
A multicenter survey on the current status of chronic cough and its impact on quality of life in Guangdong, China
Introduction
Cough is the most frequent complaint for patients who seek medical attention in primary and secondary health care (1). Chronic cough, defined as a cough lasting longer than 8 weeks, affects approximately 10% of the general population around the world (2). Owing to a lack of other respiratory symptoms and normal chest X-ray, chronic cough is usually underrecognized by clinicians (3). A few international and national respiratory societies have successively published guidelines on the diagnosis and management of chronic cough over the past decades (4-10), suggesting the importance of chronic cough as a clinical entity. Chinese guidelines on the diagnosis and management of cough were initially released in 2005 (10), and subsequently updated in 2009 (11) and 2015 (12). A growing number of physicians in large general hospitals have recognized the common etiologies of chronic cough, such as cough variant asthma (CVA), upper airway cough syndrome (UACS), eosinophilic bronchitis (EB), gastroesophageal reflux cough (GERC) and atopic cough (AC) (13). However, as a developing country, China has great variations in medical and healthcare resources across different regions. Hence, the current status and disease burden of chronic cough require better understanding in China.
Accumulating evidence suggests that chronic cough is associated with repeated doctor visits and medications use, leading to substantial economic burden on the family (14-17). In addition, chronic cough can significantly impair health-related quality of life and have more serious effects on women (17,18). However, several studies conducted in China found no difference in the impact of cough between sexes (19-22). Of note, these studies were mainly conducted in a single center with limited samples (18-22). Therefore, this study aimed to investigate the current status of the diagnosis and treatment of chronic cough and its impact on quality of life in Guangdong, south China. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1737/rc).
Methods
Study design and participants
We conducted a cross-sectional observational survey in the respiratory clinics of thirteen tertiary medical centers of Guangdong Province (south China), at which physicians had been trained and understood the diagnosis and treatment of chronic cough. Consecutive and unselected patients attending clinics for chronic cough were invited to participate in this survey from August 2017 to August 2018. Details of the study protocol have been described previously (23). Briefly, patients were enrolled if they had an isolated chronic cough (>8 weeks), no overt lung abnormalities, and an age of 15 years or more. The exclusion criteria included obvious dyspnea or wheezing, concomitant severe systemic diseases, as well as inability to fill out the questionnaire.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (No. 201778), and written informed consent was obtained from all participants prior to study.
Questionnaire
All participants completed a standardized questionnaire. We extracted and analyzed the data on demographics and medical history, including age, sex, cough duration, smoking history, number of visits to a doctor, previous diagnosis, previous medications and initial diagnosis.
The definition of previous diagnosis was a diagnosis that had been made at any previous visit due to chronic cough. The previous medications were defined as any drugs used by asking a question “Have you ever used the following medications for chronic cough, such as antitussives, antibiotics, traditional Chinese medicine (TCM), anti-allergic medications, inhaled corticosteroids (ICS), oral corticosteroids (OCS) or antireflux medications?”. The initial diagnosis was defined as a diagnosis given at this visit according to the medical history and response to past treatment. Of these, asthmatic cough was diagnosed if a patient presented with bronchial hyperresponsiveness to methacholine and well responded to antiasthmatic therapy, including CVA and cough predominant asthma (CPA) (24). A slight difference of clinical manifestations was shown between these two disorders, cough as an isolated symptom (no wheeze and dyspnea) in CVA and cough as a predominant symptom (occasionally wheeze and dyspnea) in CPA.
The Mandarin Chinese version of the Leicester Cough Questionnaire (LCQ-MC) was used to evaluate the impact of cough on the patients’ quality of life (25,26). The questionnaire consisted of 19 cough-specific items divided into three subscales (physical, psychological and social) and utilized a seven-point Likert response scale. Scores for each subscale ranged from 1 to 7 and the overall score ranged from 3 to 21, with a higher score indicating better quality of life.
