Nuss bar removal without straightening is a safe technique: a single center experience
Introduction
The minimally invasive Nuss procedure is currently the preferred surgical approach for treatment of pectus excavatum. During this procedure, a retrosternal bar is inserted which instantly corrects the deformity. The bar typically remains in place for 2 to 3 years, during which time the chest is considered to have adopted its new shape. Removal of the bar is generally considered to be a nondemanding procedure. Notwithstanding, it is associated with rare but potentially life-threatening complications such as bleeding from the pericardium, heart, and internal thoracic vessels when the bar is removed from its substernal tunnel (1-8).
An online survey among 112 surgeons affiliated to the Chest Wall International Group (CWIG) observed that straightening of the bar before removal in conjunction with bilateral opening of the previous surgical incisions is the most popular approach (9). This observation is reinforced by a recent systematic review by Haecker and colleagues (10) who correspondingly advocate for bilateral opening of the surgical incisions, straightening of the bar as well as meticulous bar mobilization based on three large cohort studies (2,11,12). However, these safety measures introduce increased surgical trauma. In our center, Nuss bar removal is performed without straightening, removing the bar along the thoracic curvature, preferably using only one incision. We hypothesize that this approach without straightening the bar reduces surgical trauma during removal and is safe in terms of perioperative complications. The aim of this retrospective study is to report our single-center experience with emphasis on perioperative complications after bar removal, using our alternative approach. Secondary outcomes included operation duration, blood loss, and length of postoperative hospital stay. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-725/rc) (13).
Methods
Study design and setting
A single-center retrospective study was conducted at Zuyderland Medical Centre, Heerlen, The Netherlands. The study was approved by the local ethics committee of Zuyderland Medical Center, Heerlen, The Netherlands (registration number: METCZ20210073; date of approval: April 15th, 2021) and conducted in accordance with the Declaration of Helsinki (as revised in 2013). The need for individual patient consent for this retrospective analysis was waived.
Participants
All consecutive patients undergoing bar removal between May 2011 and September 2020 at our institution were eligible for inclusion. No age restrictions were imposed. Patients who underwent additional surgical corrections (e.g., the Ravitch procedure or costal cartilage resection) after removal during the same surgical session were excluded.
Variables and data analysis
Clinical data and endpoints of removal procedures were extracted from the electronic patient files by a single researcher. A second researcher validated the data.
The following data was extracted: (I) patient characteristics [age, sex, body mass index (BMI)], baseline Haller index (i.e., Haller index prior to the Nuss repair) and the time between the insertion and removal; (II) procedural characteristics (number of bars, number of incisions, number of stabilizers, position of the stabilizers and their fixation method, duration of the removal procedure, as well as its blood loss, perioperative complications, and the postoperative length of hospital stay).
The primary outcome measure was the incidence of perioperative complications. Complications were classified using the definitions and time windows as defined in our previous report on the learning curve of the Nuss procedure (14). See Table S1 for further specification. Complications were graded according to the Clavien-Dindo classification (CDC) (15). Major complications were defined as those with a CDC larger than or equal to IIIa. Those with a CDC lower than III were defined as minor.
Secondary outcomes included duration of operation, blood loss, and length of postoperative hospital stay.
Statistical analyses
Statistical analyses were performed using SPSS for Mac OS software version 27.0 (IBM Corp, Armonk, NY, USA). Continuous data was reported as mean and standard deviation (SD) or median and interquartile range (IQR) in the presence of skewness. Categorical variables were denoted as frequencies and percentages. Missing data was reported as such.
