Global development and current evidence of uniportal thoracoscopic surgery
Introduction
Video-assisted thoracoscopic surgery (VATS) has been used in almost all surgical indications for thoracic disease, including pneumothorax, infectious disease, and malignancy (1). The benefits of VATS include shorter hospital stay, reduced postoperative pain, and superior postoperative quality of life compared to open thoracotomy. Multiple variants of the VATS technique exist, including those that use different port numbers, positions, and entry styles. Most surgeons perform VATS with one utility port plus one or two more assistant ports (2).
Uniportal VATS, also known as single incision thoracoscopic surgery (SITS), has gained popularity in the past decade. Rocco et al. published the first case series of uniportal VATS pulmonary wedge resection in 2004 (3). Since then, uniportal VATS has been successfully performed for numerous indications. When performing thoracic endoscopic surgery with all instruments in a single incision, the collision of instruments is inevitable and might compromise the operative outcome. However, with the advent of specialized surgical instruments and the improvement of surgical technique, we can safely perform not only simple operations, such as diagnostic procedures or sympathectomy, but also more complication procedures, such as anatomic resection of the lung (4).
The number of patients who have undergone uniportal VATS and the number of published studies regarding this procedure are increased rapidly. Interestingly, with the increasing number of patients undergoing this operation, surgeons in Asian countries seem more inclined to practice uniportal VATS. Some authors reported various additional benefits of the uniportal approach versus its multi portal counterpart, while others demonstrated no difference between the procedures. The aim of this review was to provide a clear picture of the current achievements associated with uniportal VATS, its development and geographic distribution, accumulated evidence of its actual benefits, and educational resources.
Methods
An electronic search was performed in databases including PubMed, The Cochrane Library, and Embase. The search terms were “single port” or “single incision” or “uniportal”, and “VATS”. We sought controlled trials, observational studies, case series, case reports, and review articles. The searches were limited to English-language articles published before November 2015. Only articles that provided full text were included.
From these articles, we included those that described surgery attempted with only one incision. The following characteristics were recorded: number of each type of procedure, operative time, blood loss, complications and mortality, length of incision, hospital stay, and rate of conversion. With respect to surgery for cancer treatment, we also collected data regarding oncological outcomes, such as overall survival (OS) and recurrence-free survival (RFS).
Results
Current publications
A total of 240 articles were found using the search criteria. After excluding articles without complete data, articles not written in English, and letters or replying commentaries, 192 articles remained: 102 original articles, 49 case reports, and 41 review or technical articles mentioning SITS or uniportal VATS.
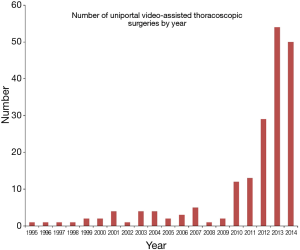
Before 2010, there were generally fewer than 10 articles published each year. In the past half-decade, there was a sharp increase in number; there were 54 publications in 2014 and 50 in 2015. The number of publications by year is presented in Figure 1.
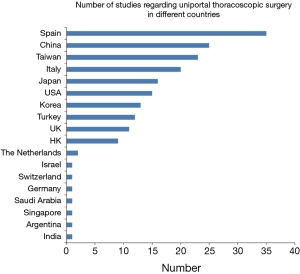
The top three countries with the highest number of publications were Spain with 35 articles; China, 25; and Taiwan, 23. The complete list is shown in Figure 2. Overall, authors from Asian countries published more articles regarding uniportal VATS. Among the European countries, Spain, Italy, Turkey, and the UK were those that had more interest in uniportal VATS than the others. In addition, of the 35 articles from Spain, 26 of them were the works of one group: Gonzalez-Rivas et al.
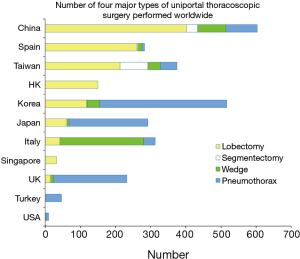
From a total of 9,545 operations attempted in the fashion of uniportal VATS, 61 (0.61%) were converted to either 2- or 3-port VATS, or thoracotomy. Sympathectomy was the most common operation, with 6,845 procedures. Other popular operations included 1,293 lobectomies and 1,024 uniportal VATS for spontaneous pneumothorax. In Figure 3, we compare the four main types of surgery by country. The four types of surgery included two types of major lung resection, lobectomy and segmentectomy, and two types of VATS surgery involving primarily minor lung resection, and wedge and pneumothorax surgery. China, Spain, and Taiwan published the most uniportal lobectomy cases, while most of the pneumothorax surgeries were published by authors from Korea, Japan, and the UK.
