
Utilizing the chest tube insertion site as the site of initial trocar insertion with an optical-access trocar in video-assisted thoracoscopic surgery for spontaneous pneumothorax
Introduction
Insertion of an optical-access trocar as the initial trocar under direct view in laparoscopic procedures (1) is termed “the optical view method” (2). An endoscope can be attached to the inner cylinder of the optical-access trocar to allow visualization of body wall layers.
Video-assisted thoracoscopic surgery for spontaneous pneumothorax is typically performed following preoperative insertion of a chest drain. The pleurocutaneous fistula formed during chest drain insertion allows more convenient and reliable trocar insertion, thereby avoiding the creation of a new surgical wound.
However, blind trocar insertion though the pleurocutaneous fistula formed during chest drain insertion is technically challenging as it relies on the tactile sensation of the surgeon. As the trocar is inserted using trial and error, there is a risk of damage to the lungs and fistula.
Therefore, we evaluated the use of the optical view method when replacing the initial trocar and preoperatively placed chest drain. In our optical view method using the optical-access trocar, the initial trocar may be inserted into the pleural cavity through the fistula formed during chest drain placement under monitor visualization. The present study aimed to assess the safety and feasibility of our optical view method. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-489/rc).
Methods
Patients
The present study comprised patients with spontaneous pneumothorax who underwent video-assisted thoracoscopic surgery at Saitama Hospital between April, 2017 and December, 2019. A 20-French trocar catheter was placed as a chest tube. No signs of infection (i.e., erythema, pain, local warmth, or edema) at the chest tube insertion site were observed at the beginning of surgery.
Devices
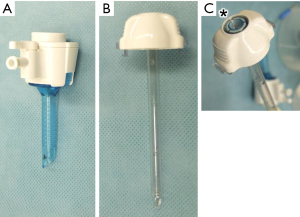
An optical-access trocar (Kii® Optical Access System, Z-thread, CTR 05, 5 mm × 55 mm, Applied Medical Resources Corp., US) was used (Figure 1).
Surgical methods
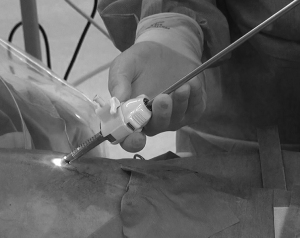
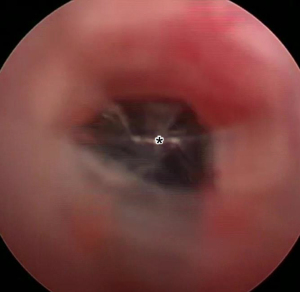
All surgeries were performed under general anesthesia with one-lung ventilation using a double lumen tube. Immediately prior to surgery, an optical-access trocar as the initial trocar was prepared with a 5-mm diameter rigid direct endoscope attached to the inner cylinder. The preoperatively placed chest drain was removed at the beginning of surgery and the initial trocar was inserted into the chest tube insertion site (Figure 2). Under visualization of the tip of the trocar using the attached endoscope, the trocar was advanced into the fistula formed by the chest tube (Figure 3). Once the tip of the trocar reached the thoracic cavity, the inner cylinder and direct endoscope were removed and used as the first access port. After removing the inner cylinder from the direct endoscope, the endoscope was changed to a 30-degree squint and inserted into the thoracic cavity through this port. The time required for the initial trocar to reach the thoracic cavity after contact with the chest tube insertion site was measured.
A skin incision was made at a site distant to the initial trocar, and a second access port was placed using a normal trocar. We then assessed for lung injury during insertion of the initial trocar via intra-thoracic observation from the second access port. After the addition of a third access port, three-port thoracoscopic surgery for spontaneous pneumothorax was performed according to the standard method. A chest tube was placed at a site distant to the initial trocar before the end of surgery. Wounds were sutured after bleeding at the initial trocar site had been controlled. Cefazolin sodium was administered 30 minutes before the start of surgery, at 8 pm after surgery, and at 8 am on the day following surgery as prophylaxis against wound infection. Wounds were reviewed for signs of infection at 10 days postoperatively. Complications were defined according to the Clavien-Dindo classification (3).
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The present study was approved by the ethics committee of Saitama Hospital (approval number R2017-22). Informed consent was obtained from all individual participants involved in the study.
