Postoperative survival for patients with thymoma complicating myasthenia gravis—preliminary retrospective results of the ChART database
Introduction
Due to the immunologic feature of the thymus, quite a few thymoma patients are accompanied with autoimmune disorders among which myasthenia gravis (MG) is the most important one with the incidence rate ranging 10–45%. In early times, MG once was reported to be the negative factor (1) because of a lack of experiences to deal with MG related complications after thymothymectomy (2-4). On the other hand, there has been an increasing body of evidences indicating that MG is related to better survival. However, the role of MG in the postoperative outcome for patients with thymoma is so far still not clear. The Chinese Alliance for Research in Thymomas (ChART) registry recruited patients with thymoma from 18 centers over the country in 20 years with the intention to compare the postoperative survival between patients with thymoma only and those with both thymoma and MG so as to have a preliminary understanding of how MG affects the prognosis of patients with thymoma.
Materials and methods
Patients
The ChART registry included patients with thymoma from 18 centers over the country from 1992 to 2012. Demographic and clinical data were reviewed. In this research, two groups were formed according to whether the patient complicated MG—MG group and non-MG group. All the demographic and clinical data were compared between the two groups. Patients were followed before their survival status were compared. Because only de-identified data were used for the study, informed consent was waived by Institutional Review Board (IRB).
The final pathologic staging was based on Masaoka-Coga staging system while the histology types were based on WHO classification. The resectability of thymoma was divided into R0 (no residue tumor), R1 (residue tumor microscopically), R2 (residue tumor macroscopically), and biopsy only according to the pathology of the sample margins and the operation note. The normal thymus was either completely removed (total resection of the thymus) or partly (resection of the tumor and a portion of the thymus) removed according to the surgeon’s preference. Data regarding chemotherapy and radiotherapy were also collected.
