
The clinical characteristics and surgical treatment for delayed blunt thoracic aortic injury—a case series
Introduction
Blunt thoracic aortic injury (BTAI) is a leading cause of death, second only to head injury in patients with blunt trauma (1,2). Despite its low incidence, accounting for about 1.5% to 2.0% of chest trauma, BTAI is considered a life-threatening condition (3,4). The exact mechanisms underlying BTAI have been studied extensively, and there are 2 leading theories. The most commonly described physical mechanism is rapid deceleration with the application of either anteroposterior or lateral forces upon the relatively mobile ascending thoracic aorta, with shearing forces predominantly at the aortic isthmus. The other major physical theory underlying BTAI is direct penetrating injury from rib and thoracic vertebral fractures (5-7). About 80% of patients with BTAI die before admission, and the in-hospital mortality rate is as high as 50% (5,8). BTAI can be detected easily by computed tomography (CT) of the chest or great vessel post-trauma, with a diagnostic accuracy of up to 100% (9). However, the specific type known as delayed blunt thoracic aortic injury (DBTAI) is a notable exception. To date, far too little attention has been paid to DBTAIs resulting from rib fractures (RFs). Although the condition is uncommon, a missed diagnosis can lead to fatal bleeding complications. Early diagnosis and timely treatment are crucial for preventing such adverse outcomes. Considering the possibility of continuous displacement in the short term (10), theoretically speaking, fresh fractures in the left posterior ribs near the descending aorta entail the risk of aortic injuries, despite the fact that the number of such reported complications are on the scarce side. Which kind of patients should be prioritized? Patients with severe RFs are frequently associated with other injuries. How should surgical treatment be performed effectively? We present the following article in accordance with the AME Case Series reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1359/rc).
Methods
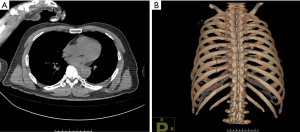
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Shanghai Sixth People’s Hospital (No. 2020-KY-034). Individual consent for this retrospective analysis was waived. Clinical data were collected from 7 patients who received treatment at the Shanghai Jiao Tong University Affiliated Sixth People’s Hospital due to closed RF-induced delayed thoracic aortic injury (DTAI) from June 2015 through June 2020. There were 5 male and 2 female patients aged from 43 to 64 years. The injuries involved the following mechanisms: falls from height (n=3), motor vehicle accidents (n=2), falls from a bicycle (n=2), and getting hit by a heavy object (n=1). RFs with dislocation and injuries to the aorta were absent on the chest CT on the day of injury (Figure 1A,1B). Findings on the chest CT at 1–4 days post-injury indicated possible TAI caused by RFs. The RF broken ends causing aortic injury were all found in the lateral erector spinae, and >3 fractured ribs were present in all these patients. There were left RFs (n=2), left RFs with spleen rupture (n=2), bilateral RFs (n=1), left rib and leg fractures (n=1), and left RFs with hip dislocation and lumbar spine fractures (n=1). The thoracic aorta was either directly injured by left RF broken ends (n=5) or by free bone fragments (n=2). The posterior ribs that injured the aorta were the 6th (n=1), 7th (n=3), 8th (n=2), and 5th–8th (n=1) posterior ribs.
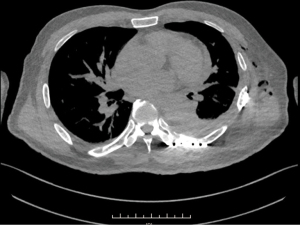
The surgical procedures are summarized as follows: A patient in a state of shock upon admission underwent emergency exploratory laparotomy and splenectomy. At 4 days post-surgery, the free bone fragments of the 7th left rib were found to have potentially injured the thoracic aorta (Figure 2). At 5 days post-injury, the patient received open reduction and thoracoscopic removal of free bone fragments. In a case of left RFs with spleen rupture, the patient was transferred to our hospital after conservative treatment. As the CT scan upon admission indicated possible TAI (Figure 3), the patient underwent emergency exploratory thoracotomy, surgical fixation, and aortic repair simultaneously. As for the 2 cases of left RFs with lumbar spine and leg fractures, exploratory thoracotomy was performed following surgical fixation. The left and bilateral RF cases received surgical fixation of the fractured ribs on the left side and exploratory thoracotomy. The intraoperative exploration revealed that 6 patients had hematomas in the aortic tunica adventitia, and 1 had a ruptured aortic tunica adventitia and elastic layers. Details are presented in Table 1. The literature review covered 8 cases of RF-induced descending aortic injury, of which 3 were caused by free bone fragments and 5 by broken ends. The treatment methods were resection of broken ends and removal of free bone fragments with atraumatic sutures (n=8). Details of these cases are listed in Table 2.