Perioperative outcome of uniportal versus conventional VATS
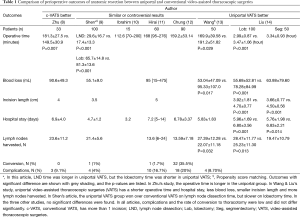
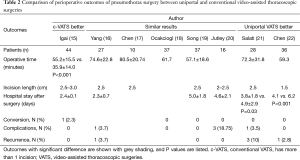
Many authors have reported large series of uniportal VATS operations, with low morbidity and low 30-day mortality. However, perioperative parameters varied greatly between centers. For example, the operative time for lobectomy ranged from 80 to 230 minutes (5,6). Hsu et al. (7) reported the first multi-institutional study for perioperative outcome of uniportal VATS and demonstrated that in experienced centers there is a general decline in the rate of conversion and complication after 2–4 years of practice, but that great differences in operative time and the numbers of harvested lymph nodes exist between hospitals. Thus, we focused on those publications that compared uniportal and conventional VATS. These studies mainly included surgery for pneumothorax and lung anatomic resection. The comparison of perioperative outcomes is listed in Tables 1,2. Table 1 shows the seven articles in which the authors compared outcomes of anatomic resection with uniportal and conventional VATS in their own institutes. Three of the articles found no significant differences between the two VATS approaches. Two showed that uniportal VATS had a mildly increased operative time, while other outcomes were similar. In Liu’s series, uniportal VATS surpassed conventional VATS in many aspects, such as less blood loss, shorter operative time and hospital stay, and a greater number of harvested lymph nodes (14). In that article, the author provided figures that demonstrated improved operative results year by year. Wang and Shen et al. compared anatomic resections in uni- or multi portal VATS with propensity score matching (9,13). In Shen’s series, the operative time was longer during lymph node dissection, but shorter during lobectomy. In Wang’s study, 35 lobectomies and 15 segmentectomy were performed in a uniportal fashion. The uniportal group had shorter operative time, less blood loss, and a greater number of harvested lymph nodes. The comparison of surgery for pneumothorax revealed similar or superior results associated with uniportal VATS in seven of 8 articles (Table 2). Morbidity and recurrence rates after uniportal VATS are generally low. In Salati and Chen’s studies, patients who received uniportal VATS had shorter hospital stays.
Full table
Full table
In conclusion, in either anatomic resection or pneumothorax operations, most studies show that uniportal VATS is not inferior to multi portal VATS. Several authors also demonstrated better results in the uniportal group; two studies of pneumothorax surgery showed uniportal VATS was associated with shorter hospital stays, and two studies of anatomic resection showed numerous benefits, such as shorter hospital stay, less blood loss, smaller wound size, and a larger number of retrieved lymph nodes. Only one study in each surgical type showed that conventional VATS was superior to uniportal VATS with respect to operative time, which could be overcome with practice.
Pain and paresthesia issue
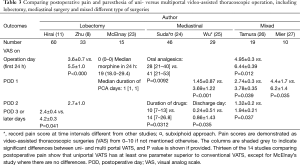
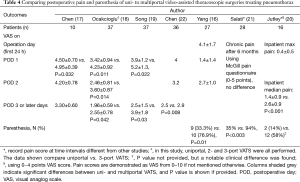
Pain reduction is an important goal for many surgeons who attempt uniportal VATS. However, does applying the uniportal technique actually reduce patient’s suffering? In the current study, of the 192 articles identified in our search, 14 focused on the evaluation of pain score. Those 14 articles are summarized in Tables 3,4. Three of these articles included the evaluation of patients with NSCLC, with a total of 108 lobectomies performed. Two articles that focused on mediastinal surgery included seven patients with spontaneous pneumothorax. The remaining two studies had a mixture of patients. Tamura et al. reported the results of operations on 19 patients, including 5 wedge resections, 10 pneumothorax operations, and 4 mediastinal operations. Mier et al. analyzed a group of patients who underwent lung biopsies, the pneumothorax procedure, and mediastinal cyst excisions.
