Tricuspid valve chordae tendineae as protective filter to prevent massive pulmonary embolism
Although several cases of thrombus-in-transit associated with pro-thrombotic conditions have been reported (1-3), a transit thrombus located in the right ventricular (RV) cavity is extremely rare (4,5). Here, we report a case of nephrotic syndrome (NS) with a RV thrombus-in-transit that threatened to cause a fatal pulmonary embolism (PE).
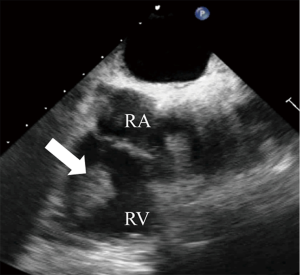
A 32-year-old male who had complained of right leg edema 1 month earlier, was referred to our hospital with chest pain. A chest X-ray revealed a right pulmonary infiltrative shadow. Contrast-enhanced chest computed tomography (CT) revealed filling defects in not only the right pulmonary inferior lobe artery, suggestive of a PE, but also in the RV cavity (Figure 1A). Transthoracic echocardiography (TTE) detected a large lobulated mass (23 mm × 30 mm) in the RV cavity with preserved contractile function of the right and left ventricles (Figure 1B). Interestingly, close observation by TTE revealed that the lobulated mass was not attached to the RV wall, and that the two lobules of the mass rubbed against one another, implying that the longitudinal mass was folded, and straddled the chordae tendineae of the tricuspid valve (TV) (Figure 2). The laboratory data were as follows: d-dimer, 8.28 μg/mL; serum albumin, 0.4 g/dL; total cholesterol, 363 mg/dL; and urinary protein excretion, 17.9 g/gCr, indicating NS. Based on these findings, we strongly suspected that the mass in the RV was an embolus derived from a deep vein thrombosis caused by NS, which subsequently caused a small PE. A thrombus formed inside the vein in the right leg might retain the shape of the vessel in which it originates. Initially, this patient was treated with 18,000 U/day heparin for 4 days, but the RV thrombus-in-transit was not reduced in size. The regimen was then modified to a continuous infusion of urokinase (240,000 U/day), and 4 days later, transesophageal echocardiography revealed an isolated thrombus that had become slightly smaller but still clung tightly to the chordae tendineae of the TV (Figures 3,4). As a result of thrombolytic therapy for 10 days, TTE and enhanced CT demonstrated the disappearance of the RV thrombus (Figure 5), and that the pulmonary artery thrombus was reduced in size. Subsequently, intravenous infusion of heparin was resumed and continued until renal biopsy was performed. The patient did not have any hemorrhagic complications. A percutaneous renal biopsy demonstrated that a minimal change disease was the cause of the NS. The anticoagulation therapy regimen was changed to warfarin, and steroid therapy for the treatment of minimal change disease was started. Normalization of d-dimer levels was achieved 4 weeks later. The patient’s recovery was uneventful. Anticoagulation therapy was continued, as a residual small thrombus behind venous valve pockets in the right leg was observed by vascular ultrasound.
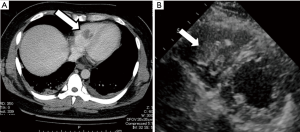
In this case, TTE revealed a large lobulated mass in the RV cavity. The differential diagnosis of the RV mass included primary or metastatic cardiac neoplasms (9) and large vegetation. In addition to a history of leg edema and a typical NS profile on laboratory analysis, the lack of adhesion of the mass to the RV wall and the lack of association with valve leaflets helped to distinguish the thrombus. Unlike other modalities of cardiac imaging, the contribution of echocardiography to tissue characterization is limited; however, echocardiography can evaluate rapid motion with ease. Notably, the finding of the rubbing motion of the two lobules of the mass, constituting a unique echocardiographic appearance, has not been reported previously and represents valuable information for the diagnosis of a thrombus-in-transit which straddled the chordae tendineae of the TV.
Although a right cardiac thrombus-in-transit under pro-thrombotic conditions has rarely been reported, it occurs predominantly in the right atrium (10). In addition to the low pressure in the chamber, structural features of the RV such as multiple chordal attachments to the ventricular septum, a triangular-shaped ventricular cavity, the presence of the moderator band, coarse apical trabeculation, and a trileaflet atrioventricular valve may predispose the RV to a thrombus-in-transit compared to the left ventricle. Nevertheless, a transit RV thrombus entangled in the chordae tendineae of the TV is extremely rare. Because the chordae tendineae must work together with TV leaflets and papillary muscles to ensure proper coaptation, its main role is recognized to be in transmitting tension to the TV, causing them to open and close. Interestingly, the chordae tendineae in this case also acted as a protective filter and prevented a massive fatal PE.
In this case, the therapeutic options included medication and surgery. Myers et al. have shown that thrombolysis is less desirable than surgical thromboembolectomy for the treatment of a biatrial thromboembolus caught in transit across a patent foramen ovale (11). Given the negligible risk for systemic embolism due to the lack of a patent foramen ovale and the high risk of cardiac surgery due to the patient’s poor general condition, we decided to give thrombolytic therapy. Although the selected treatment in this case was met with good clinical outcome, the treatment selection for other thrombus-in-transit cases warrants further investigation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Eweda II, Samir S, Abbas O, et al. Right heart thrombus-in-transit with pulmonary embolism in a patient with primary hypercoagulable state. Cardiol J 2010;17:408-11. [PubMed]
- Rivera IR, da Silva MA, Cavalcanti RC, et al. Right heart emboli-in-transit. Case report and literature review. Arq Bras Cardiol 2008;90:e44-7. [PubMed]
- Shah DP, Min JK, Raman J, et al. Thrombus-in-transit: two cases and a review of diagnosis and management. J Am Soc Echocardiogr 2007;20:1219.e6-8.
- Casazza F, Caponi C, Mignoli S. A four-chamber in transit heart thrombus in a pregnant woman with acute pulmonary embolism. Thromb Haemost 2015;114:5-6. [Crossref] [PubMed]
- Moaref AR, Mollazadeh R, Amirghofran AA, et al. Thrombus entrapped in tricuspid chordae masquerading as tumour. Eur J Echocardiogr 2008;9:572-4. [Crossref] [PubMed]
- Watanabe H, Shimbo M, Terada M, et al. TTE showing a large lobulated mass in the RV cavity. Asvide 2016;3.163. Available online: http://www.asvide.com/articles/921
- Watanabe H, Shimbo M, Terada M, et al. A transesophageal echocardiographic image produced 4 days after initiating thrombolytic therapy. Note the isolated thrombus, which had become slightly smaller but still clung tightly to the chordae tendineae of the TV. Asvide 2016;3.164. Available online: http://www.asvide.com/articles/922
- Watanabe H, Shimbo M, Terada M, et al. TTE and transesophageal echocardiography showing the disappearance of the RV thrombus. Asvide 2016;3.165. Available online: http://www.asvide.com/articles/923
- Sen S, Naina HV, Gupta A. Persistent Intracardiac Thrombus: Could it be Cancer? J Gen Intern Med 2016;31:357. [Crossref] [PubMed]
- Casazza F, Bongarzoni A, Centonze F, et al. Prevalence and prognostic significance of right-sided cardiac mobile thrombi in acute massive pulmonary embolism. Am J Cardiol 1997;79:1433-5. [Crossref] [PubMed]
- Myers PO, Bounameaux H, Panos A, et al. Impending paradoxical embolism: systematic review of prognostic factors and treatment. Chest 2010;137:164-70. [Crossref] [PubMed]