Statistical analysis
For descriptive statistics, we show mean and standard deviation for continuous variables. For categorical variables, we show counts and proportions.
Results
This study comprised 28 patients who consented to participation in this study (Table 1).
Table 1
| Characteristic | Case (n=28) |
|---|---|
| Age (years) | 42.9±23.3 |
| Sex, n (%) | |
| Male | 26 (92.9) |
| Female | 2 (7.1) |
| Disease, n (%) | |
| Primary spontaneous pneumothorax | 18 (64.3) |
| Secondary spontaneous pneumothorax | 10 (35.7) |
| Side, n (%) | |
| Right | 13 (46.4) |
| Left | 15 (53.6) |
| Preoperative chest tube placement period (days) | 10.0±6.4 |
Data are presented as the mean ± standard deviation unless otherwise noted.
The site of preoperative chest tube insertion was at the lateral thoracic region in 27 cases and the 2nd intercostal midclavicular line in one case. Among the 27 cases with chest drains placed in the lateral thoracic region, the chest tube was inserted into the 4th, 5th, 6th, and 7th intercostal spaces in 1, 9, 14, and 3 cases, respectively.
In 26 out of 28 cases (92.9%), the initial trocar was successfully inserted into the preoperatively placed chest drain insertion site (Table 2). In two cases where the trocar tip could not be easily visualized, the tip of the trocar was deviated from the fistula (Figure 4). An extended incision was made in the skin at the insertion site and a normal trocar was inserted via the usual method.
Table 2
| Outcomes | Case (n=28) |
|---|---|
| Approach, n (%) | |
| Optical view method | 26 (92.9) |
| Transition to method using a normal trocar | 2 (7.1) |
| Surgery time (min) | 126.2±86.4 |
| Bleeding volume (mL) | 14.1±38.8 |
| Postoperative complication, n (%) | |
| Persistent air leakage | 2 (7.1) |
| Pneumonia | 1 (3.6) |
| Wound trouble | 0 (0.0) |
| Postoperative chest tube placement period (days) | 2.0±2.5 |
| Postoperative length of stay (days) | 5.6±5.0 |
Data are presented as the mean ± standard deviation unless otherwise noted.
In 8 cases with video recording, the initial trocar reached the thoracic cavity after contact with the chest tube insertion site in a mean duration of 21.5±9.4 s. The average total surgical duration in 28 cases was 126.2±86.4 minutes. No lung injury or pulsatile bleeding around the initial trocar was observed in any case.
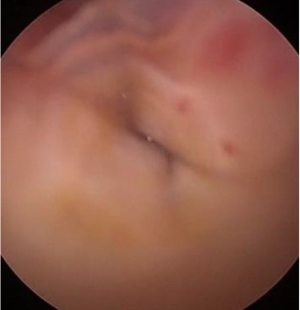
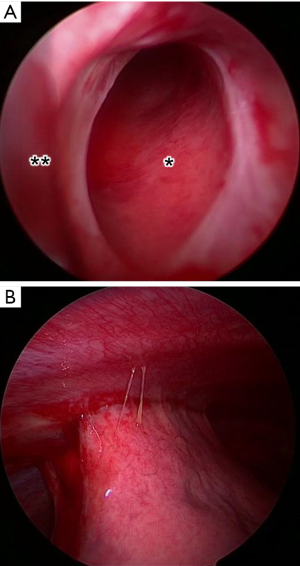
In one case, pleural adhesions were observed around the trocar insertion site (Figure 5); however, the trocar was inserted without lung damage. The mean duration of postoperative chest tube placement in 28 cases was 2.0±2.5 days.
No cases of postoperative wound infection or wound dehiscence were observed.
Discussion
The present study evaluated the utility of initial trocar insertion into the chest tube removal site during video-assisted thoracoscopic surgery for spontaneous pneumothorax by applying the optical method. In 26 out of 28 cases (92.9%), the initial trocar was successfully replaced into the insertion site of the preoperatively placed chest tube.
The optical view method is a well-described method of initial trocar insertion during laparoscopic surgery (2). The optical-access trocar used as the initial trocar is made from transparent plastic and has a conical shape with a blade at the tip, such that the trocar can be punctured while the endoscope is attached to the inner cylinder.