Statistical analysis
Statistical analysis was performed by the X test and the unpaired t test with the SPSS 14.0 for Windows. Prognostic factors were analyzed by the Kaplan-Meier method and Cox regression with respect to survival. Comparisons between survival curves were made by the log-rank test.
Results
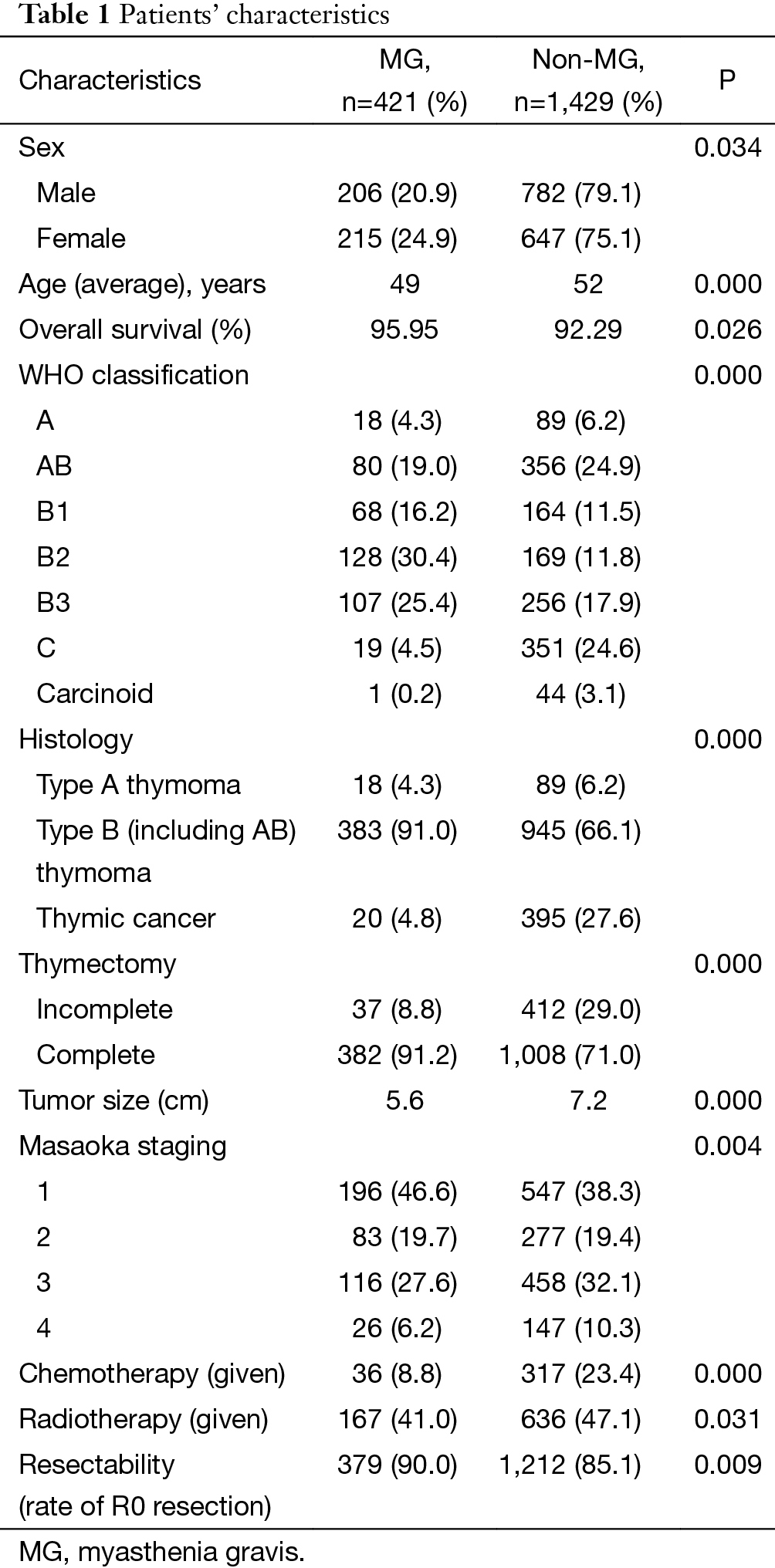
Patients’ characteristics: data of 2,306 patients were collected, and 1,850 patients entered this study, including 421 with and 1,429 without MG as showed in Table 1, after excluding the following ones: 49 patients only biopsied, 152 lack of surgical information, 124 without WHO classification, and 118 lack of Masaoka staging. There were more proportion of female in MG group than non-MG group (P=0.034) and the average age of MG group was significantly younger (49 vs. 52, P=0.000). The overall survival (OS) for MG group was significantly higher (95.95% vs. 92.29%, P=0.026). The tumor size of MG group was significantly smaller (5.6 vs. 7.2 cm, P=0.000). There were more percentage of patients with the histology of thymoma A and B (P=0.000) in MG group, and more percentage of patients with MG were in Masaoka stage I and II (P=0.004). R0 resection and complete thymectomy were both done significantly more in MG group (90.0% vs. 85.1%, P=0.009; 91.2% vs. 71.0%, P=0.000). Postoperative adjuvant chemotherapy or radiotherapy were given more in patients without MG (8.8% vs. 23.4%, P=0.000; 41.0% vs. 47.1%, P=0.03).
Full table
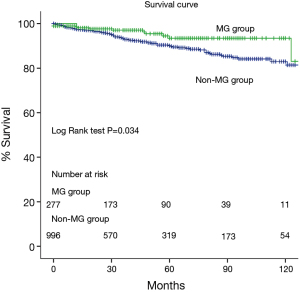
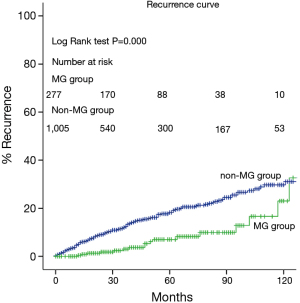
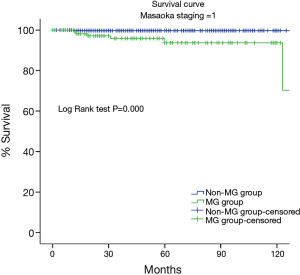
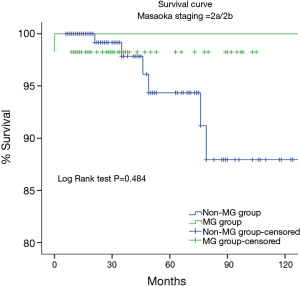
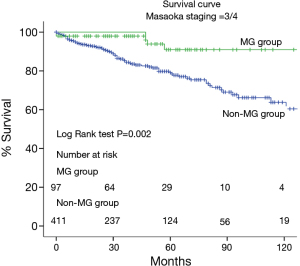
The 5-year and 10-year OS rates were both higher in MG group (93% vs. 88%, 83% vs. 81%, P=0.034, respectively) (Figures 1,2,3,4). However, the survival rate was significantly higher in non-MG group when the Masaoka staging was 1 (P=0.000), and the result was opposite when the Masaoka staging was 3/4 (P=0.003).