Full table
Full table
From these reports, we concluded that uniportal VATS caused no more pain than conventional VATS and, apart from one study, all investigations showed that uniportal VATS was superior to its conventional counterpart for at least one pain-related parameter. In most studies, a 0–10 numeric visual analog pain scale was used, and many authors recorded pain scores on each day after the operation. Suda et al. recorded the amount and duration of oral analgesics used after the operation (24). Wu et al. evaluated the pain score on the day of discharge, and their uniportal VATS patients were discharged 3.75±1.53 days postoperatively, which is significantly shorter than that for conventional VATS (28). In McElnay’s article, the first day pain score, median days of patient-controlled anesthesia use, and median amount of morphine used were compared (23). The pain score was zero in both uni- and multiportal groups, and the two other parameters were also similar. Young et al. recently reported a best-evidence topic: “Is uniportal thoracosopic surgery less painful than multiple port approaches?” (29). That article, which commented on the very issue that is the focus of the present review, included 10 papers and 2 abstracts. In one of the two abstracts, Byun et al. showed significant lower median pain score associated with uniportal VATS, while in the other Socci et al. reported no statistical differences in postoperative pain between uni- and multiportal groups (30,31). In most articles, the level of evidence was highest in level IIb, while in all of them the case number was small. The author concluded that uniportal VATS might have a small effect on early postoperative pain because only half of the studies showed significant reduction of postoperative pain, and most reported differences in pain score of only 1 or 2 points.
Paresthesia is also an important complication after thoracic surgery; however, this issue was not addressed in the study conducted by Young et al. Three of the 14 articles compared postoperative paresthesia in uni- versus multi portal VATS, and recorded the patient’s neurological complications or paresthesia. In Yang and Salati’s studies, the incidence of paresthesia was significantly lower among patients in the uniportal group. According to the study of Jutley et al., 86% of patients with multi-port VATS developed paresthesia, compared to just 58% of patients with uniportal VATS (20). Although the P value was not provided, the clinical difference was evident. Neurological symptoms or paresthesia is a distinct complaint in VATS patients. Sihoe et al., described as many as 52.8% of patients having such complaints, and as many as 21% of patients having symptoms that last more than a year (32). These neurological symptoms can be very troublesome, and are often not amendable to oral analgesics. Reducing the number of ports also reduces the chance of intercostal nerve damage, and lowers the risk for paresthesia. The results presented in tables underscores this theory.
In conclusion, most of the studies reviewed showed that uniportal VATS produces less pain than does conventional VATS, but that there is generally a small difference in the degree of pain score difference. All three studies showed that uniportal VATS was associated with significant lower incidence of paresthesia. Reducing the number of ports used in the surgery might be crucial to reduce the chance of developing intercostal nerve injury.
Technical instructions for anatomic lung resection
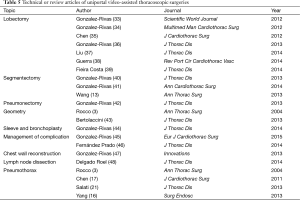
One of the most challenging tasks in the SITS operation is anatomic lung resection. Thus, in the articles reviewed many surgeons have provided suggestions and tips for surgical procedures. The articles listed in Table 5 describe the technical issues of specific operations. Uniportal VATS for the management of pneumothorax, lobectomy, segmentectomy, pneumonectomy, and even detailed techniques on chest wall reconstruction and lymph node dissection has been described. Of all the types of surgery that involve VATS, anatomic resection remains the most complex. Gonzalez-Rivas et al. reviewed a comprehensive array of techniques for anatomic lung resection, covering every important aspect encountered in lung cancer surgery, including lobectomy (33,34), segmentectomy (40), pneumonectomy (42), and lobectomy with bronchovascular reconstruction (42). These valuable publications provide many videos and useful suggestions on surgical techniques. Liu’s review of uniportal VATS for lung cancer included a detailed discussion on important aspects of surgical planning, such as incision placing, instrument handling, anesthesia, and patient positioning (37). With respect to lymph node dissection, Liu’s group found that single port surgery led to the harvesting of a higher number of lymph nodes, and shorter operative time and hospital stay (14). That article outlined the number of operations and perioperative outcomes by year, and obvious improvement was observed after several years of skill refinement. A specialized technique, called Liu’s maneuver, was also described to facilitate lymph node dissection.
