
Diagnosis of mediastinal cysts: the role and safety of EUS–FNA with 19-gauge needle: a retrospective cohort study
Introduction
Mediastinal cysts form a group of uncommon benign lesions that are generally considered as associated with developmental disorder in the foregut during embryogenesis (1,2). Foregut cysts including bronchogenic cysts and enteric cysts are the most common mediastinal cysts, accounting for about 20% of the mediastinal masses (2,3). Mediastinal cysts are usually asymptomatic in adults and detected by incidental radiological imaging but also can present with a variety of symptoms, especially coughing and chest pain, which are generally due to compression of adjacent structures. As they can simulate multiple lesions at imaging, both benign and malignant, accurate diagnosis is important to the development of therapeutic strategies.
Currently, a presurgical diagnosis can be made by computed tomography (CT) and magnetic resonance imaging (MRI). However, 30–80% of lesions might be misdiagnosed as solid masses resulting from high protein content in the cystic lumen (4-6). Endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) offers a noninvasive way to obtain tissues for cytological examination prior to surgery, which could be regarded a more accurate diagnostic method for mediastinal cysts (1,7). However, acquiring adequate samples from the cystic wall for diagnosis remains challenging, as some cysts contain thick proteinaceous material that is difficult to aspirate.
Most previous reports of cytological biopsies of mediastinal cysts by EUS-FNA have been case reports. The present study evaluated the safety and utility of EUS-FNA for diagnosis and treatment of mediastinal cysts. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1105/rc).
Methods
Patients
This was a retrospective cohort study. A total of 15,492 patients underwent EUS, of whom 1,636 underwent EUS-FNA at Tianjin Medical University Cancer Institute and Hospital between January 2016 and December 2020. The medical records of patients who underwent EUS-FNA and were further diagnosed with mediastinal cysts were retrospectively collected. Clinical presentation, radiological findings, EUS-FNA procedure, cytopathology reports, and follow-up were all analyzed. The presence of a benign cyst was established through EUS or EUS-FNA consistent with a mediastinal cyst, or surgical pathological confirmation. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Tianjin Medical University Cancer Institute and Hospital (No. bc2022134). Informed consent was routinely acquired from all patients before EUS-FNA examination.
EUS-FNA
The EUS-FNA was performed in the standard fashion. The routine preoperative preparation was performed, and all patients fasted for 6–8 h prior to surgery. After patients were placed in the left lateral decubitus position, local anesthesia was administered. Then, US was performed to determine lesion location, size, and surrounding tissue. Diagnosis of foregut cysts by EUS was based on the following criteria: (I) hypoechoic or anechoic lesions; (II) lesions with a well-defined, thin, smooth wall without infiltration to the mediastinum; and (III) texture of the lesion was soft after being compressed by the US probe. The lesion region near the probe was deformed, with a hypoechoic appearance. After compressing the probe rapidly and repeatedly, the hypoechoic lesion with or without hyperechoic debris could move. The EUS-FNA was performed to evaluate cystic lesions. The puncture needle was inserted into the target cyst in closest proximity to the esophagus, and no vessels were confirmed by color Doppler US. Continuous negative pressure suction was performed with a 50 mL syringe to ensure effective drainage. To obtain adequate tissue from the lesions, 19-gauge puncture needles (EchoTip Ultra; Cook Ireland Ltd., Limerick, Ireland) were used for aspiration. A single pass and one-time complete aspiration were performed if the lesion manifested as echoless. However, if the lesion presented as hypoechoic, indicating that the lesion contained semisolid secretions, suction of a larger amount of content was difficult. When the sticky contents were drawn into the syringe or constant aspiration lasted for >5 min, the negative pressure was removed, and the puncture needle was withdrawn.
Sample processing
The aspirated tissue was smeared on a slide and fixed in alcohol. The smears were then sent for cytological analysis. Patients were observed in the recovery area for 30–60 min. Postoperatively, antibiotics (levofloxacin, 5 mg/mL) were intravenously injected for 3 days and then switched to oral administration within 5–7 days to prevent infection.