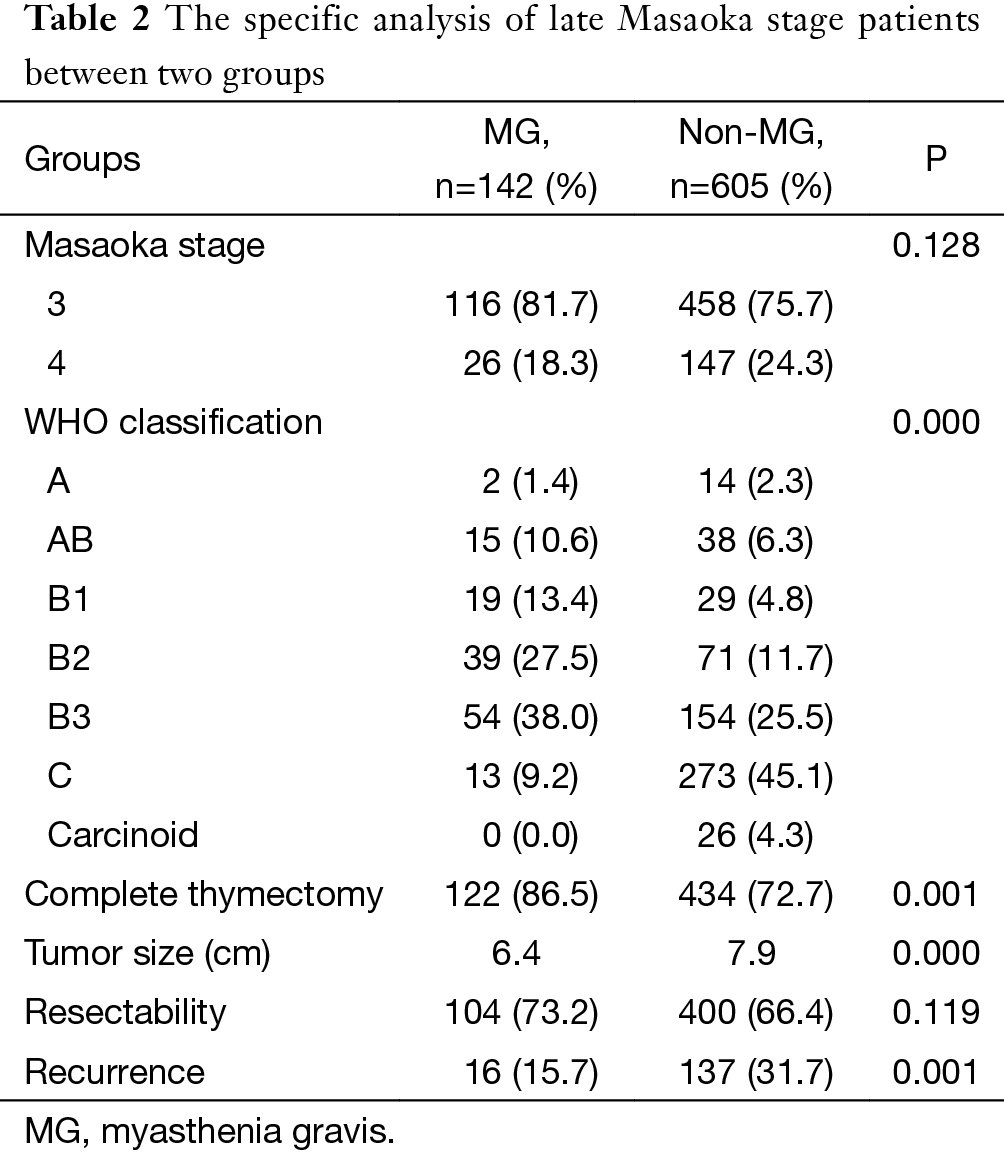
Among patients with advanced stage thymoma (stage 3, 4a, 4b) (Table 2), the constituent ratios of 3 and 4 were similar between MG and non-MG group. Histologically, however, there were significantly more proportion of AB/B1/B2/B3 in the MG group while there were more C in the non-MG group (P=0.000). The tumor size of MG group was also significantly smaller (6.4 vs. 7.9 cm, P=0.000). Total thymectomy had been done in more proportion of patients in MG group (86.5% vs. 72.7%, P=0.001), but the two groups were comparable in resectability.