Full table
To conclude, resources for surgeons interested in uniportal VATS, and literature regarding techniques and helpful suggestions are abundant, especially from the excellent works by Gonzalez-Rivas and Liu. With these resources and several years of practice, thoracic surgeons have an excellent opportunity to grasp the uniportal VATS technique.
Other indications of uniportal video-assisted thoracoscopic surgeries
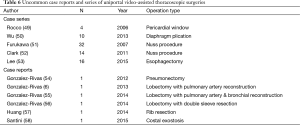
Apart from lung and mediastinal surgery, many different types of surgery, such as those of the diaphragm and chest wall, are also performed with single port VATS. As shown in Table 6, Wu et al. performed 10 uniportal diaphragm plications (50). For chest wall surgery, Furukawa and Clark used the Nuss procedure in a uniportal fashion (51,52). In addition, Huang reported a single port rib resection (57) where they delivered a gigli saw via single incision into the thoracic cavity, and controlled the saw with instruments. Apart from common anatomic resection, Gonzalez-Rivas reported several complex surgeries, such as uniportal lobectomy with pulmonary artery reconstruction and bronchovascular reconstruction.
Full table
In conclusion, many other indications are now also possible in a uniportal setting, including diaphragm and chest wall surgeries.
Subxiphoid approach
Subxiphoid uniportal VATS is yet another variant of VATS. It allows the surgeon to approach both hemithorax from the anterior side using the unusual entry point of the thorax. In contrast, the posterior surface of the pleural cavity is covered by the lungs, making it a more difficult point of access. This incision would be suitable for wedge resection located at the anterior or apical parts of the lungs, anterior mediastinal tumor resection, or thymectomy. Nevertheless, this type of uniportal VATS may not be the best option for operations requiring subcarinal lymph node dissection or treating esophageal cancer. Five studies reported a total of 51 operations that were performed in a subxiphoid uniportal setting. The main study was reported by Suda et al., in which 46 patients underwent uniportal subxiphoid thymectomy for anterior mediastinal tumor or extended thymectomy for those with myasthenia gravis, compared to 35 patients who received 3-port VATS (24). The subxiphoid group had great surgical results, with less blood loss and shorter hospital stay. The author also reported that the uniportal group required less oral analgesics after the operation and used these drugs over a shorter duration. Another reason why the author proposed the subxiphoid approach for anterior mediastinal dissection during thymectomy is that this approach offers the convenience to simultaneously view the bilateral phrenic nerve, instead of performing the VATS bilaterally. With respect to pain reduction, if reducing the number of intercostal ports proportionally reduces paresthesia, then theoretically the subxiphoid incision would eliminate the possibility of intercostal neurological symptoms. Further investigation of long-term postoperative symptoms and satisfaction comparing this modality to other forms of VATS are required to confirm this possible advantage. Other authors have reported subxiphoid single port VATS as case reports, in which they performed lobectomy, bilateral metastasectomy, bilateral sympathectomy, or operations for pneumothorax (59-62).
Therefore, uniportal VATS has a variant—subxiphoid uniportal VATS—that allows assessment of the bilateral pleural cavity with one incision from the anterior aspect and most likely provides an excellent solution to postoperative paresthesia.
Conclusions
Uniportal VATS is a mature variant of VATS, development of which continues to flourish worldwide. During the past 12 years, this approach was practiced in exponentially greater number each year. The surgical quality of this procedure is excellent and has been shown to be superior to conventional VATS in many studies, especially with respect to hospital stay and pain/paresthesia. Many uncommon types of surgery were also reported possible with only a single incision. The resources of education and learning regarding uniportal VATS are abundant and have covered all major aspects of thoracic surgery.