Surgical technique
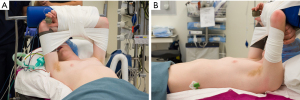
The patient is placed in the dorsal decubitus position, aligned on the far-left side of the table to allow removal without prior straightening of the bar (Figure 1). The procedure is performed under general anesthesia using single-lumen endotracheal intubation. Cefazoline is administered prophylactically. After draping, an incision is made along the prior left-sided surgical scar. In the presence of bilateral stabilizers incisions are made on both sides. In the case of unilateral stabilizer(s), the contralateral incision is only opened in the presence of extensive callus formation preventing bar mobilization. The bar is identified and dissected using electrocautery and the stabilizer(s) removed. We use the short symmetric universal pectus bar (Medxpert GmbH, Eschbach, Germany) with mild bending as introduced by Pilegaard for pectus excavatum repair (16). Over time, the stabilizers’ fixation method has been subject to change. The most recent generation is fixed onto the bar with a single screw. Prior, wire cerclages (until late 2017), FiberWire (Arthrex, Naples, Fla; until late 2018) and Hi-Fi sutures (CONMED, Utica, NY, USA; until 2019) were utilized. Extensive ossification is removed by using an osteotome. A bone hook is attached to the bar’s end to extract the bar in one smooth movement along the natural (convex) curvature of the thorax without prior straightening of the bar (Figure 2). If too much force is required for bar removal and/or or any tissue resistance is present, then a contralateral incision is made. Additional bars are removed in similar fashion. After hemostasis, the incisions are closed in a three-layered fashion with absorbable sutures. No chest tubes or wound catheters are left, nor is de-airing of the thoracic cavity performed. A chest X-ray was performed routinely after surgery. Patients were usually discharged on the first operative day, provided adequate mobilization and pain control. Since 2017 patients who undergo such a removal procedure enter a standard follow-up program of 1 year. Between 2011 and 2017, these patients only visited our outpatient clinic on indication.

Results
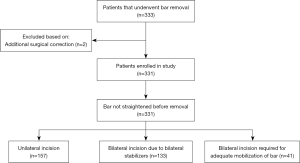
Between May 2011 and September 2020, 333 patients underwent Nuss bar removal at our institution (Figure 3). Two patients were excluded because a Ravitch procedure was performed in the same surgical session as the bar removal.
A total of 331 patients were enrolled. Patient and procedural characteristics and are summarized in Table 1. Most patients were male (n=288, 87%). Patients had a median age of 20 years (IQR, 19–26 years) at the time of bar removal. Bar removal was performed at a median of 3.1 years (IQR, 2.9–3.4 years) after insertion. Bilateral stabilizers were implanted in 133 patients (40%), requiring bilateral incisions. Bilateral incisions were necessary in 41 (12%) patients to allow for bar mobilization. Thus, in 41/198 (21%) patients with only one stabilizer, bilateral incisions were necessary.
Table 1
| Variables | Patients | Missing data |
|---|---|---|
| Total number of patients | 331 | |
| Gender, n [%] | 0 | |
| Male | 288 [87] | |
| Age at removal, years, median [IQR] | 20 [19–26] | 0 |
| BMI, kg/m2, median [IQR] | 21 [20–23] | 4 |
| Baseline Haller index, median [IQR] | 3.5 [3.0–4.0] | 51 |
| Number of bars, n [%] | 0 | |
| 1 | 317 [96] | |
| 2 | 14 [4] | |
| Bar time, years, median [IQR] | 3.1 [2.9–3.4] | 10 |
| Stabilizers, n [%] | 0 | |
| Left side only | 190 [57] | |
| Right side only | 8 [3] | |
| Both sides | 133 [40] | |
| Incisions, n [%] | 0 | |
| Unilateral | 157 [48] | |
| Bilateral due to presence of bilateral stabilizers | 133 [40] | |
| Bilateral required for bar mobilization | 41 [12] | |
| Duration of surgical procedure, min, median [IQR] | 30 [20–40] | 7 |
| Blood loss, mL, median [IQR] | 5 [5–10] | 1 |
| Postoperative hospital stay, days, median [IQR] | 1 [1–1] | 0 |
IQR, interquartile range; BMI, body mass index; n, number; mL, milliliters; min, minutes.