Full table
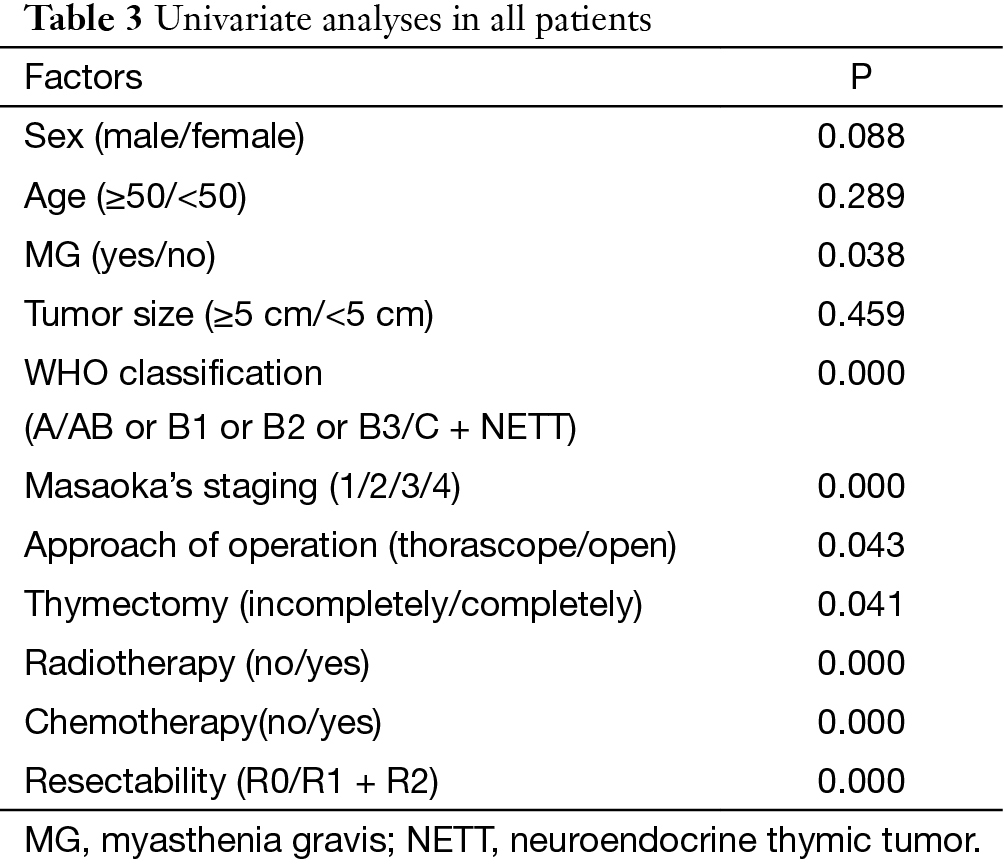
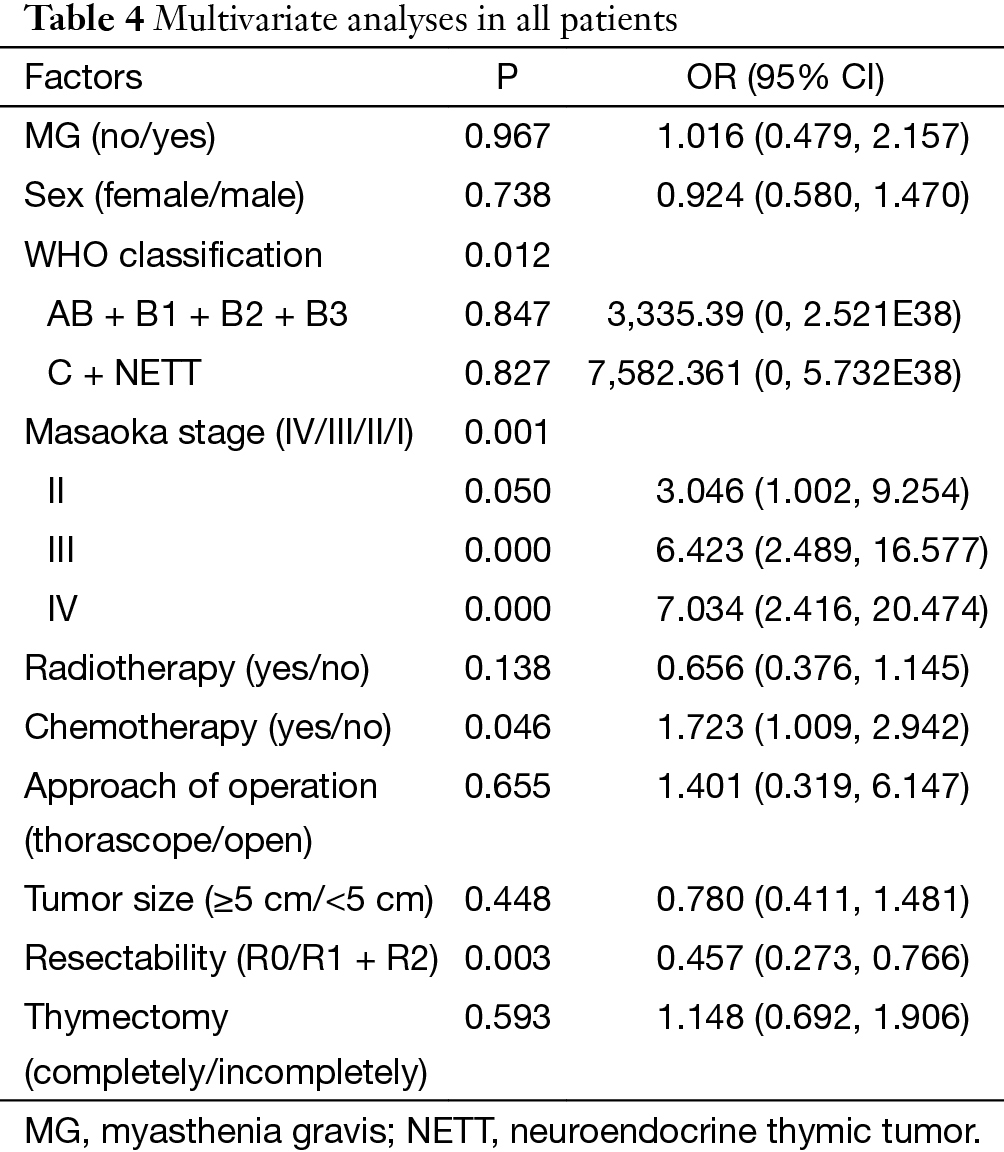
Univariate analyses showed that MG, WHO classification, Masaoka stage, approach of operation, chemotherapy and radiotherapy and resectability were significant factors for survival (Table 3). Whereas in multivariate analyses of Cox regression model (Table 4), WHO classification, Masaoka stage, and resectability were strong independent prognostic indicators.
Full table
Full table
In patients with advanced stage thymoma, the postoperative recurrence was much higher in non-MG group than MG group (Figures 5,6).

Discussion
The appearance of MG in patients with thymoma makes them stand out from the population not only because of the fact the perioperative management has become more complicated, but the postoperative outcome is somewhat different. Results of earlier studies on postoperative prognosis of thymoma are quite different from those of recent studies (2,3,5). Anyway, MG does have an impact on patients with thymoma, as is shown in this multicenter study. Patients in MG group were at earlier stage of the disease and there were more proportion of type AB and B in this group, while patients with thymoma only were at quite advanced stage and their pathologic classification tended to be worse. The onset of MG is a good reason for the timely diagnosis and attention for the thymic tumor. The overall R0 resection rate, an independent prognostic factor according to the multivariate analysis of this study, was also higher in patients with MG. All these might account for the positive influence of MG on the long term outcome of subjects with thymoma.
The inter-relations among MG, tumor histology and Masaoka staging have been under the study of quite a few physicians (6,7). Ruffini et al. proposed that two models, early Masaoka stage A/AB WHO type and high Masaoka stage/B WHO type, were most frequently seen in MG patients. He noted the