Revival of impaired lung perfusion after sleeve lobectomy
Introduction
Pneumonectomy, a standard procedure for centrally-located lung cancer, may cause cardiopulmonary compromise, known as “post-pneumonectomy syndrome”. If the residual lung is preserved, sleeve resection can provide better postoperative quality of life by achieving equal or higher curability compared with pneumonectomy (1). We herein report a patient in whom impaired lung perfusion of the residual lung markedly recovered after right upper sleeve lobectomy for lung cancer invading the main bronchus. This is the first article to demonstrate the recovery of lung perfusion after sleeve lobectomy for lung cancer. The indications for sleeve lobectomy with an impaired residual lung are discussed.
Case presentation
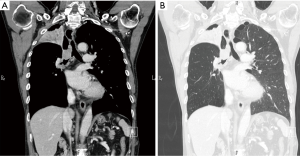
A 61-year-old male was referred to our department for lung cancer obstructing the right upper bronchus accompanied by total atelectasis of the right upper lobe. Bronchoscopy and chest computed tomography image examination revealed a 30 mm × 30 mm × 33 mm mass with an intraluminal growth at the right upper bronchus, invading into the main bronchus, and existing one bronchial ring distally from the carina (Figure 1). The right middle and lower lobes were well expanded without parenchymal damage and consolidation, while the right upper lobe was totally collapsed. The tumor did not invade the pulmonary vessels. The tumor was diagnosed as squamous cell carcinoma by an endobronchial biopsy. Lung perfusion scanning with 99mTc-macroaggregated albumin revealed decreased perfusion of the right lung to 7.3% (Figure 2). The pulmonary function showed restrictive and obstructive ventilatory impairment as follows: forced vital capacity (FVC) was 2.18 L (50.3% of predicted normal value) and forced expiratory volume in 1 second (FEV1.0) was 1.51 L (41.8% of predicted normal value).

As there were no distant metastases, we chose to perform surgical treatment. The surgery was performed via a posterolateral thoracotomy of the 5th intercostal space. After division of the superior pulmonary vein and pulmonary arteries branching to the upper lobe, the central and distal sites of the bronchus were divided at the level of the carina and truncus intermedius (two bronchial rings above the second bifurcation), with both diagnosed as negative surgical margins by rapid pathologic diagnosis. After removal of the right upper lobe, the airway was reconstructed by a one-stoma cranioplasty method using the pericardial fat pad as a wrapping material for the anastomosed site.
A bronchoscopy was performed at 5 days after the surgery. Although there was no anastomotic dehiscence, ischemia of the anastomotic site was observed. Routine bronchoscopy examinations revealed gradual recovery of the bronchial wall perfusion, and on day 23, the ischemia was radically cured. Pulmonary function and perfusion scans were re-examined at 2 months after the surgery. The perfusion of the right lung had markedly recovered up to 20.7%, accompanied by improvement of the pulmonary function up to FVC of 3.24 L (75.3% of normal) and FEV1.0 of 2.26 L (63.3% of normal). The patient is currently living his normal daily life without any recurrence at 6 months after the surgery.
Discussion
Sleeve resection is an ideal surgical procedure for centrally-located lung cancer, and can provide much better quality of life than pneumonectomy when the tumor can be completely eliminated. Anastomotic healing and residual lung function should be secured for a better surgical outcome. Bronchial circulation is impaired in cases with hypoperfusion of the pulmonary artery, which has a high risk of developing ischemia after bronchial anastomosis. Our case achieved successful recovery from anastomotic ischemia by wrapping the anastomotic site with the pericardial fat pad in advance. Reinforcement of the anastomotic site using autologous tissue might be necessary for cases with impaired lung perfusion.
The residual lung function after surgery is also an important factor for sleeve lobectomy. Sleeve lobectomy is contraindicated when the residual lung is irreversibly deteriorated by infection or destruction. However, the question arises as to whether the ischemic lung with normal lung parenchyma is worth preserving. Our case successfully recovered both the perfusion and function of the residual ischemic lung, through restoration of the reflex pulmonary vasoconstriction (RPV). Hypoxia of the alveolar causes vasoconstriction and hypertrophy of the pulmonary arteriole, leading to hypoperfusion of the less-ventilated residual lung. Ward et al. (2) reported reversibility of the RPV, suggesting that the duration of recovery of pulmonary perfusion after surgery depends on the preoperative vasoconstriction level. Bagan et al. (3) agreed with this suggestion, presenting 11 cases of benign and low-grade malignant tumors obstructing the unilateral airway that required bronchial sleeve resection. They examined preoperative and postoperative lung function and lung perfusion scans, finding that patients with incomplete arterial vasoconstriction recovered earlier than patients with completely abolished pulmonary perfusion. Many articles have discussed the recovery of ventilatory function after recanalization of the bronchus, whereas articles discussing the recovery of circulatory function, especially those comparing perioperative lung perfusion scans, are very rare (3,4). Moreover, these previous reports focused on bronchial sleeve resection for benign or low-malignant tumors, and there are no existing reports focusing on sleeve resection for high-malignant tumors. This is the first article to report recovery of vasoconstriction in a non-functional lung after sleeve lobectomy for lung cancer. Our case has successfully recovered the perfusion of the impaired lung, achieving remarkable improvement of his lung function.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Bölükbas S, Eberlein MH, Schirren J. Pneumonectomy vs. sleeve resection for non-small cell lung carcinoma in the elderly: analysis of short-term and long-term results. Thorac Cardiovasc Surg 2011;59:142-7. [Crossref] [PubMed]
- Ward HE, Jones RL, King EG, et al. Reversible ventilation and perfusion abnormalities in unilateral obstructed lung. Chest 1982;81:11-5. [Crossref] [PubMed]
- Bagan P, Le Pimpec-Barthes F, Badia A, et al. Bronchial sleeve resections: lung function resurrecting procedure. Eur J Cardiothorac Surg 2008;34:484-7. [Crossref] [PubMed]
- Takahashi S, Hata Y, Sasamoto S, et al. Recovery of lung perfusion after sleeve resection for tuberculous bronchial stenosis. Ann Thorac Surg 2012;93:2041-3. [Crossref] [PubMed]