Assessment of adverse events (AEs)
Safety was estimated by the incidence of reported AEs. AEs were defined as events that prevented completion of EUS-FNA and/or leaded to admission to hospital, prolongation of existing hospital stay or subsequent medical consultation. To evaluate AEs a telephone call was performed by a physician at 48 h and 1 week after EUS-FNA to ask patients whether they had symptoms or needed medical assistance.
Statistical analysis
All the values were expressed as means or medians. Descriptive statistics was used to analyze the data.
Results
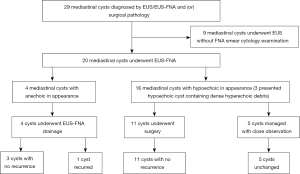
During the study period, 20 patients with mediastinal cysts who underwent EUS-FNA with 19-gauge needles were included in the analysis (Table 1, Figure 1). The mean age was 51 years (range, 29–72 years), and 13 were men. Only 5 cases presented with symptoms, including chest pain or discomfort (n=2, 10%), cough (n=2, 10%) and dysphagia (n=1, 5%). The other 15 patients were asymptomatic, and the cyst was a casual radiological finding.
Table 1
| Patient | Age, years | Gender | Symptom | CT | EUS | Management | Final diagnosis | ||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Size (mm) | FNA | |||||||
| 1 | 50 | F | Cough | Cyst | Anechoic cyst | 43×42 | Clear | EUS-FNA drainage | Bronchogenic cyst |
| 2 | 32 | M | Chest pain | Mass | Hypoechoic cyst with dense hyperechoic debris | 45×36 | Thick | Surgery | Bronchogenic cyst |
| 3 | 45 | F | Asymptomatic | Mass | Hypoechoic cyst | 35×25 | Thick | Surgery | Bronchogenic cyst |
| 4 | 48 | M | Asymptomatic | Mass | Hypoechoic cyst | 67×36 | Thick | Observation | Bronchogenic cyst |
| 5 | 31 | F | Asymptomatic | Mass | Anechoic cyst | 27×17 | Clear | EUS-FNA drainage | Enteric cyst |
| 6 | 55 | F | Chest pain | Neurogenic tumour | Hypoechoic cyst with dense hyperechoic debris | 38×37 | Thick | Surgery | Bronchogenic cyst |
| 7 | 41 | M | Asymptomatic | Neurogenic tumour | Hypoechoic cyst | 55×43 | Thick | Surgery | Bronchogenic cyst |
| 8 | 40 | M | Asymptomatic | Mass | Hypoechoic cyst | 32×30 | Thick | Observation | Bronchogenic cyst |
| 9 | 43 | M | Asymptomatic | Cyst | Hypoechoic cyst | 79×22 | Thick | Observation | Bronchogenic cyst |
| 10 | 46 | F | Asymptomatic | Lymphangioma | Hypoechoic cyst with dense hyperechoic debris | 35×23 | Thick | Surgery | Enteric cyst |
| 11 | 66 | M | Asymptomatic | Mass | Hypoechoic cyst | 45×32 | Thick | Surgery | Bronchogenic cyst |
| 12 | 34 | M | Cough | Cyst | Hypoechoic cyst | 33×23 | Thick | Surgery | Pericardial cyst |
| 13 | 81 | M | Asymptomatic | Mass | Hypoechoic cyst | 61×43 | Thick | Observation | Bronchogenic cyst |
| 14 | 17 | F | Asymptomatic | Neurogenic tumour | Hypoechoic cyst | 43×33 | Thick | Surgery | Bronchogenic cyst |
| 15 | 57 | M | Dyspnea | Cyst | Anechoic cyst | 90×80 | Clear | EUS-FNA drainage | Bronchogenic cyst |
| 16 | 53 | M | Asymptomatic | Cyst | Hypoechoic cyst | 30×28 | Thick | Surgery | Enteric cyst |
| 17 | 66 | M | Asymptomatic | Mass | Hypoechoic cyst | 45×32 | Thick | Surgery | Bronchogenic cyst |
| 18 | 52 | M | Asymptomatic | Mass | Anechoic cyst | 26×19 | Clear | EUS-FNA drainage | Bronchogenic cyst |
| 19 | 44 | F | Asymptomatic | Mass | Hypoechoic cyst | 58×40 | Thick | Surgery | Enteric cyst |
| 20 | 50 | M | Asymptomatic | Lymphoma | Hypoechoic cyst | 30×25 | Thick | observation | Bronchogenic cyst |
EUS, endoscopic ultrasound; FNA, fine needle aspiration; CT, computed tomography.