influence of MG on Masaoka staging and histology, and his study showed only Masaoka stage had a prognostic significance on OS and disease free survival (DFS) (6). His conclusions could be well applied to the results of this multicenter study except that in the ChART database the independent prognostic factors included histology, tumor resectability besides Masaoka stage, and MG seemed to have a positive impact on all three elements.
MG affects patients with thymoma in quite an interesting way. Although multivariate analysis indicated that MG was not an independent prognostic factor for a superior survival status, univariate study showed that on the whole patients with MG actually lived longer. Further investigation found MG had a different influence on the patients’ survival in different Masaoka stages. Theoretically MG is usually not fatal and adds no mortality to thymoma providing adequate medical care is given. However, perioperative death from myasthenic crisis or pulmonary complications is possible if importance is not fully attached. In this study the worse survival status of MG group in early stages might result from the increased death contributed by MG related complications. Dramatically, the survival advantage of MG group became extremely obvious when thymoma was in quite advanced stage. This might be explained by the better pathologic classification and lower recurrence rate of thymoma in the MG group. Although this advantage was to some extent offset by the increased mortality of MG group in early stages, the positive effect of MG on the OS of thymoma patients still came into sight as shown by the single variant analysis. Hopefully, as the understanding and intervention for MG has developed rapidly, which minimizes death caused by MG, and multidisciplinary collaboration for thymoma patients with MG has become much tighter, an even better prognosis of thymoma patients with MG will be expected in future studies.