The optical view method is performed under a skin incision at the initial trocar insertion site according to the outer diameter of the optical-access trocar. The tip of the trocar is inserted into the subcutaneous tissue at the skin incision with the endoscope attached to the trocar inner cylinder. The direction of movement can be observed through the transparent tip of the trocar from the endoscope attached to the inner cylinder of the trocar. Therefore, the trocar can be inserted into the body cavity under monitor visualization during penetration of subcutaneous tissues, muscular layer, and finally the peritoneum or pleura.
The optical view method is predominantly used in laparoscopic surgery. Compared to the open method using for small laparotomies, the optical view method is associated with the advantages of less bleeding (2), shorter time to pneumoperitoneum (1), less gas leakage (1,4), and is unaffected by body shape (5,6). However, injury to intra-abdominal structures is common despite trocar insertion under monitor visualization. Organ damage associated with the laparoscopic optical view method has previously been reported (5,7-9). According to a single-center report, the optical view method is associated with a 2.1% frequency of organ damage (10). In addition, four cases of death due to damage to large blood vessels, liver, or intestinal tract have been reported (11,12).
Initial trocar insertion during video-assisted thoracoscopic surgery can cause lung injury (13). For patients with a chest tube placed during surgery, the fistula formed during chest tube placement can be used for trocar insertion. Once the trocar has passed through the fistula, the initial trocar should be able to be reliably inserted into the pleural cavity. However, blind trocar insertion though the fistula formed by the chest tube is technically challenging as it relies on the tactile sensation of the surgeon. The location, length, and path of the fistula formed by the chest tube varies according to patient posture. Chest tube drainage, which is generally performed as an initial treatment for spontaneous pneumothorax, is typically performed by emergency physicians, respiratory physicians, and general physicians in addition to respiratory surgeons. Therefore, the insertion site and insertion route of the chest tube may differ depending on the experience and skill of the initial therapist. The optical view method described in the present study allows for successful initial trocar insertion without injury, even when the fistula tract is unknown.
The optical view method used in the present study differs from the laparoscopic optical view method in that it utilizes a fistula formed during chest tube placement during trocar insertion. In the optical view method of laparoscopic surgery, the initial trocar is inserted under visualization of the subcutaneous tissues, muscles, and pleura. Therefore, the conventional optical view method requires a deep understanding of endoscopic images. In our optical view method, trocar insertion proceeds under visualization of the inner wall of the fistula formed along the chest wall. The fistula appears as a black void from the tip of the endoscope. If the endoscope is adjusted so that the black void is in the center of the tip of the endoscope, successful trocar insertion results in no resistance during further advancement of the trocar. Thus, we believe the optical view method described in this study represents a simple and technically less challenging method of trocar insertion.
The price of an optical-access trocar (Kii® Optical Access System, Z-thread, CTR 05, 5 mm × 55 mm, Applied Medical Resources Corp., US) used in this study is USD 69.77, while the price of a normal trocar (thoracoportTM 5.5 mm, 179305, Cardinal Health K.K. Tokyo, Japan) used in our hospital before the study is USD 44.06. Identification of chest drain fistulae is technically challenging using a muscle retractor during port insertion. The incision into which the 20-French trocar is inserted is approximately 1 cm and therefore requires extension to allow for direct observation. Therefore, the use of optical-access trocars is slightly more expensive; however, it is beneficial to the patient in terms of safety and burden.
In the present study, there were 2 cases (7.1%) wherein initial trocar insertion failed. In both cases, the tip of the trocar did not proceed along the fistula formed in the chest wall but went straight along the chest wall, pierced the fistula wall, and proceeded into chest wall tissue leading to loss of trocar visualization. The tip of the optical-access trocar is sharp and can easily penetrate adjacent tissues if the trocar is carelessly advanced. The chest tubes used in the present study (20 Fr, 6.7 mm diameter) were thinner than the optical-access trocar (7.9 mm outer diameter). Normally, the inner diameter of the fistula is slightly larger than the diameter of the drain, thereby allowing the trocar to pass through with careful execution. Thus, careful surgical technique is required when using the optical view method (14).