In all 20 cases, CT was performed before EUS, showing that only 5 of them were diagnostic for a cyst, and the other 15 patients (75%) demonstrated a mass, enlarged lymph node, lymphangioma, or neurogenic tumor.
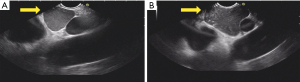
An EUS examination was performed in all cases demonstrating that the lesions were oval or round in shape. The mean length of the cyst in the longest and shortest axes was 46.85 and 33.3 mm, respectively. The cyst wall was monolayer and thin in 19 patients (95%), and 1 had a layered outside wall on EUS examination. Some 11 of the 20 (55%) lesions were located in the posterior mediastinum, as well as 5 in the middle and 4 in the superior mediastinum. Variation existed in the EUS appearance of cyst contents. The characteristic on EUS examination was hypoechoic in 16 patients, among whom, 3 presented with hypoechoic cysts containing dense hyperechoic debris (Figure 2). In the remaining 4 cases, the contents were anechoic in appearance.
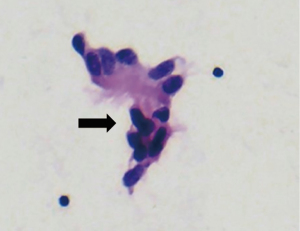
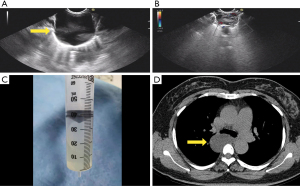
The EUS-FNA samples were successfully obtained by a single pass with a 19-gauge needle in all cases. AEs occurred in 2/20 (10%) patients and these two cases had self-limited chest pain within 48 h after the EUS-FNA (Table 2). None of them need longer hospital stay or subsequent medical consultation. Of 16 patients with hypoechoic appearance of cysts, an average of 2 mL (range, 1–10 mL) of fluid could be aspirated from the cysts due to the thick proteinaceous contents. For the other 4 patients showing no echo through EUS, the cystic cavity almost disappeared after EUS-FNA drainage and an average 40 mL (range, 10–180 mL) of clear fluid could be drained almost completely from the cysts. Cytological and histopathological evaluation was negative for malignancy, showing only mucinous material and bronchial epithelial cells (Figure 3). No recurrence was noted in 3 of 4 cases after at least 6-months of follow-up. The other patient showed relapse at 3 months after EUS-FNA drainage (Figure 4). No patient had an infection-related complication.
Table 2
| Adverse events | Number |
|---|---|
| Bleeding | 0 |
| Fever | 0 |
| Chest pain | 2 (10%) |
| Perforation | 0 |
| Pneumothorax or pneumomediastinum | 0 |
A total of 11 patients who were worried about clinical symptoms or development of malignant transformation of the cyst underwent surgical treatment and were confirmed as having bronchogenic or enteric cyst by postoperative pathology. Further, 8 of 11 patients without symptoms were followed-up for 6–48 months with a mean of 36 months, and remained asymptomatic with no long-term complications.
Discussion
This retrospective cohort study evaluated the safety and clinical effectiveness of EUS-FNA for diagnosis and treatment of mediastinal cysts. The EUS-FNA was more accurate than CT for diagnosis of mediastinal cysts, and this study demonstrated the acceptable low rate of AEs after EUS-FNA, which suggested the utility and safety of EUS-FNA and prophylactic antibiotics for definitive diagnosis of benign mediastinal cysts. No infective complications occurred during the follow-up period. Finally, our results suggested that the resolution of cysts containing thin, free-flowing fluid material can be achieved by a single pass with a 19-gauge needle.
