can be done through resection and replacement of SVC (including simple removal and replacement of SVC, and replacement of bilateral innominate veins), repair of SVC, and partial resection of SVC wall followed by direct closure (1). Using the traditional method, the removal of SVC requires occlusion of a part of the sidewall by a clamp or complete occlusion of the vessel from the proximal to distal ends. When a video-assisted thoracic surgery (VATS) manual suture technique is applied, many surgical devices need to pass through the minimally invasive incision(s); in addition, the suturing needs to be performed using needle holders. Thus, this technique is highly challenging for most thoracic surgeons. However, few articles have described the application of complete VATS for the tumors invading SVC, and its surgical modes and skills require further investigations. Automatic mechanical suturing enables the direct resection of the sidewall of SVC and avoids the blockage of SVC and manual suturing, thus reducing the difficulty of minimally invasive surgery.
Case presentation
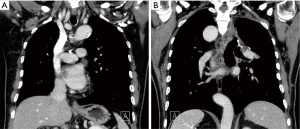
The case selection criteria were as follows (2): (I) the general condition of the patient is good, the functions of various organs are normal, and thus the patient can tolerate a surgery; (II) preoperative examinations confirm that there is no distant metastasis or positive N3; (III) in patients being N2 node-positive, if there is no obvious fusion or metastasis to multiple stations, surgical resection may be applied in those with localized lymph node metastasis; (IV) the range of invaded SVC should be no more than 1/6 of its circumference (Figure 1).
Anesthesia
After the induction of general anesthesia, the patient was under double-lumen endotracheal intubation.
Body position
The patients were often placed in a lateral decubitus position on the unaffected side. The waist bridge is elevated to maximize the intercostal spaces and thus facilitate the operation.
Surgical procedures
Incisions: typically three incisions will be more feasible. Observation port (incision): in the 6th or 7th intercostal space at anterior axillary line, about 1 cm in length. Main operation incision: in the 3rd or 4th intercostal space at anterior axillary line, about 4 cm in length. Auxiliary operation incision: within the same intercostal space with the observation port; in the 6th or 7th intercostal space at posterior axillary line, about 1 cm in length.
Surgical steps
The pulmonary fissure is cut open to expose the upper lobe branch of the right upper pulmonary vein, which is then transected using the endoscopic cutter/stapler (Figure 2). To facilitate the stapler to pass through the intervascular space, a silk suture can be used to lift the vein and the endoscopic cutter/stapler can be guided by a urinary catheter.
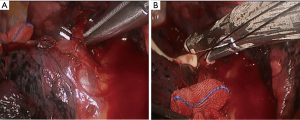
Dissect to expose the pulmonary arterial branch in posterior segment of the right upper lobe and then transect it with high intensity focused ultrasound (HIFU) after it is blocked off with vascular clamps (Figure 3). To ensure the safety, the proximal end is usually blocked off using two vascular clamps, while the distal end of the pulmonary arterial branch can be directly transected using HIFU.
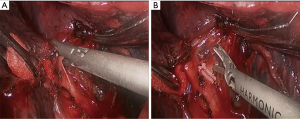
Expose the first branch of the right upper pulmonary artery, which is then transected using the endoscopic cutter/stapler (Figure 4). To facilitate the stapler to pass through the intervascular space, the endoscopic cutter/stapler can still be guided by a urinary catheter. Transect the right upper lobe bronchus.
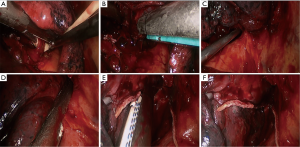
Under general anesthesia with double lumen tube, resection of the sidewall of SVC using VATS mechanical suture technique was performed on August 18th 2010 (Figure 5).

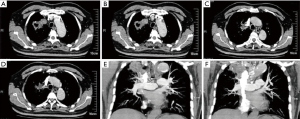
Postoperative computed tomography (CT)
The SVC was patent and no stricture was found. The right middle bronchial anastomosis was patent (Figure 6).
Discussion
The method used in this study has two key technical concerns: first, how to ensure safe resection without bleeding margins of the sidewall, and second, how to ensure thoracoscopic resection with negative margins while maintaining sufficient blood reflux in the residual vessel.
Regarding the first technical issue, in thoracoscopic lung surgery, cutting blood vessels of different diameters and thicknesses with a stapler is a common operation, such as cutting the pulmonary artery, pulmonary vein, or even azygos vein. From a technical point of view, resection of the sidewall of the SVC with a stapler is essentially nothing different from handling the pulmonary artery, pulmonary vein or even azygos vein of different diameters. Therefore, we do not worry whether the cutting margin can be properly stapled and if bleed leakage occurs. In view of the experience with operations for the latter, we did not administer systemic heparin during the surgery or routine anticoagulation after it.
Regarding the second technical issue, since the present cohort had advanced lung cancer, the surgery was relatively complex, and the surgical indications should therefore be properly observed. From the technical view for minimally invasive surgery, we are most concerned about the length and the circumference of invasions in the SVC, especially the latter. To this end, we need to be careful in selecting eligible cases. In our current case, the inclusion criteria were mainly based on the diameter of SVC and the width of endoscopic cutter/stapler (take Ethicon Echelon Flex 60 as an example) (Figure 7):
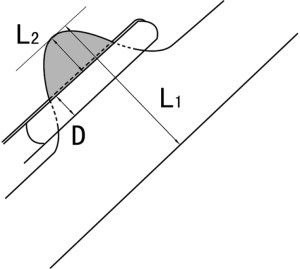
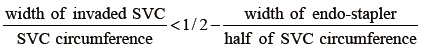
in which the width of the endoscopic linear cutter/stapler is about 1 cm. Since the SVC diameter is about 2 cm in most Chinese patients, the range of the invaded SVC should be less than 1/6 of the circumference. As for a patient with a large body size, or a more delicate stapler can be used, this range can be further expanded.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jones DR. Technique of superior vena cava resection for lung carcinomas. Operative Techniques in Thoracic and Cardiovascular Surgery 2008;13:274-82. [Crossref]
- Xu X, Chen H, Yin W, et al. Initial experience of thoracoscopic lobectomy with partial removal of the superior vena cava for lung cancers. Eur J Cardiothorac Surg 2015;47:e8-12. [Crossref] [PubMed]
- Xu X, Qiu Y, He J, et al. Resection of the sidewall of superior vena cava using VATS mechanical suture technique. Asvide 2016;3:159. Available online: http://www.asvide.com/articles/917