Statistical analysis
SPSS statistical software version 22.0 (SPSS Inc., Chicago, IL, USA) was used for all data analysis. Continuous variables were expressed as median and interquartile range (IQR), whilst categorical variables were presented as numbers and proportions. Wilcoxon rank-sum tests were carried out to compare the LCQ-MC scores between the two groups (sexes and number of visits to a doctor more than three times or not), while Kruskal-Wallis test was applied in the comparison of the LCQ-MC scores among the three domains (physical, psychological and social). P value <0.05 was considered as statistically significant.
Results
Demographics
A total of 1,384 patients with cough were screened, and 933 (67.4%) met the criteria and were included in this study. The patient numbers and reasons for exclusion have been previously reported (23). The median age of the patients was 40.0 (IQR, 31.0–52.0) years, with 52.2% of them being female (Table 1). They had a median cough duration of 6.0 (IQR, 3.0–24.0) months. The majority were never/ex-smokers, accounting for 87.8% of the study population.
Table 1
| Characteristics | Values |
|---|---|
| Participants | 933 |
| Age, years | 40.0 (31.0–52.0) |
| Female | 487 (52.2%) |
| Cough duration, months | 6.0 (3.0–24.0) |
| Current smokers | 114 (12.2%) |
| Never/former smokers | 819 (87.8%) |
Data were expressed as median (IQR), number (%) or number. IQR, interquartile range.
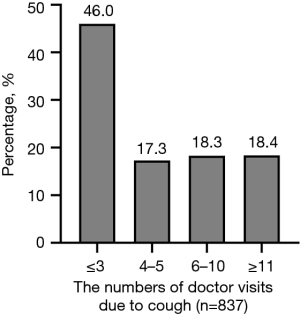
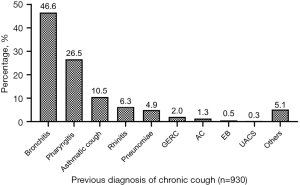
Previous diagnosis and medications
Over half (n=452, 54.0%) of the patients had sought medical service for cough more than three times (Figure 1). Surprisingly, the proportion of patients experiencing >10 doctor visits was 18.4%. In terms of previous diagnosis, 433 (46.6%) patients had been diagnosed with bronchitis, followed by pharyngitis (n=246, 26.5%) and asthmatic cough (n=98, 10.5%) (Figure 2).
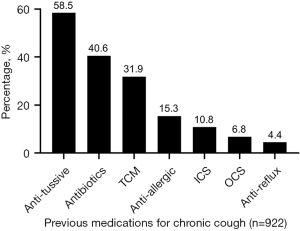
Some sort of treatment had been usually prescribed against chronic cough by clinicians in primary and secondary care prior to this visit. As shown in Figure 3, 539 (58.5%) out of 922 patients (with data) reported the use of antitussive agents, 374 (40.6%) used antibiotics, and 294 (31.9%) used TCM. Nevertheless, only 17.6% of the cases had ever received ICS or OCS, and 4.4% received antireflux therapy (acid suppression or promotility agents).
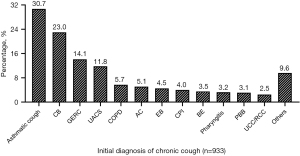
Initial diagnosis
Of the 933 patients, dual causes were identified in 78 (8.4%) patients and triple causes were identified in 20 (2.1%) patients at the initial visit. A total of 286 (30.7%) patients were initially diagnosed with asthmatic cough, 215 (23.0%) with chronic bronchitis (CB), 132 (14.1%) with GERC, and 110 (11.8%) with UACS (Figure 4). However, a minority of patients were considered having AC (n=48, 5.1%) or EB (n=42, 4.5%).
Impact of chronic cough
Complete information from the LCQ-MC was available in 809 (86.7%) of 933 patients with chronic cough. The majority complained of cough-related physical symptoms, such as sleep disturbance (n=247, 30.5%), fatigue (n=235, 29.0%), and sputum production (n=230, 28.4%) (Table 2). Besides, commonly described associated psychological effects included anxiety (n=287, 35.5%), embarrassment (n=272, 33.6%) and frustration (n=192, 23.7%), which more frequently occurred in women and patients who visited to the doctor more than three times (all P<0.05). Nearly one-third (n=251, 31.0%) of chronic coughers felt that cough interfered with their daily work.