The majority of cases with mediastinal cysts are asymptomatic, with the lesion being detected by routine radiological examination. Surgical resection is recommended for symptomatic cases, whereas the treatment of asymptomatic patients remains controversial (8,9). In a study of 86 patients with bronchogenic cysts, 72% of patients eventually became symptomatic with observation over a 20-year period (10). Mediastinal cysts are frequently treated by complete resection in asymptomatic cases due to the rare development of complications and malignant transformation (11). However, some experts argue that close observation is warranted when the diagnosis has been confirmed by needle aspiration (7). In the current study, 3 symptomatic and 8 asymptomatic patients who were worried about development of possible complications underwent surgical excision. There were no postoperative complications during follow-up.
Cysts vary in their content ranging from thin, free-flowing fluid to viscous mucinous material, leading to lesions being misclassified as soft tissue masses by CT in 43% of patients (6). Eloubeidi et al. (12) reported that 70% of cases were misinterpreted as solid masses. Our data showed that diagnosis of mediastinal cysts was certain in only 25% (5/20) of patients, which was consistent with the previous study suggesting that CT frequently misjudges the cystic nature of lesions.
Using the esophagus as an acoustic medium to image the mediastinum, EUS has been proposed as a method for diagnosis of mediastinal cysts. Commonly, EUS shows the cysts as having anechoic, hypoechoic, or hyperechoic thickening within the cyst walls (5). It remains difficult to distinguish cysts containing viscous mucinous material from hypoechoic malignant masses and the cysts containing hyperechoic debris may be confused with soft-tissue masses. In the present study, we showed after compressing the mass repeatedly by the US probe, if the hypoechoic lesion with or without hyperechoic debris could move, a diagnosis of cystic mass can be made. This manipulation may be more informative for diagnosis of benign cysts.
The method of EUS-FNA has been considered as a technique for precise diagnosis of lesions in and around the gastrointestinal tract (13-16). However, inserting the needle into the sterile environment of a cyst may increase the risk of AEs including infection, bleeding, chest pain, perforation, pneumothorax or pneumomediastinum. Our results showed two patients had self-limited chest pain within 48 h and other AEs were not observed suggesting the safety of EUS-FNA in diagnosis of mediastinal cysts. Wiersema et al. (17) reported infection after puncture of the cyst with a 22-gauge needle and a 19-gauge tru-cut needle without prophylactic antibiotics. Diehl et al. (18) reported 3 cases that developed cyst infections 4–5 days after EUS-FNA by 1–3 passes with a 22-gauge needle, although intravenous prophylactic antibiotics was given before EUS-FNA, and oral ciprofloxacin was given after EUS-FNA. Fazel et al. (5) suggested that use of only 22-gauge needles with prophylactic administration of antibiotics was safe and large-gauge needles were best avoided. Our results demonstrated no infectious complications with the use of 19-gauge needles and prophylactic antibiotics among 20 patients, which suggests that EUS-FNA by a single pass with a 19-gauge needle is safe when antibiotics are intravenously injected for 3 days and then switched to oral administration within 5–7 days to prevent infection. The main reason for this may be differences in antibiotic usage, with different modes of action and the number of punctures. Furthermore, we revealed that a single pass with a 19-gauge needle could acquire adequate tissue for cytological analysis, in order to avoid additional passes.
Long-term cyst regression can be achieved by complete drainage (19,20). Since the wall of the cyst persists, treatment of cystic mass by aspiration alone may lead to recurrence. In the present study, among 4 patients who underwent complete FNA drainage, 3 had good prognosis without recurrence during follow-up, whereas 1 experienced recurrence at 3 months after treatment. These results revealed that FNA could serve as a palliative treatment for patients unable to undergo an open surgical procedure.
The main limitation of this study was that the number of patients was not large enough. However, the rarity of mediastinal cysts makes it difficult to conduct a study of adequate size.
