Subxiphoid uniportal video-assisted thoracoscopic surgery (VATS) for lobectomy: a report of 105 cases
Introduction
Thoracoscopic pulmonary lobectomy is widely used in clinics as the standard operation for the treatment of various benign and malignant thoracic diseases, of which the therapeutic efficacy has been confirmed (1). In traditional thoracoscopic surgery, the instruments and thoracoscope lens enter the thoracic cavity through the 2-4 operating ports on the lateral chest wall, which can easily cause postoperative chronic pain and chest wall numbness. Moreover, single-portal thoracoscopic surgery could also cause similar problems. Liu et al. reported a subxiphoid uniportal VATS left upper lobectomy in August 2014 (2). Since then, 105 subxiphoid uniportal video-assisted thoracoscopic surgery (VATS) for lobectomy have been successfully performed in our hospital. Herein we present the results of our experience with this procedure.
Methods
Clinical information
Preoperative chest CT showed all of the 105 cases had pulmonary nodules, 1 case had pulmonary nodules and a mediastinal tumor. As for the pulmonary nodules, the pre-operative thoracic CT and PET-CT suggested a high possibility of lung cancer. As all of the nodules were located in the center of the lobe, lobectomy rather than wedge resection or segmentectomy was necessary. Surgery was scheduled after pre-operative examinations were completed.
Surgical procedure
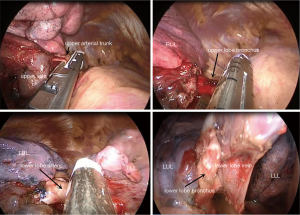
Among the patients undergoing subxiphoid uniportal VATS, 96 cases received unilateral surgery and 9 cases received bilateral surgeries. Surgical information is presented in Table 1. After general anesthesia and intubation with a double-lumen endotracheal tube, the surgical side was elevated to an angle of 30° (Figure 1), while the patients receiving synchronized bilateral surgeries were put into a horizontal position. After regular sterilization and draping, a 4–5 cm incision was made in the subxiphoid area (oblique incision under subcostal arch for unilateral surgery and subxiphoid transverse incision for bilateral surgeries), then subcutaneous tissue and rectus abdominis were separated along the subcostal margin. A subcostal tunnel was created and approached behind the posterior costal arch, the mediastinal pleura was opened at the cardiophrenic angle, the affected pleural cavity was accessed, and finally a wound protector was placed into wound. A thoracoscope with an angle of 30° was used during the operation. The pleural cavity was examined and the site of the lesion was determined. Additionally, the complexity of the interlobar fissure was examined. Lobectomy was then performed (Figure 2). Among the nine cases undergoing synchronized bilateral resections, each case received unilateral lobectomy with the contralateral side undergoing pulmonary wedge resection. The bilateral resections were performed sequentially, and the process of lobectomy was the same as for the unilateral resection. After surgery, a 28F pleural drainage tube was inserted through the subxiphoid incision (Figure 3) to the thoracic apex, and then connected to a drainage bottle. Bilateral pleural drainage tubes were inserted through the subxiphoid incision in bilateral resections (Figure 4). A deep venous puncture catheter was inserted through the 7-8th intercostal on lateral chest wall, which was connected to a drainage bag after surgery. The incision was closed layer by layer. All the patients returned to the postoperative care ward after surgery.
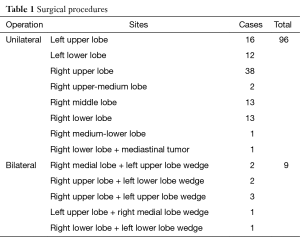
Full table


Statistical analysis
A total of 90 patients undergoing standard intercostal uniportal VATS lobectomy were included as the control group. The patients’ characteristics were listed in Table 2. Surgical results, complications and pain score were compared between two groups. The quantitative variables are expressed as mean±standard deviation, median and rang. Qualitative variables are expressed by means of frequencies and the corresponding percentages. The Mann Whitney U test was used for quantitative variables and Chi square test or Fisher exact test was used for qualitative variables. SPSS 19.0 for Windows for statistical analysis, with P<0.05 as statistically significant.

Full table
Results
Patients characteristics
In the subxiphoid group, there were 47 males and 58 females, with an average age of 58.06±11.21 (range, 27–76) years old. Preoperative average nodule size is 1.61±0.67 (range, 0.8–3.5) cm. The patients’ characteristics in both groups are described in Table 2. There were no significant differences in terms of patient age, sex or pulmonary nodule size. But in intercostal group, mean nodule size was larger (P>0.05).
Surgical results
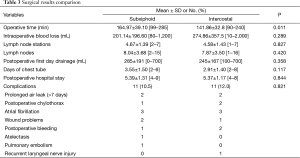
The total operative time was 164.97±39.10 (range, 99–285) min, and the volume of blood loss was 201.14±196.60 (range, 80–1,200) mL. Two patients required conversion to thoracotomy during surgery, due to the intra-operative vessels rupture and hemorrhage. One or two more incisions were adopted in six patients, among whom two cases were due to severe cardiac compression during left side resection, and four cases were due to the extensive pleural adhesion during operation.