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014;19:552-5. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Single-port video-assisted thoracoscopic lobectomy with pulmonary artery reconstruction. Interact Cardiovasc Thorac Surg 2013;17:889-91. [PubMed]
- Hsu PK, Lin WC, Chang YC, et al. Multiinstitutional analysis of single-port video-assisted thoracoscopic anatomical resection for primary lung cancer. Ann Thorac Surg 2015;99:1739-44. [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i48-i53. [PubMed]
- Ibrahim M, Menna C, Andreetti C, et al. Flexible videoscope for thoracoscopic lobectomy: evolution of uniportal technique. Surg Endosc 2015;29:2056-9. [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i37-i41. [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [PubMed]
- Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique?†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i64-i72. [PubMed]
- Igai H, Kamiyoshihara M, Ibe T, et al. Single-incision thoracoscopic surgery for spontaneous pneumothorax using multi-degrees of freedom forceps. Ann Thorac Cardiovasc Surg 2014;20:974-9. [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [PubMed]
- Chen PR, Chen CK, Lin YS, et al. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax. J Cardiothorac Surg 2011;6:58. [PubMed]
- Ocakcioglu I, Alpay L, Demir M, et al. Is single port enough in minimally surgery for pneumothorax? Surg Endosc 2016;30:59-64. [PubMed]
- Song IH, Lee SY, Lee SJ. Can single-incision thoracoscopic surgery using a wound protector be used as a first-line approach for the surgical treatment of primary spontaneous pneumothorax? A comparison with three-port video-assisted thoracoscopic surgery. Gen Thorac Cardiovasc Surg 2015;63:284-9. [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [PubMed]
- Salati M, Brunelli A, Xiumè F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [PubMed]
- Chen CH, Lee SY, Chang H, et al. The adequacy of single-incisional thoracoscopic surgery as a first-line endoscopic approach for the management of recurrent primary spontaneous pneumothorax: a retrospective study. J Cardiothorac Surg 2012;7:99. [PubMed]
- McElnay PJ, Molyneux M, Krishnadas R, et al. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. Eur J Cardiothorac Surg 2015;47:912-5. [PubMed]
- Suda T, Hachimaru A, Tochii D, et al. Video-assisted thoracoscopic thymectomy versus subxiphoid single-port thymectomy: initial results†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i54-i58. [PubMed]
- Wu CF, Gonzalez-Rivas D, Wen CT, et al. Comparative Short-Term Clinical Outcomes of Mediastinum Tumor Excision Performed by Conventional VATS and Single-Port VATS: Is It Worthwhile? Medicine (Baltimore) 2015;94:e1975.
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [PubMed]
- Mier JM, Chavarin A, Izquierdo-Vidal C, et al. A prospective study comparing three-port video-assisted thoracoscopy with the single-incision laparoscopic surgery (SILS) port and instruments for the video thoracoscopic approach: a pilot study. Surg Endosc 2013;27:2557-60. [PubMed]
- Wu CF, Gonzalez-Rivas D, Wen CT, et al. Single-port video-assisted thoracoscopic mediastinal tumour resection. Interact Cardiovasc Thorac Surg 2015;21:644-9. [PubMed]
- Young R, McElnay P, Leslie R, et al. Is uniport thoracoscopic surgery less painful than multiple port approaches? Interact Cardiovasc Thorac Surg 2015;20:409-14. [PubMed]
- Byun CS, Hwang JJ, Choi JH, et al. Single incision VATS bullectomy with suture-lift method in primary spontaneous pneumothorax. Available online: http://meetings.ismics.org/abstracts/2013/P72.cgi
- Socci L, Jones V, Malik M, et al. Single-port video-assisted thoracic lung volume reduction surgery for emphysema: reducing surgical trauma does not compromise the procedure. Interact CardioVasc Thorac Surg 2013;17:S41.
- Sihoe AD, Au SS, Cheung ML, et al. Incidence of chest wall paresthesia after video-assisted thoracic surgery for primary spontaneous pneumothorax. Eur J Cardiothorac Surg 2004;25:1054-8. [PubMed]
- Gonzalez-Rivas D. VATS Lobectomy: Surgical Evolution from Conventional VATS to Uniportal Approach. SCI WORLD J 2012:5.
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Thoracoscopic lobectomy through a single incision. Multimed Man Cardiothorac Surg 2012;2012:mms007.
