Video-assisted thoracoscopic surgery resection and reconstruction of thoracic trachea in the management of a tracheal neoplasm
Introduction
Surgery remains the treatment of choice for tracheal tumor. The purpose of surgery is to completely resect the tumor and the adjacent tracheal tissues that have been invaded by the tumor, followed by the anastomosis of the distal and proximal ends of the trachea to finalize the tracheal reconstruction. In the past, open incision is used during the surgery for tracheal tumors: for tumors located in the cervical trachea, the incision is made in the neck; for tumors located in the thoracic trachea, however, the incision is often made in the left or right chest. Along with advances in video-assisted thoracoscopic surgery (VATS) minimally invasive techniques and devices, VATS lobectomy or even total pneumonectomy has become possible. However, few literatures have reported the VATS tracheal resection and reconstruction for tracheal masses. To achieve radical resection of tracheal tumor and meanwhile reduce the injury to patients, we describe the application of intubated VATS tracheal resection and reconstruction in the management of a tracheal neoplasm, with particular focus on the anesthesia and operation skills during the surgery.
Case presentation
Patient
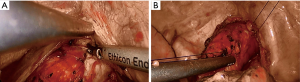
A 60-year-old non-smoking male patient developed progressively worsening cough, hemoptysis, and shortness of breath in the past 1 month. Chest computed tomography (CT) showed a space-occupying lesion inside the upper trachea, along with the stricture of the corresponding tracheal lumen. Low-grade malignant tumor or benign lesion was considered. The mass was sized 2.5 cm × 2 cm × 2 cm and located at the level of the second thoracic vertebra (Figure 1). Multiple bullae were seen at the apex of the right upper lobe, whereas fibrous lesions were visible at the apexes of both upper lungs and the basal segment of left lower lobe. Whole-body bone scan showed no abnormality. Plain CT scans of head and abdominal organs did not find any suspicious lesion. Pulmonary function tests showed decreased FEF 25–75%, MEF 50%, and MEF 25%, whereas the pulmonary ventilation function was basically normal.
Anesthesia
After the induction of general anesthesia, the patient was under endotracheal intubation. Sufentanil (10 μg) and propofol (80 mg) were used for anesthetic induction. Muscle relaxant vecuronium (0.1 mg/kg) was applied. Ventilation with tracheal intubation was applied when spontaneous breathing stopped. Tracheal intubation was completed under the guidance of fibrobronchoscope. Touching of the intratracheal mass by the tracheal tube should be avoided. The tracheal tube was connected with the anesthesia ventilator for mechanical ventilation. The oxygen concentration was adjusted according to blood oxygen saturation to maintain the blood oxygen saturation above 95%. During the surgery, anesthesia was maintained using remifentanil (0.03–0.05 μg/kg per min) and propofol (0.2 mg/kg per min). In addition, the anesthesiologist also prepared devices for intrathoracic tracheal intubation, which was used to maintain oxygen supply during tracheal reconstruction. The depth of anesthesia was measured using the EEG bispectral index during the surgery.
Surgical process
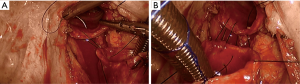
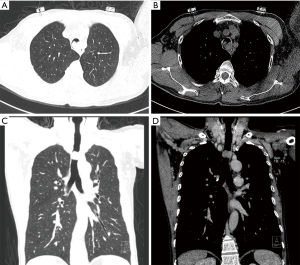
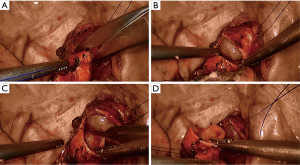
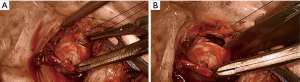
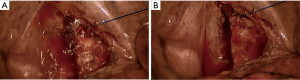
The patient was placed in a left lateral decubitus position. A 1-cm observation port was made in the 6th intercostal space at right anterior axillary line for the placement of 30° thoracoscope. In addition, two incisions (2.5 and 0.5 cm in length, respectively) were made in the 3rd intercostal space at anterior axillary line and in the 7th intercostal space at posterior axillary line as the operation ports. During the surgery, we found that the collapse of the operated lung was good; then, the lung was lifted forwards to achieve good surgical field. Mediastinal pleura was cut open using HIFU, and the trachea from the level of suprasternal notch to that of carina was dissociated (Figures 2,3). After the trachea was suspended using rubber tubes and sutures (Figure 4), the distal end of the trachea that was about 1.0 cm away from the tumor edge was dissected (Figure 5); meanwhile, the tracheal tube with a balloon was inserted via the thoracic cavity to ensure the patency of airway (Figure 6). Then, the trachea was transected at the proximal end of the tumor to completely resect the tracheal mass (Figures 7,8). Intra-operative frozen section analysis showed that the surgical margin was negative. The mass was pathologically confirmed to be low-grade malignant epithelial tumor. Reconstruction of the trachea was completed by continuous end-to-end anastomosis of the stumps using 2–0 Prolene sutures (Figure 9). After the reconstruction of the posterior wall of the trachea was completed, the tracheal tube was withdrawn via the thoracic cavity and then inserted via mouth (Figure 10), so that the reconstruction of the lateral and anterior walls of the trachea could be completed (Figures 11,12). The anastomotic leak test was performed using sterile saline (Figure 13). After it was confirmed that there was no anastomotic leak or intrathoracic active bleeding, we closed the chest incisions, while two chest tubes (up and down) were remained in the thoracic cavity for drainage. The intraoperative SpO2was maintained between 97% and 100%. Blood gas analysis showed that the patient had no non-respiratory acidosis. The patient’s vital signs remained stable throughout the operation.