Table 2
| Item | Total (n=809) | Gender | Number of visits to the doctor | |||
|---|---|---|---|---|---|---|
| Male (n=384) | Female (n=425) | ≤3 (n=375) | >3 (n=430) | |||
| Chest or stomach pains, n (%) | 72 (8.9) | 29 (7.6) | 43 (10.1) | 28 (7.5) | 41 (9.5) | |
| Phlegm, n (%) | 230 (28.4) | 95 (24.7)* | 135 (31.8) | 86 (22.9)# | 142 (33.0) | |
| Fatigue, n (%) | 235 (29.0) | 96 (25.0)* | 139 (32.7) | 87 (23.2)# | 146 (34.0) | |
| Unable to control their cough, n (%) | 484 (59.8) | 207 (53.9) | 277 (65.2) | 211 (56.3) | 269 (62.6) | |
| Embarrassment, n (%) | 272 (33.6) | 119 (31.0) | 153 (36.0) | 107 (28.5)# | 162 (37.7) | |
| Anxiety, n (%) | 287 (35.5) | 113 (29.4)* | 174 (40.9) | 110 (29.3)# | 175 (40.7) | |
| Interference with daily work, n (%) | 251 (31.0) | 100 (26.0)* | 151 (35.5) | 91 (24.3)# | 158 (36.7) | |
| Interference with overall enjoyment, n (%) | 247 (30.5) | 110 (28.6) | 137 (32.2) | 84 (22.4)# | 162 (37.7) | |
| Cough due to exposure to paints or fumes, n (%) | 284 (35.1) | 119 (31.0)* | 165 (38.8) | 120 (32.0) | 162 (37.7) | |
| Disturbance of sleep, n (%) | 247 (30.5) | 88 (22.9)* | 159 (37.4) | 100 (26.7)# | 145 (33.7) | |
| Coughing bouts, n (%) | 364 (45.0) | 153 (39.8)* | 211 (49.6) | 150 (40.0)# | 211 (49.1) | |
| Frustration, n (%) | 192 (23.7) | 62 (16.1)* | 130 (30.6) | 65 (17.3)# | 125 (29.1) | |
| Fed up, n (%) | 361 (44.6) | 157 (40.9)* | 204 (48.0) | 147 (39.2)# | 211 (49.1) | |
| Hoarse voice, n (%) | 155 (19.2) | 68 (17.7) | 87 (20.5) | 63 (16.8) | 91 (21.2) | |
| Lack of energy, n (%) | 253 (31.3) | 108 (28.1) | 145 (34.1) | 110 (29.3) | 141 (32.8) | |
| Worried about serious diseases, n (%) | 259 (32.0) | 104 (27.1)* | 155 (36.5) | 101 (26.9) | 157 (36.5) | |
| Concerned the other’s feelings about your cough, n (%) | 254 (31.4) | 112 (29.2) | 142 (33.4) | 97 (25.9) | 155 (36.0) | |
| Interrupted conversation or telephone calls, n (%) | 189 (23.4) | 71 (18.5)* | 118 (27.8) | 74 (19.7) | 114 (26.5) | |
| Annoying partners, family or friends, n (%) | 137 (16.9) | 56 (14.6) | 81 (19.1) | 55 (14.7) | 81 (18.8) | |
A score ≤3 points indicated a significant impact on individual patients (27). (%): ratios of the number of patients with score ≤3 points to the total number of patients completing the LCQ-MC in each group. *, male versus female, P<0.05; #, number of visits to the doctor: ≤3 times versus >3 times, P<0.05. LCQ-MC, Mandarin Chinese version of the Leicester Cough Questionnaire.