- Chen CH, Lee SY, Chang H, et al. Technical aspects of single-port thoracoscopic surgery for lobectomy. J Cardiothorac Surg 2012;7:50. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Liu CY, Lin CS, Shih CH, et al. Single-port video-assisted thoracoscopic surgery for lung cancer. J Thorac Dis 2014;6:14-21. [PubMed]
- Guerra M, Fernandes P, Martins D, et al. Uniportal thoracoscopic lobectomy. Rev Port Cir Cardiotorac Vasc 2014;21:99-105. [PubMed]
- Fieira Costa E, Delgado Roel M, Paradela de la Morena M, et al. Technique of uniportal VATS major pulmonary resections. J Thorac Dis 2014;6:S660-4. [PubMed]
- Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5 Suppl 3:S226-33. [PubMed]
- Gonzalez-Rivas D. Single incision video-assisted thoracoscopic anatomic segmentectomy. Ann Cardiothorac Surg 2014;3:204-7. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uniportal video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2013;5 Suppl 3:S246-52. [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Gonzalez-Rivas D, Stupnik T, Fernandez R, et al. Intraoperative bleeding control by uniportal video-assisted thoracoscopic surgery. Eur J Cardiothorac Surg 2016;49 Suppl 1:i17-i24. [PubMed]
- Fernández Prado R, Fieira Costa E, Delgado Roel M, et al. Management of complications by uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2014;6:S669-73. [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Single-incision thoracoscopic right upper lobectomy with chest wall resection by posterior approach. Innovations (Phila) 2013;8:70-2. [PubMed]
- Delgado Roel M, Fieira Costa EM, Gonzalez-Rivas D, et al. Uniportal video-assisted thoracoscopic lymph node dissection. J Thorac Dis 2014;6:S665-8. [PubMed]
- Rocco G, La Rocca A, La Manna C, et al. Uniportal video-assisted thoracoscopic surgery pericardial window. J Thorac Cardiovasc Surg 2006;131:921-2. [PubMed]
- Wu HH, Chen CH, Chang H, et al. A preliminary report on the feasibility of single-port thoracoscopic surgery for diaphragm plication in the treatment of diaphragm eventration. J Cardiothorac Surg 2013;8:224. [PubMed]
- Furukawa H, Sasaki S, William M, et al. Modification of thoracoscopy in pectus excavatum: insertion of both thoracoscope and introducer through a single incision to maximise visualisation. Scand J Plast Reconstr Surg Hand Surg 2007;41:189-92. [PubMed]
- Clark JJ, Johnson SM. Single incision Nuss procedure for pectus excavatum. Pediatr Surg Int 2011;27:733-6. [PubMed]
- Lee JM, Yang SM, Yang PW, et al. Single-incision laparo-thoracoscopic minimally invasive oesophagectomy to treat oesophageal cancer. Eur J Cardiothorac Surg 2016;49 Suppl 1:i59-i63. [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Video: Single-incision video-assisted thoracoscopic right pneumonectomy. Surg Endosc 2012;26:2078-9. [PubMed]
- Gonzalez-Rivas D, Fieira E, de la Torre M, et al. Bronchovascular right upper lobe reconstruction by uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2014;6:861-3. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Huang CL, Cheng CY, Lin CH, et al. Single-port thoracoscopic rib resection: a case report. J Cardiothorac Surg 2014;9:49. [PubMed]
- Santini M, Fiorelli A, Santagata M, et al. Resection of costal exostosis using piezosurgery associated with uniportal video-assisted thoracoscopy. Ann Thorac Surg 2015;99:1080-2. [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxyphoid single-incision thoracoscopic pulmonary metastasectomy. Thorac Cancer 2015;6:230-2. [PubMed]
- Chen JT, Liao CP, Chiang HC, et al. Subxiphoid single-incision thoracoscopic bilateral ablative sympathectomy for hyperhidrosis. Interact Cardiovasc Thorac Surg 2015;21:119-20. [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [PubMed]
- Liu CY, Lin CS, Liu CC. Subxiphoid single-incision thoracoscopic surgery for bilateral primary spontaneous pneumothorax. Wideochir Inne Tech Maloinwazyjne 2015;10:125-8. [PubMed]