When the patients returned to the postoperative care ward, in the subxiphoid group, pleural drainage was 285±191 (range, 0–700) mL on the first day after operation, and the tube was removed 3.55±1.50 (range, 2–9) days after operation. Chest X-ray revealed good pulmonary reexpansion in all patients expect one atelectasis case. No major laboratory abnormalities were found postoperatively. Of the 105 cases, 11 patients suffered from postoperative complications (10.5%), and the details are described in Table 3. All the105 patients were discharged on 5.39±1.31 (range, 4–9) days after operation. No postoperative mortality occurred.
Full table
The comparison of surgical results between two groups is described in Table 3.
Pain score
Pain was evaluated with the post-operative pain score (from 0 to 10 with 0 denoting no pain, and 10 indicating the worst pain ever experienced). Pain was evaluated postoperatively at 8 h, day 1, 2, and 3 and the day before discharge. The pain conditions were compared between two groups. The results are described in Table 4. The postoperative pain was primarily located around the subxiphoid area for patients undergoing subxiphoid surgeries.

Full table
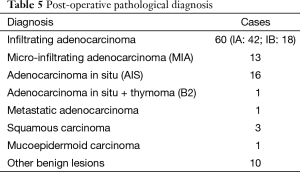
Postoperative pathology
Postoperative pathological results are shown in Table 5. A total of 77 patients with primary lung carcinoma (except adenocarcinoma in situ, AIS) underwent lymph node dissection, and 4.67±1.39 (range, 2–7) stations and 8.04±3.68 (range, 2–15) lymph nodes were dissected. Among them, 69 underwent lymph nodes dissection of the 7th station of lymph nodes. No metastatic lymph nodes were seen in postoperative pathology.
Full table
Discussion
The subxiphoid approach was applied in the expanded excision of thymus in treating myasthenia gravis early on (3). Subxiphoid incision and intercostal incisions were applied in bilateral lung metastasis tumor resections (4). Hence, the subxiphoid approach had already been used in thoracic surgery. The uniportal thoracoscopic surgery was first put forward by Gonzalez-Rivas et al. (5), and widely applied in the thoracic field in recent years, with satisfactory efficacy. On the basis of the two previous techniques, the subxiphoid uniportal VATS lobectomy was an innovation modification of VATS.
Since September 2013, we have successfully finished over 300 intercostal uniportal VATS lobectomies and segmentectomies, and we are fully experienced in uniportal VATS lobectomy. On the basis of our previous experience, we chose patients for subxiphoid VATS. The subxiphoid surgery was more difficult compared with the intercostal uniportal VATS due to the longer subcutaneous tunnel, longer distance to the upper and lower hilus of the lung, smaller operative angle and more instrument mutual interference. To solve these, we tried to reduce the number of instruments used in surgery. Generally only two instruments and one thoracoscope lens were used in the surgery. Meanwhile the instruments must be long and thin, better angled, which was convenient for operation. As for the operation procedure, on the occasion that fissure did not develop well, it was quite difficult to open the fissure with ‘tunnel’ method, so usually the operational sequence was vein-bronchus-fissure with artery, and the fissure was left until last. In the early period, four patients received 1 extra 3 cm incision on lateral chest wall for extensive pleural adhesion; while with the increased experience, subxiphoid uniportal incision could handle almost all occasions except those with very severe extensive pleural adhesion. As the subxiphoid incision was much closer to the diaphragm and the costophrenic angle, it was more convenient for separation of the difficult adhesion of diaphragm and anterior-posterior costophrenic angle compared with that of intercostal uniportal incision. Hence pleural adhesion was not a contraindication for the subxiphoid uniportal incision procedure.
In the early period, two patients who received subxiphoid left lobectomy were converted into intercostal uniportal VATS lobectomy for severe obstruction of heart to instruments and lens. We improved this situation through lowering and left shifting the subxiphoid incision. Afterwards, we lowered and left shifted the incision alongside the left costal arch margin for left side lobectomy, which made the instruments enter through the left margin of heart and reduced the compression to heart, hence the risk and difficulty of surgery were reduced. In the early period we used the subxiphoid longitudinal incision in one patient. Afterwards, through comparison, we found that the field of vision was better with the oblique incision alongside the costal arch and transverse arch, and through which the instruments and lens could enter the pleural cavity more conveniently. Hence, we suggest oblique incision for unilateral operation and transverse incision for bilateral operations in the subxiphoid uniportal VATS.