As outlined in Table 3, the median LCQ-MC total score was 13.2 (IQR, 10.7–15.5), with lower scores in the mental health domain than in the physical and social domains [median (IQR): 4.0 (3.1–4.9) versus 4.5 (3.8–5.3), 4.0 (3.1–4.9) versus 4.8 (3.8–5.5), respectively, both P<0.001]. Moreover, we also observed lower LCQ-MC scores in females and patients who saw the doctor >3 times for both the total and three subscale scores (all P<0.05).
Table 3
| LCQ-MC | Total (n=809) | Gender | Number of visits to the doctor | |||
|---|---|---|---|---|---|---|
| Male (n=384) | Female (n=425) | ≤3 (n=375) | >3 (n=430) | |||
| Physical | 4.5 (3.8–5.3)‡ | 4.8 (4.0–5.5)** | 4.4 (3.6–5.1) | 4.8 (4.0–5.4)# | 4.4 (3.6–5.1) | |
| Psychological | 4.0 (3.1–4.9)&† | 4.3 (3.3–5.3)** | 3.9 (2.9–4.7) | 4.3 (3.4–5.1)# | 3.9 (2.9–4.7) | |
| Social | 4.8 (3.8–5.5) | 5.0 (3.8–5.8)* | 4.5 (3.5–5.5) | 5.0 (4.0–5.8)# | 4.4 (3.3–5.5) | |
| Total | 13.2 (10.7–15.5) | 13.9 (11.4–16.2)** | 12.6 (10.3–14.9) | 14.0 (11.7–16.1)# | 12.6 (10.1–14.9) | |
Data were presented as median (IQR). ‡, physical versus social, P<0.05; **, male versus female, P<0.001; #, number of visits to the doctor: ≤3 times versus >3 times, P<0.001; &, psychological versus physical, P<0.001; †, psychological versus social, P<0.001; *, male versus female, P=0.001. LCQ-MC, Mandarin Chinese version of the Leicester Cough Questionnaire; IQR, interquartile range.
Discussion
Using data from a multicenter cross-sectional observational study conducted in Guangdong, we showed that the patients who visited the hospital for chronic cough had a substantially high rate of visiting other medical institutions and varying degrees of misdiagnosis, suggesting an unmet clinical need of chronic cough despite the publication of cough guidelines for ages (10). Additionally, we further confirmed that the majority of patients presenting with chronic cough experienced negative impacts on all aspects of quality of life. More importantly, we also demonstrated a more significant deterioration in quality of life in females. These results suggested that there is room for improvement in the management of chronic cough in China (28).
Our findings showed that, in accordance with a previous study performed in the cough specialist clinic of Guangzhou (14), most patients with chronic cough had been diagnosed with bronchitis or pharyngitis. Nevertheless, a nationwide study focusing on chronic cough-associated conditions in China found that isolated chronic cough was usually due to CVA, UACS, EB and AC, accounting for 75.2–87.6% of the cases across different regions of the country (13). Furthermore, similar common causes of chronic cough were reported in the United States and Europe as well (29). These observations implied that a significant proportion of individuals with chronic cough might be misdiagnosed as having bronchitis and pharyngitis. One principal reason may be that physicians do not recognize the common diseases in relation to chronic cough. The other possible explanation is the lack of objective diagnostic criteria for bronchitis and pharyngitis. For example, CB is defined as chronic cough and expectoration for at least 3 months per year for 2 consecutive years or more, when other potential causes of chronic productive cough are excluded (30). In other words, the difficult aspect of CB diagnosis is ruling out other respiratory or cardiac conditions associated with chronic productive cough. Chronic cough is usually considered CB merely based on clinical manifestations in clinical practice, but possible underlying diseases are not excluded.
In addition to an insufficient understanding of chronic cough, the limitations of medical facilities are likely to be another potential reason for misdiagnosis in both primary and secondary medical centers. Cough-related assessments, including 24-hour impedance-pH monitoring, bronchial challenge testing and differential cell counts of induced sputum, are unavailable in many medical centers (10). As a result, it is difficult to provide a specific diagnosis for patients with chronic cough. To address this problem, the Chinese Cough Guideline for Primary Care, published in 2019 by the Chinese Cough Coalition, recommended empiric treatment based upon the clinical characteristics of chronic cough in medical centers lacking cough-related investigations (31). It is necessary to deepen clinicians’ understanding of underlying medical conditions presenting with chronic cough, and facilitate the implementation of cough management guidelines in community-based healthcare.