When the initial trocar replaces the preoperatively placed chest tube, the risk of wound infection is reported to be 7.7% (15). No cases of postoperative infection were observed in the present study. The use of a chest tube insertion site as a port for endoscopic surgery does not require a separate skin incision for trocar insertion, thus being favorable in terms of invasiveness and cosmetics.
In the present study, the mean time required for the initial trocar to reach the thoracic cavity using the optical view method was 21.5 seconds. Although this was not compared to other techniques in the present study, we do not believe this method increases operative duration. Further, we consider the insertion time to be acceptable as this technique reliably avoids lung damage. According, we consider the optical view method to be safe without increased operative complexity or duration.
Conclusions
The results of the present study demonstrate the safety of the optical view method, which uses an optical-access trocar as the initial trocar to replace a chest tube placed preoperatively. No instances of lung damage, bleeding, or infection were observed in 26 out of 28 cases (92.6%) that underwent surgery for treatment of spontaneous pneumothorax. The optical view method of initial trocar insertion into a chest tube insertion site has utility in video-assisted thoracoscopic surgery for spontaneous pneumothorax in patients with preoperative chest drain placement.
Acknowledgments
We gratefully acknowledge the hard work of all nursing and physician staff present in our operating room.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-489/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-489/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-489/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Saitama Hospital (approval number R2017-22) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- String A, Berber E, Foroutani A, et al. Use of the optical access trocar for safe and rapid entry in various laparoscopic procedures. Surg Endosc 2001;15:570-3. [Crossref] [PubMed]
- Michitaka F, Masamichi S, Hiroki H, et al. Virtual reality training system of the optical access in initial trocal insertion for laparoscopic surgery. Med Virtual Real 2011;9:1-6. [Crossref]
- Dindo D. The Clavien-Dindo Classification of Surgical Complications. In: Cuesta MA, Bonjer HJ. editors. Treatment of Postoperative Complications After Digestive Surgery. Springer, 2014:13-7.
- Berch BR, Torquati A, Lutfi RE, et al. Experience with the optical access trocar for safe and rapid entry in the performance of laparoscopic gastric bypass. Surg Endosc 2006;20:1238-41. [Crossref] [PubMed]
- Sabeti N, Tarnoff M, Kim J, et al. Primary midline peritoneal access with optical trocar is safe and effective in morbidly obese patients. Surg Obes Relat Dis 2009;5:610-4. [Crossref] [PubMed]
- Tinelli A, Malvasi A, Mynbaev OA, et al. Bladeless direct optical trocar insertion in laparoscopic procedures on the obese patient. JSLS 2013;17:521-8. [Crossref] [PubMed]
- Mami S, Ruriko K, Noriko O, et al. The optical trocar insertion technique using Kocher clamps in laparoscopic surgery. Jpn J Gynecol Obestrics Endosc 2013;29:224-7.
- Mettler L, Ibrahim M, Vinh VQ, et al. Clinical experience with an optical access trocar in gynecological laparoscopy-pelviscopy. JSLS 1997;1:315-8. [PubMed]
- Wolf JS Jr. Laparoscopic access with a visualizing trocar. Tech Urol 1997;3:34-7. [PubMed]
- Brown JA, Canal D, Sundaram CP. Optical-access visual obturator trocar entry into desufflated abdomen during laparoscopy: assessment after 96 cases. J Endourol 2005;19:853-5. [Crossref] [PubMed]
- Sharp HT, Dodson MK, Draper ML, et al. Complications associated with optical-access laparoscopic trocars. Obstet Gynecol 2002;99:553-5. [PubMed]
- Thompson JE Jr, Bock R, Lowe DK, et al. Vena cava injuries during laparoscopic cholecystectomy. Surg Laparosc Endosc 1996;6:221-3. [Crossref] [PubMed]
- Takayuki K, Keiko U, Ikuta H, et al. Safety of thoracoscopy under local anesthesia. J Jpn Soc Respir Endosc 2006;28:582-4.
- Kesavadas T, Srimathveeravalli G, Arulesan V. Parametric modeling and simulation of trocar insertion. Stud Health Technol Inform 2006;119:252-4. [PubMed]
- Kesieme EB, Dongo A, Ezemba N, et al. Tube thoracostomy: complications and its management. Pulm Med 2012;2012:256878. [Crossref] [PubMed]