We suggest that the application of EUS-FNA appears safe when antibiotic prophylaxis is used, especially for cysts with viscous proteinaceous contents where fluid is difficult to be aspirated. Future multicenter studies with larger sample sizes will be helpful to confirm our results.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1105/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1105/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1105/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Tianjin Medical University Cancer Institute and Hospital (No. bc2022134). Informed consent was routinely acquired from all patients before EUS-FNA examination.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wildi SM, Hoda RS, Fickling W, et al. Diagnosis of benign cysts of the mediastinum: the role and risks of EUS and FNA. Gastrointest Endosc 2003;58:362-8. [Crossref] [PubMed]
- Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: part II. Tumors of the middle and posterior mediastinum. Chest 1997;112:1344-57. [Crossref] [PubMed]
- Sirivella S, Ford WB, Zikria EA, et al. Foregut cysts of the mediastinum. Results in 20 consecutive surgically treated cases. J Thorac Cardiovasc Surg 1985;90:776-82. [Crossref] [PubMed]
- Odev K, Arıbaş BK, Nayman A, et al. Imaging of Cystic and Cyst-like Lesions of the Mediastinum with Pathologic Correlation. J Clin Imaging Sci 2012;2:33. [Crossref] [PubMed]
- Fazel A, Moezardalan K, Varadarajulu S, et al. The utility and the safety of EUS-guided FNA in the evaluation of duplication cysts. Gastrointest Endosc 2005;62:575-80. [Crossref] [PubMed]
- McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, et al. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology 2000;217:441-6. [Crossref] [PubMed]
- Faigel DO, Burke A, Ginsberg GG, et al. The role of endoscopic ultrasound in the evaluation and management of foregut duplications. Gastrointest Endosc 1997;45:99-103. [Crossref] [PubMed]
- Pugatch RD, Faling LJ, Robbins AH, et al. CT diagnosis of benign mediastinal abnormalities. AJR Am J Roentgenol 1980;134:685-94. [Crossref] [PubMed]
- Patel SR, Meeker DP, Biscotti CV, et al. Presentation and management of bronchogenic cysts in the adult. Chest 1994;106:79-85. [Crossref] [PubMed]
- St-Georges R, Deslauriers J, Duranceau A, et al. Clinical spectrum of bronchogenic cysts of the mediastinum and lung in the adult. Ann Thorac Surg 1991;52:6-13. [Crossref] [PubMed]
- Miralles Lozano F, Gonzalez-Martínez B, Luna More S, et al. Carcinoma arising in a calcified bronchogenic cyst. Respiration 1981;42:135-7. [PubMed]
- Eloubeidi MA, Cohn M, Cerfolio RJ, et al. Endoscopic ultrasound-guided fine-needle aspiration in the diagnosis of foregut duplication cysts: the value of demonstrating detached ciliary tufts in cyst fluid. Cancer 2004;102:253-8. [Crossref] [PubMed]
- Clementsen PF, Bodtger U, Konge L, et al. Diagnosis and staging of lung cancer with the use of one single echoendoscope in both the trachea and the esophagus: A practical guide. Endosc Ultrasound 2021;10:325-34. [Crossref] [PubMed]
- Masoumi-Moghaddam S, Lundy J, Gao H, et al. The EUS molecular evaluation of pancreatic cancer: A prospective multicenter cohort trial. Endosc Ultrasound 2021;10:335-43. [Crossref] [PubMed]
- Solonitsyn EG, Danilov IN, Poddymova AV, et al. EUS-FNA biopsy of parathyroid gland. Endosc Ultrasound 2021;10:315-6. [Crossref] [PubMed]
- Kamata K, Kurita A, Yasukawa S, et al. Utility of a 20G needle with a core trap in EUS-guided fine-needle biopsy for gastric submucosal tumors: A multicentric prospective trial. Endosc Ultrasound 2021;10:134-40. [Crossref] [PubMed]
- Wiersema MJ, Vilmann P, Giovannini M, et al. Endosonography-guided fine-needle aspiration biopsy: diagnostic accuracy and complication assessment. Gastroenterology 1997;112:1087-95. [Crossref] [PubMed]
- Diehl DL, Cheruvattath R, Facktor MA, et al. Infection after endoscopic ultrasound-guided aspiration of mediastinal cysts. Interact Cardiovasc Thorac Surg 2010;10:338-40. [Crossref] [PubMed]
- Schwartz DB, Beals TF, Wimbish KJ, et al. Trans-bronchial fine needle aspiration of bronchogenic cysts. Chest 1985;88:573-5. [Crossref] [PubMed]
- Whyte MK, Dollery CT, Adam A, et al. Central bronchogenic cyst: treatment by extrapleural percutaneous aspiration. BMJ 1989;299:1457-8. [Crossref] [PubMed]
(English Language Editor: J. Jones)