Postoperative conditions
Postoperative chest X-ray showed that the operated lung was well reexpanded and there was no sign of pneumothorax. The patient occasionally had cough and sputum production but did not have symptoms such as shortness of breath, chest pain, or dyspnea. He complained of pain at the site of chest tube placement. Non-steroidal anti-inflammatory drugs and ambroxol were administered to alleviate the symptom. The patient did not experience any surgery-related complication. The chest tubes were withdrawn on the third postoperative day, and the patient was discharged on the seventh postoperative day. The patient was advised to avoid any strenuous activity. Meanwhile, he was advised to keep his head in a lower neutral position, so as to prevent hyperextension of his neck. During the 3-month follow-up, the patient had good general conditions and did not complain of any respiratory symptom.
Postoperative diagnosis
The final pathological diagnosis was: low-grade adenocarcinoma in the trachea (Figure 14).
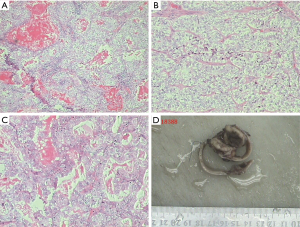
Immunohistochemistry: CK (+), EMA (+), CEA (−), S100 (−), Syn (−), CgA (−), Cd56 (−), CK7 (+), Napsin A (−), TTF1 (−), Calponin (−), P63 (−), CK5/6 (−), P40 (−), Cd10 (−), Vim (+), CK20 (−), CDX2 (−), PAX-8 (−), PSA (−), HMB45 (−), Ki67 (about 5%).
Special staining: mucicarmine staining (+), periodic acid-Schiff (PAS) digest stain (+), AB (+), and PAS (+).
Lymph nodes: station 1 (0/2), station 2 (0/5), and station 2/4 (0/1).
The detail of the surgical process was demonstrated in the video (Figure 15).
Discussion
Tracheal tumor is a relatively uncommon tumor of upper respiratory tract (2). Typically it is less malignant and is often localized within tracheal lumen. The common symptoms of tracheal tumors include cough, coughing up blood, shortness of breath, and wheezing. However, some patients can also be asymptomatic. When the tumor becomes larger, the patient may suffer from difficulty breathing or even asphyxia (2-4). Therefore, early diagnosis and early treatment are particularly important for tracheal tumors. A variety of treatment methods including fibrobronchoscopic tumor resection, radiotherapy, and conventional surgical resection have been development for tracheal tumors (5). However, the preferred radical treatment remains the complete resection of the tumor followed by tracheal reconstruction.
However, this surgery is somehow difficult due to various reasons. First, the thoracic trachea is located above the thoracic outlet and approaching the apex of cervical pleura, which are surrounded by many vital structures such as the superior vena cava. Therefore, the operation range is relatively small, and the surgical field is somehow limited. Second, part of the trachea needs to be resected before reconstruction. Thus, to ensure oxygen supply during the surgery, the anesthesiologist needs to withdraw the orally inserted tracheal tube during the resection of tracheal tumor; meanwhile, the operator must insert another tracheal tube into the distal end of trachea via the thoracic cavity to ensure the patency of airway. During tracheal reconstruction, the anesthetist needs to insert a new tracheal tube by mouth, whereas the operator must remove the transthoracically inserted tracheal tube (6). Furthermore, the anesthesiologist needs to continue to place the transorally-inserted tracheal tube to the distal end of the trachea to ensure the tube pass through the anastomosis. Due to the complexity of the procedure, the operator must have rich and solid experiences and skills in endoscopic suturing, along with close cooperation with the anesthesiologist.
In summary, VATS resection and reconstruction of trachea in the management of tracheal mass have certain advantages: (I) it reduces the surgery-related injuries; and (II) the zoom-in function of the thoracoscope enables finer suturing. However, it’s the surgical field is near the apex of pleural cavity, the visual field and surgical range are somehow limited. It remains a highly challenging procedure for most medical teams.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Li S, Liu J, He J, et al. Video-assisted thoracoscopic surgery (VATS) resection and reconstruction of thoracic trachea. Asvide 2016;3:157. Available online: http://www.asvide.com/articles/912
- Bhattacharyya N. Contemporary staging and prognosis for primary tracheal malignancies: a population-based analysis. Otolaryngol Head Neck Surg 2004;131:639-42. [Crossref] [PubMed]
- Grillo HC. Development of tracheal surgery: a historical review. Part 1: Techniques of tracheal surgery. Ann Thorac Surg 2003;75:610-9. [Crossref] [PubMed]
- Licht PB, Friis S, Pettersson G. Tracheal cancer in Denmark: a nationwide study. Eur J Cardiothorac Surg 2001;19:339-45. [Crossref] [PubMed]
- Schraube P, Latz D, Wannenmacher M. Treatment of primary squamous cell carcinoma of the trachea: the role of radiation therapy. Radiother Oncol 1994;33:254-8. [Crossref] [PubMed]
- Nakanishi K, Kuruma T. Video-assisted thoracic tracheoplasty for adenoid cystic carcinoma of the mediastinal trachea. Surgery 2005;137:250-2. [Crossref] [PubMed]