Complications
Four complications associated with removal occurred in a total of 4 patients (1%, CDC II–IV), outlined in Table 2. Of these, two were graded as major (0.6%), including one deep incisional surgical site infection requiring surgical drainage and a bleeding from an intercostal artery requiring immediate reoperation with video-assisted thoracoscopic surgery (VATS) and transfer to the intensive care unit for monitoring. The other complications concerned two superficial surgical site infections for which antibiotic treatment was given. In the patient with the intercostal artery bleeding, the bar was removed via a unilateral incision, whilst in the other patients a bilateral incision was performed. The intercostal bleeding occurred on the side where the incision was reopened. In all patients with a surgical site infection, severe ossification was observed perioperative, which was handled by removal of the ossification with an osteotome. One patient of the patients with a superficial surgical site infection already had a low-grade infection before the removal procedure was started and antibiotics were therefore prescribed directly postoperative for that patient. All patients with a complication recovered fully.
Table 2
| Variables | Patient 1 | Patient 2 | Patient 3 | Patient 4 |
|---|---|---|---|---|
| Age, years | 40 | 37 | 22 | 22 |
| Gender | Male | Male | Male | Male |
| Bar time, days | 2,544 | 1,099 | 981 | 1,140 |
| Complication | Superficial incisional SSI | Superficial incisional SSI | Deep incisional SSI | Hemothorax |
| CDC | II | II | IIIb | IV |
| Days post-surgery | 14 | 21 | 11 | 0 |
| Number of bars | 1 | 1 | 1 | 1 |
| Number of stabilizers | 2 | 2 | 1 | 1 |
| Number of incisions | Bilateral | Bilateral | Bilateral | Unilateral |
| Operative time, min | 50 | 52 | 40 | 26 |
SSI, surgical-site infection; CDC, Clavien-Dindo classification; min, minutes.
Secondary outcomes
The median operation time was 30 minutes (IQR, 20–40 minutes; Table 1) with a median blood loss of 5 mL (IQR, 5–10 mL). Most patients were discharged 1 day (median: 1 day; IQR, 1–1 day) after removal.
Discussion
Elective bar removal after the Nuss procedure is associated with rare but life-threatening complications. Current evidence advocates for intraoperative straightening of the bar to prevent occurrence of such complications (9,10), though this requires additional surgical trauma. This study reports on the outcomes after bar removal without prior straightening of the bar. This technique is, in our experience, associated with a relatively low complication rate of 1% (n=4), of which only 2 (0.6%) were considered as major complications requiring surgical intervention. No mortality was reported. This relatively low complication rate suggests that straightening of the Nuss bar is not necessary to increase safety of the procedure.
Several techniques and maneuvers for removal of the bar have been described so far (1-8,17). Our method of removal consists of extraction along the thoracic curvature without prior straightening while the patient is positioned in the dorsal decubitus position on the far-left side of the operating table. Alternative techniques avoiding readjustment of the form of the bar have been reported before. Nuss et al. (18) describe a procedure whereby the patient is positioned in the lateral decubitus position to allow removal of the bar along the curvature of the thorax. St Peter et al. (7) and Fike et al. (8) recommend use of two operation tables with a gap in between such that the bar can be removed along the curvature of the thorax regardless of the bar’s length. In both studies bilateral incisions were performed. Chon and Shinn (1) likewise remove the bar without prior straightening while placing the patient in the following position: they placed their patients in the prone Mohammedan prayer position with flexed knees, abducted arms, and upward tilted head. In order to facilitate bar extraction without prior straightening shorter bars have been advocated by Nyboe et al. and Liu et al. (19,20) as also used in the present study.
Potentially, removal of the curved bar can cause additional surgical trauma such as muscle stripping and pleural defects at the hinge points. This subsequently may increase the risk for development of pneumothoraces and bleeding. Park et al. (21), reported their results on bar removal without prior straightening and observed one hemothorax, one intercostal artery bleeding (requiring intervention) and no pneumothoraxes in their sample of 1,821 patients. In addition, Kelly et al. (22) observed three pneumothoraxes requiring intervention in their 854-patient sample. Hsieh et al. (17) report their institutional experience with partially unbending the bar. They reopen both incisions, but only unbend the right side of the bar. In their sample of 283 patients, six pneumothoraces (2%), three hematomas (1%), but no major bleedings were observed.