Improper diagnosis results in a cascade of inadequate treatment that might not alleviate the cough symptom. Our results showed that a majority of patients had received antitussive agents (58.5%) and antibiotics (40.6%) for their cough. Previous studies found that antitussives were prescribed in 58.7–93.7% of patients with chronic cough and that antibiotics were prescribed in 69.0–91.6% (13,14). Most diseases causing chronic cough were not strongly associated with microbial infection, except for UACS secondary to bacterial sinusitis (32). Besides, anti-acid drugs, prokinetic agents and glucocorticoids were rarely used in our study population, reflecting a poor understanding of reflux-related cough and corticosteroid-responsive cough. In an internet-based survey on the impact of chronic cough conducted by the European Lung Foundation, up to 70% of chronic coughers had seen a doctor ≥3 times in relation to cough (15). A previous single-center survey in China showed that the average number of previous medical visits due to chronic cough was 20.8±30.0 (14). Likewise, over half of the patients had sought medical help at least 3 times in the present study. Surprisingly, approximately one-fifth of the patients saw a doctor 10 or more times. These data indicated that chronic coughers generally had disappointing responses to medications used to treat their cough (17), supporting the opinion that potential inappropriate treatment is very prevalent in the chronic cough population, especially antibiotic abuse (14).
With the dissemination and application of cough guidelines in large cities across China, there was an increasing awareness of chronic cough by physicians in large general hospitals (28). Our study revealed that the top 4 suspected diseases associated with chronic cough included asthmatic cough, CB, GERC and UACS. Given the previous survey on causes of chronic cough in China (13), CB is not one of the common causes of chronic cough. Therefore, we infer that correct diagnosis might not be achieved among some chronic coughers even in tertiary care settings.
Previous studies have shown that chronic cough markedly decreases patients’ quality of life (17,27). In the current study, the majority complained that chronic cough resulted in anxiety, embarrassment and frustration. In fact, cough-related physical events were easily noticed by physicians through the clinical history, whereas the psychosocial impact generally received inadequate attention (3). Moreover, when we looked at sex differences in cough-specific quality of life, we found much poorer LCQ-MC scores in females than males, as described by Zeiger et al. (17) and French et al. (18). In contrast with these observations, cough-associated impacts on daily living did not significantly differ between sexes in earlier studies performed in China (19-22), possibly due to the relatively small sample sizes. However, it is possible that women were more apt to develop stress urinary incontinence that provoked psychological issues such as being embarrassed, especially in elderly women (33). In addition, women were more susceptible to the impact of cough when cough lasted longer (34). It is worth noting that, as reported by Won et al. (33), no significant correlation between cough duration and quality of life was found in women. Also, a higher cough sensitivity in women might explain why chronic cough more adversely affected the quality of life of females than that of males (35). Altogether, many factors play an important role in the sex-related disparities in quality of life among chronic coughers.
To our knowledge, this is the first multicenter observational study investigating the current status and cough-specific quality of life aspects among the Chinese chronic cough population thus far. The main strength of our study is the use of a larger cohort of adults with chronic cough than those included in previous surveys conducted in China (19-22). We demonstrated that, as reported in Western countries (17,18), there was much more serious impairment of all aspects of quality of life in women with chronic cough. There were some limitations in this survey. First, our study was conducted only in local hospitals of Guangdong Province, which revealed the misdiagnosis and inappropriate treatment of chronic cough in south China. However, it remains unknown whether this phenomenon is more serious in other regions of the country due to the variation in medical level. Second, data on previous medications use and diagnosis were self-reported by patients, suggesting a potential possibility of recall bias. Third, the impact of cough on psychological issues was evaluated through several items of the LCQ-MC but not a validated anxiety or depression questionnaire. Consequently, the prevalence and severity of anxiety and depression are unclear in our study population. Last, the underlying mechanism by which women were more likely to suffer considerable impairment in quality of life was not explored in this study. Further study is needed to clarify this mechanism.