As a retrospective study, loss of patients’ information in the ChART database caused quite a lot of cases to be excluded from the analysis. Bias hence produced seemed inevitable. In addition, patients included in the data base spanned 20 years during which medical progression was rapid, especially for MG. Therefore medical care received by these patients was not homogeneous. A prospective study may be needed to prove the results of this analysis.
Acknowledgements
None.
Footnote
Members of Chinese Alliance for Research in Thymomas (ChART): Yi Shen, Yucheng Wei, Affiliated Hospital of Qingdao University, Qingdao, China; Yin Li, Guanghui Liang, Affiliated Cancer Hospital of Zhengzhou University, Zhengzhou, China; Keneng Chen, Hao Fu, Beijing Cancer Hospital, Beijing, China; Hezhong Chen, Shihua Yao, Changhai Hospital, Shanghai, China; Youbin Cui, Yanzhong Xin, First Affiliated Hospital of Jilin University, Changchun, China; Renquan Zhang, Ningning Kang, First Hospital of Anhui Medical University, Hefei, China; Lijie Tan, Jianyong Ding, Hao Wang, Gang Chen, Jie Wu, Zhongshan Hospital, Fudan University, Shanghai, China; Chun Chen, Wei Zheng, Fujian Medical University Union Hospital, Fuzhou, China; Liewen Pang, Fangrui Wang, Huashan Hospital, Fudan University, Shanghai, China; Yangchun Liu, Qing Lin, Jiangxi People’s Hospital, Nanchang, China; Yongyu Liu, Yongkai Wu, Liaoning Cancer Hospital, Shenyang, China; Wentao Fang, Jie Zhang, Yan Shen, Changlu Wang, Lei Zhu, Zhitao Gu, Shanghai Chest Hospital, Shanghai Jiao Tong University, Shanghai, China; Yongtao Han, Lin Peng, Sichuan Cancer Hospital, Chengdu, China; Jianhua Fu, Qianwen Liu, Department of Thoracic Surgery, Guangdong Esophageal Cancer Institute, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center of Cancer Medicine, Guangzhou, China; Zhentao Yu, Jie Yue, Tianjin Cancer Hospital, Tianjin, China; Peng Zhang, Yuan Chen, Tianjin Medical University General Hospital, Tianjin, China; Yun Wang, Yingcai Geng, West China Hospital, Sichuan University, Chengdu, China; Xinming Zhou, Hongguang Zhao, Zhejiang Cancer Hospital, Hangzhou, China.
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Maggi G, Casadio C, Cavallo A, et al. Thymoma: results of 241 operated cases. Ann Thorac Surg 1991;51:152-6. [Crossref] [PubMed]
- Okumura M, Miyoshi S, Takeuchi Y, et al. Results of surgical treatment of thymomas with special reference to the involved organs. J Thorac Cardiovasc Surg 1999;117:605-13. [Crossref] [PubMed]
- de Perrot M, Liu J, Bril V, et al. Prognostic significance of thymomas in patients with myasthenia gravis. Ann Thorac Surg 2002;74:1658-62. [Crossref] [PubMed]
- Maggi G, Casadio C, Cavallo A, et al. Thymectomy in myasthenia gravis. Results of 662 cases operated upon in 15 years. Eur J Cardiothorac Surg 1989;3:504-9; discussion 510-1. [Crossref] [PubMed]
- Kondo K, Monden Y. Thymoma and myasthenia gravis: a clinical study of 1,089 patients from Japan. Ann Thorac Surg 2005;79:219-24. [Crossref] [PubMed]
- Ruffini E, Filosso PL, Mossetti C, et al. Thymoma: inter-relationships among World Health Organization histology, Masaoka staging and myasthenia gravis and their independent prognostic significance: a single-centre experience. Eur J Cardiothorac Surg 2011;40:146-53. [Crossref] [PubMed]
- Filosso PL, Venuta F, Oliaro A, et al. Thymoma and inter-relationships between clinical variables: a multicentre study in 537 patients. Eur J Cardiothorac Surg 2014;45:1020-7. [Crossref] [PubMed]