In our study we report no significant pneumothoraces and only one intercostal artery bleeding requiring intervention. Moreover, the intercostal artery bleeding occurred on the side where the incision was reopened. Small pneumothoraces were observed as chest X-rays were routinely made postoperatively. However, they were of no clinical relevance. This is in line with the study samples of Liu et al. (20) and St Peter et al. (7) who both describe no significant complications requiring intervention, and Fike et al. (8) who report only one bleeding requiring blood transfusion (0.4%). Though, Nyboe et al. (19) who likewise performed removal without unbending describe relatively higher complication rates; 4 complications (1%) in their cohort of 343 patients. This concerned three postoperative pneumothoraces and one hemothorax which required intervention.
In 4 out of 5 patients with a unilateral stabilizer, reopening only the ipsilateral incision sufficed. Therefore in 79% of these patients a second incision could be prevented. This may have contributed to the low incidence of surgical site infections in the present study (0.9%) which is comparable to or lower than in series with bilateral incisions [St Peter et al. (7), 0%; Kelly et al. (22), 0.1%; Park et al. (21), 2%; Fike et al. (8), 3%].
An online survey among members of the CWIG reported that most surgeons prefer bilateral incisions and straightening of the bar (9). However, our study strengthens the evidence that removal without straightening of the bar is a safe technique and is at least non-inferior to bilateral incisions and straightening of the bar in terms of complication rates. This holds also true for the secondary outcome measures (i.e., procedural duration, blood loss and hospital stay) (3,17,21,22) although length of stay is strongly influenced by local discharge criteria.
When looking at the characteristics of our patient sample, it is important to note that 96% of patients had one bar implanted during the initial procedure, which is relatively high compared to other series. For example, 84% in the study by Nyboe et al. (19) and 69% in the study by Kelly et al. (22) Nevertheless, we also observed a trend towards multi-bar placement over time. This was also noted by Kelly et al. (22) for their study sample [88% had one bar in their cohort before 2001 as reported by Croitoru et al. (23)].
The median preoperative Haller index of our study sample was 3.5 (IQR, 3.0–4.0), while other series report a higher preoperative Haller index in their patient sample [Kelly et al. (22), 5.2 (SD 2.3); Kuyama and colleagues (24), 5.1 (SD 1.5); Kuru et al. (25), 4.0 (SD 1.3), respectively]. Our series did thus contain less severe cases of pectus excavatum, which possibly affects the external applicability of the study.
In the current study all patients were routinely discharged the day after removal surgery as part of our local policy. However, same day discharge is possible without major risks based on current literature and aim to introduce this soon.
The main limitation of this study is its retrospective and single-center design. Some of the missing data (i.e., baseline Haller index and bar in situ period) can be explained by that bar insertion procedure was performed at a different institution. However, those patients were randomly distributed throughout the sample.
Moreover, the lack of a standard follow-up period during the early experience could cause an underestimation of the actual rate of postoperative complications. In addition, although our results indicate that omission of straightening of the Nuss bar prior to extraction is safe and non-inferior, ideally this would be confirmed in an adequately powered randomized controlled trial. However, because of the low incidence rates of postoperative complications this would require very large number of patients.