Conclusions
In summary, misdiagnosis and inappropriate treatment are very common in the chronic cough population. The significant impact of chronic cough on quality of life, especially for females, dose not receive adequate attention among clinicians. Therefore, this survey highlights the necessity of raising awareness of chronic cough. In the future, much more work needs to be done to improve the diagnosis and management of cough, especially the promotion and popularization of guidelines.
Acknowledgments
The authors thank all the patients who participated in this study. And they were indebted to Yanmei Ye, Jianfeng Yang, Yuena Cai, Liqian Wen, Guangyun Cai, Xueying Yu, Yongwen Li, Yangling Ou, Jie Cai, Cuiyi Chen, Yinghan Long for assistance with recruiting subjects. Special thanks to Chen Zhan and Yonglin Mai for assistance in manuscript editing.
Funding: This study was supported by Key-Area Research and Development Program of Guangzhou Province (No. 2019B020227006), and Incubative Project for Innovation Team of GMU (No. 2017-159). The funders had no role in the study design, the collection, analysis and interpretation of data, the writing of the manuscript, and the decision to submit the manuscript for publication.
Footnote
Provenance and Peer Review: This article was a standard submission for the series “Cough Section” published in Journal of Thoracic Disease. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1737/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1737/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1737/coif). KL serves as an unpaid editorial board member of Journal of Thoracic Disease. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (No. 201778), and written informed consent was obtained from all participants prior to study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Morrell DC. Symptom interpretation in general practice. J R Coll Gen Pract 1972;22:297-309. [PubMed]
- Song WJ, Chang YS, Faruqi S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J 2015;45:1479-81. [Crossref] [PubMed]
- Morice AH, Millqvist E, Belvisi MG, et al. Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. Eur Respir J 2014;44:1132-48. [Crossref] [PubMed]
- Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 2020;55:1901136. [Crossref] [PubMed]
- Kardos P, Dinh QT, Fuchs KH, et al. German Respiratory Society guidelines for diagnosis and treatment of adults suffering from acute, subacute and chronic cough. Respir Med 2020;170:105939. [Crossref] [PubMed]
- Song DJ, Song WJ, Kwon JW, et al. KAAACI Evidence-Based Clinical Practice Guidelines for Chronic Cough in Adults and Children in Korea. Allergy Asthma Immunol Res 2018;10:591-613. [Crossref] [PubMed]
- Irwin RS, French CL, Chang AB, et al. Classification of Cough as a Symptom in Adults and Management Algorithms: CHEST Guideline and Expert Panel Report. Chest 2018;153:196-209. [Crossref] [PubMed]
- Committee for the Japanese Respiratory Society Guidelines for Management of Cough. The Japanese Respiratory Society guidelines for management of cough. Respirology 2006;11:S135-86. [PubMed]
- Gibson PG, Chang AB, Glasgow NJ, et al. CICADA: Cough in Children and Adults: Diagnosis and Assessment. Australian cough guidelines summary statement. Med J Aust 2010;192:265-71. [Crossref] [PubMed]
- Chinses Thoracic Society (CTS) Asthma Cosortium. Chinese guidelines for diagnosis and management of cough (2005). Chin J Tuberc Respir Dis 2005;28:738-44.
- Chinses Thoracic Society (CTS) Asthma Cosortium. Chinese guidelines for diagnosis and treatment of cough (2009). Chin J Tuberc Respir Dis 2009;32:407-13.
- Chinses Thoracic Society (CTS) Asthma Cosortium. Chinese guidelines for diagnosis and treatment of cough. Chin J Tuberc Respir Dis 2016;39:323-54.