The field of vision was limited in the subxiphoid incision, so it’s harder for hemostatic operation than in the regular operation. Once rupture of greater vessels and hemorrhage occur during the operation and preliminary hemostatic operation does not achieve hemostasis, we suggest compression of the bleeding sites with gauze pliers, and convert to thoracotomy as soon as possible. Two patients in our group were transitioned to thoracotomy due to pulmonary arterial hemorrhage, and no alteration in positioning was required. The surgeon could approach into chest through the 4th intercostal anterolateral incision quickly, and the 4th rib could be cut down when necessary. Therefore the hemorrhage could be easily controlled. Hence, even though the operative difficulty index was quite high, we still considered the subxiphoid uniportal VATS lung resection to be safe.
Liu et al. reported that systemic lymph node dissection through the subxiphoid incision was difficult, and the one case reported only received mediastinal lymph node sampling (2). In our group, 77 patients with primary lung carcinoma underwent mediastinal lymph node sampling or dissection (4.67±1.39 group, 8.04±3.68 lymph nodes), but those with benign and AIS intra-operative frozen results did not undergo lymph nodes sampling or dissection. There were no significant differences in lymph nodes dissection between subxiphoid and intercostal groups (stations or nodes, Table 3). Our experience was that although the field of was not adequate in the subxiphoid uniportal VATS, systemic lymph node dissection, including the lymph nodes of the left group 4L, 5, 6, 7, 8, 9, 10, 11 and the right group 2, 3a, 4R, 7, 8, 9, 10, 11, could be performed through appropriate traction of lung and the coordinated reversal of the operation bed. Given our limited experience with this procedure, we chose the patients who needed the lobectomy with solid nodes or ground-grass nodes with the diameter less than 2 cm and no concurrent enlarged hilar or mediastinal lymph nodes, and no lymph node dissection after a negative selective sampling was performed. Later on, with increased experience, the progression of technique and the improvement of instruments, we could complete the mediastinal and hilar lymph node dissection, and the operative indication range could be further enlarged to the same as for uniportal VATS lobectomy.
In subxiphoid group, operative time was statistically longer (P<0.05, Table 3). We consider the reason is the early subxiphoid procedures always cost too much time. We expect the operative time will get shorter and be stable with the accumulation of cases. Except this, there were no significant differences in terms of blood loss, drainage, days of chest tube, postoperative hospital stay or complications. So, we think subxiphoid uniportal VATS lobectomy is as safe and effective as intercostal procedure for pulmonary nodule.
It has been reported that the incidence of post-operative incision pain was 11–80% in thoracic patients, and the post-operative pain incidence of the traditional intercostal incisive thoracoscopic surgery was not different from thoracotomy (6). The post-operative pain was mainly due to the damage of intercostal nerve during operation. There was no bone structure or intercostal nerve in the subxiphoid incision, so the post-operative pain of this approach was significantly less than that of the regular surgery (according to the patients’ chief complain). The average pain scores on day 1, 2 and 3 after surgery, and the day before discharge were 2.39±0.99, 2.06±0.85, 1.68±0.87, 1.29±0.78 and 0.48±0.51, respectively, which were significantly lower than those of the control group (intercostal uniportal VATS) (P<0.001), indicating that the pain was relieved compared with the regular intercostal incision. This approach might solve the post-operative chronic persistent pain caused by the intercostal incision, but more studies are still required to confirm this.
In the subxiphoid incision, the surgeon could approach bilateral pleural cavities through subcutaneous tunnel, which made the operation suitable for patients with bilateral lung lesions. Nine patients in our study underwent subxiphoid bilateral lung operations with only single-portal subxiphoid incision, and bilateral lung operations could be performed simultaneously. Moreover, no intra-operative alteration of position was needed, the operative time and anesthetic time was shortened when compared with the regular bilateral operation, and the operative trauma was reduced. This operation is very convenient for bilateral lung bulla resection to treat bilateral pneumothorax patients. We have already performed several cases.
Conclusions
The subxiphoid uniportal VATS lobectomy is quite technically difficult, so it should be performed by experienced thoracic uniportal VATS surgeons in appropriate patients. It is very safe and especially suitable for the bilateral lung lesions. Mediastinal lymph node dissection could be completed after lung cancer resection. It significantly relieves the post-operative incision pain when compared with the intercostal uniportal VATS.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg 2010;139:366-78. [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [PubMed]
- Hsu CP, Chuang CY, Hsu NY, et al. Subxiphoid approach for video-assisted thoracoscopic extended thymectomy in treating myasthenia gravis. Interact Cardiovasc Thorac Surg 2002;1:4-8. [PubMed]
- Taniguchi Y, Suzuki Y, Suda T, et al. Video-assisted thoracoscopic bilateral lung metastasectomy with a subxiphoid access port. J Thorac Cardiovasc Surg 2005;130:916-7. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Rogers ML, Duffy JP. Surgical aspects of chronic post-thoracotomy pain. Eur J Cardiothorac Surg 2000;18:711-6. [PubMed]