Conclusions
Removal of the Nuss bar along the thoracic curvature without in-situ straightening of the bar is a safe procedure in terms of perioperative complications.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-725/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-725/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-725/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the local ethics committee of Zuyderland Medical Center, Heerlen, The Netherlands (registration number: METCZ20210073; date of approval: April 15th, 2021) and conducted in accordance with the Declaration of Helsinki (as revised in 2013). The need for individual patient consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chon SH, Shinn SH. A simple method of substernal bar removal after the Nuss procedure. Eur J Cardiothorac Surg 2011;40:e130-1. [Crossref] [PubMed]
- Bilgi Z, Ermerak NO, Laçin T, et al. Previously Complicated Nuss Procedure Does Not Preclude Blind Removal of the Bar. Thorac Cardiovasc Surg 2016;64:83-6. [PubMed]
- Varela P, Romanini MV, Asquasciati C, et al. A simple technique for removing the Nuss bar with one stabilizer: the lateral approach. J Laparoendosc Adv Surg Tech A 2010;20:91-3. [Crossref] [PubMed]
- de Campos JR, Das-Neves-Pereira JC, Lopes KM, et al. Technical modifications in stabilisers and in bar removal in the Nuss procedure. Eur J Cardiothorac Surg 2009;36:410-2. [Crossref] [PubMed]
- Toselli L, Bellía Munzón G, Martinez J, et al. Safety-string: A handy maneuver to control pectus bar removal bleeding complications. J Pediatr Surg 2020;55:1162-4. [Crossref] [PubMed]
- Kanegaonkar RG, Dussek JE. Removal of migrating pectus bars by video-assisted thoracoscopy. Eur J Cardiothorac Surg 2001;19:713-5. [Crossref] [PubMed]
- St Peter SD, Sharp RJ, Upadhyaya P, et al. A straightforward technique for removal of the substernal bar after the Nuss operation. J Pediatr Surg 2007;42:1789-91. [Crossref] [PubMed]
- Fike FB, Mortellaro VE, Iqbal CW, et al. Experience with a simple technique for pectus bar removal. J Pediatr Surg 2012;47:490-3. [Crossref] [PubMed]
- Alvarez-Garcia N, Ardigo L, Bellia-Munzon G, et al. Close Examination of the Bar Removal Procedure: The Surgeons’ Voice. Eur J Pediatr Surg 2018;28:406-12. [Crossref] [PubMed]
- Haecker FM, Hebra A, Ferro MM. Pectus bar removal - why, when, where and how. J Pediatr Surg 2021;56:540-4. [Crossref] [PubMed]
- Nuss D, Obermeyer RJ, Kelly RE. Pectus excavatum from a pediatric surgeon’s perspective. Ann Cardiothorac Surg 2016;5:493-500. [Crossref] [PubMed]
- Noguchi M, Fujita K. A new technique for removing the pectus bar used in the Nuss procedure. J Pediatr Surg 2005;40:674-7. [Crossref] [PubMed]
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495-9. [Crossref] [PubMed]
- de Loos ER, Daemen JHT, Pennings AJ, et al. Minimally invasive repair of pectus excavatum by the Nuss procedure: The learning curve. J Thorac Cardiovasc Surg 2022;163:828-837.e4. [Crossref] [PubMed]
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Pilegaard HK. Short Nuss bar procedure. Ann Cardiothorac Surg 2016;5:513-8. [Crossref] [PubMed]
- Hsieh MS, Tong SS, Wei BC, et al. Minimization of the complications associated with bar removal after the Nuss procedure in adults. J Cardiothorac Surg 2020;15:65. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Nyboe C, Knudsen MR, Pilegaard HK. Elective pectus bar removal following Nuss procedure for pectus excavatum: a single-institution experience. Eur J Cardiothorac Surg 2011;39:1040-2. [Crossref] [PubMed]
- Liu W, Kong D, Yu F, et al. Clinical analysis of modified technique for pectus bar removal after Nuss procedure. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2013;38:274-8. [PubMed]
- Park HJ, Kim KS. Pectus bar removal: surgical technique and strategy to avoid complications. J Vis Surg 2016;2:60. [Crossref] [PubMed]
- Kelly RE, Goretsky MJ, Obermeyer R, et al. Twenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patients. Ann Surg 2010;252:1072-81. [Crossref] [PubMed]
- Croitoru DP, Kelly RE Jr, Goretsky MJ, et al. Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients. J Pediatr Surg 2002;37:437-45. [Crossref] [PubMed]
- Kuyama H, Uemura S, Yoshida A. Recurrence of pectus excavatum in long-term follow-up after the Nuss procedure in young children based on the radiographic Haller index. J Pediatr Surg 2020;55:2699-702. [Crossref] [PubMed]
- Kuru P, Bostanci K, Ermerak NO, et al. Quality of life improves after minimally invasive repair of pectus excavatum. Asian Cardiovasc Thorac Ann 2015;23:302-7. [Crossref] [PubMed]