- Lai K, Chen R, Lin J, et al. A prospective, multicenter survey on causes of chronic cough in China. Chest 2013;143:613-20. [Crossref] [PubMed]
- Lai K, Li B, Wang F, et al. Survey on the diagnosis and management of the patients with chronic cough. Chin J Asthma 2011;5:8-10.
- Chamberlain SA, Garrod R, Douiri A, et al. The impact of chronic cough: a cross-sectional European survey. Lung 2015;193:401-8. [Crossref] [PubMed]
- Marchant JM, Newcombe PA, Juniper EF, et al. What is the burden of chronic cough for families? Chest 2008;134:303-9. [Crossref] [PubMed]
- Zeiger RS, Schatz M, Hong B, et al. Patient-Reported Burden of Chronic Cough in a Managed Care Organization. J Allergy Clin Immunol Pract 2021;9:1624-1637.e10. [Crossref] [PubMed]
- French CT, Fletcher KE, Irwin RS. Gender differences in health-related quality of life in patients complaining of chronic cough. Chest 2004;125:482-8. [Crossref] [PubMed]
- Yang C, Chen R, Li B, et al. Survey of quality of life and incontinence in female patients with chronic cough. Chin J Asthma 2010;4:252-5.
- Xu M, Shan H, Li Y, et al. Survey of quality of life and incontinence in 100 female patients with chronic cough. Chin J Matern and Child Health Care 2015;30:2816-7.
- Ma W, Yu L, Wang Y, et al. Changes in health-related quality of life and clinical implications in Chinese patients with chronic cough. Cough 2009;5:7. [Crossref] [PubMed]
- Shi X, Peng QF, Kong LF. An analysis of factors for quality-of-life in patients with chronic cough. Zhonghua Nei Ke Za Zhi 2011;50:672-5. [PubMed]
- Lai K, Huang L, Zhao H, et al. Clinical characteristics of patients with chronic cough in Guangdong, China: a multicenter descriptive study. BMC Pulm Med 2021;21:305. [Crossref] [PubMed]
- Asano T, Takemura M, Fukumitsu K, et al. Diagnostic utility of fractional exhaled nitric oxide in prolonged and chronic cough according to atopic status. Allergol Int 2017;66:344-50. [Crossref] [PubMed]
- Birring SS, Prudon B, Carr AJ, et al. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax 2003;58:339-43. [Crossref] [PubMed]
- Raj AA, Pavord DI, Birring SS. Clinical cough IV:what is the minimal important difference for the Leicester Cough Questionnaire? Handb Exp Pharmacol 2009;311-20. [Crossref] [PubMed]
- Li B, Lai K, Wang F, et al. Quality of life questionnaire in patients with chronic cough. Chin J Asthma 2011;5:11-4.
- Lai K, Long L. Current Status and Future Directions of Chronic Cough in China. Lung 2020;198:23-9. [Crossref] [PubMed]
- Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet 2008;371:1364-74. [Crossref] [PubMed]
- Braman SS. Chronic cough due to chronic bronchitis: ACCP evidence-based clinical practice guidelines. Chest 2006;129:104S-15S. [Crossref] [PubMed]
- Chinses Thoracic Society (CTS) Asthma Cosortium. Guideline for primary care of cough(2018). J Chinese Journal of General Practitioners 2019;18:207-19.
- Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest 2006;129:63S-71S. [Crossref] [PubMed]
- Won HK, Lee JH, An J, et al. Impact of Chronic Cough on Health-Related Quality of Life in the Korean Adult General Population: The Korean National Health and Nutrition Examination Survey 2010-2016. Allergy Asthma Immunol Res 2020;12:964-79. [Crossref] [PubMed]
- French CT, Fletcher KE, Irwin RS. A comparison of gender differences in health-related quality of life in acute and chronic coughers. Chest 2005;127:1991-8. [Crossref] [PubMed]
- Lai K, Long L, Yi F, et al. Age and Sex Distribution of Chinese Chronic Cough Patients and Their Relationship With Capsaicin Cough Sensitivity. Allergy Asthma Immunol Res 2019;11:871-84. [Crossref] [PubMed]