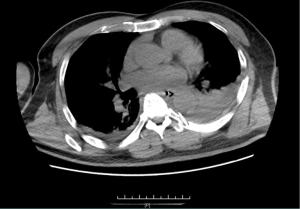

Table 1
| Gender | Age (year) | Injury factor | Time from injury to CT finding that ribs were closely related to the aorta (d) | Left-sided rib fractures | Posterior rib of the injured aorta | Complicated injury | Surgery | Aortic injury | Hospital stay (d) |
|---|---|---|---|---|---|---|---|---|---|
| Male | 62 | Fall from height | 4 | 3rd–9th rib fractures | 7th posterior rib | Splenic rupture | Staged surgery, splenectomy first | Adventitial hematoma | 9 |
| Male | 63 | Fall from height | 3 | 3rd–11th rib fractures | 6th posterior rib | Splenic rupture | Synchronous surgery, rib fracture fixation and aortic repair first | Rupture of the aortic adventitia and elastic layer | 21 |
| Male | 51 | Motor vehicle accident | 2 | 2nd–11th rib fractures | 7th posterior rib | Fracture of the 2nd lumbar vertebra | Staged surgery, rib fracture fixation and thoracoscopic exploration first | Adventitial hematoma | 7 |
| Male | 58 | Fall from a bicycle | 3 | 2nd–10th rib fractures | 8th posterior rib | No | Rib fracture fixation and thoracoscopic exploration | Adventitial hematoma | 3 |
| Male | 43 | Motor vehicle accident | 3 | 2nd–11th rib fractures | 8th posterior rib | Left lower limb fracture, left hip dislocation | Staged surgery, rib fracture fixation and thoracoscopic exploration first | Adventitial hematoma | 14 |
| Female | 54 | Fall from height | 1 | 3rd–10th rib fractures | 5th–8th posterior ribs | No | Rib fracture fixation and thoracoscopic exploration | Adventitial hematoma | 14 |
| Female | 64 | Heavy pound | 2 | 1st–11th rib fractures | 7th posterior rib | Fractures of the right 2nd-8th ribs | Left rib fracture fixation, thoracoscopic exploration and conservative treatment of the right rib first | Adventitial hematoma | 4 |
CT, computed tomography.
Table 2
| Case No. | Sex | Age (years) | Fractured left ribs | Fractured ribs causing TAI | Surgical procedure(s) | Author(s) | Year of publication |
|---|---|---|---|---|---|---|---|
| 1 | Female | 24 | 9–10 | Fracture ends of the 10th left rib | Resection of the 10th left rib + adventitial repair with pleura | Kabiri et al. (11) | 2007 |
| 2 | Male | 57 | 6–10 | Fracture ends of the 6th and 7th left ribs | Fracture end repair + adventitial repair | Yanagawa et al. (12) | 2008 |
| 3 | Male | 87 | 8–9 | Free bone fragments of the 8th left rib | Removal of free bone fragments + direct adventitial repair | Bruno et al. (13) | 2009 |
| 4 | Female | 43 | Unknown | Free bone fragments of the 5th left rib | Resection of free bone fragments + aortic repair | Carter et al. (14) | 2011 |
| 5 | Male | 63 | 5–11 | Fracture ends of the 7th left rib | Resection of fracture ends + adventitial repair | Kitamura et al. (3) | 2012 |
| 6 | Female | 55 | 3–8 | Free bone fragments of the 7th left rib | Death | Kano et al. (15) | 2014 |
| 7 | Female | 34 | 4–8 | Fracture ends of the 4th–6th left ribs | Resection of the 4th–8th left ribs + total aortic repair | Xie et al. (16) | 2019 |
| 8 | Male | 66 | 8–11 | Fracture ends of the 10th left rib | Resection of fracture ends of the 10th left rib + adventitial repair |
TAI, thoracic aortic injury.
Results
There was no perioperative death, and the length of stay in our hospital was 3 to 21 days. In the case of left RFs with spleen rupture, acute renal failure and secondary intra-abdominal infection occurred after overlapping emergency surgery. Conservative treatment was administered accordingly, and the patient was discharged after cure. No perioperative complications were observed in other patients. The pre-discharge chest CT scans showed that the fractured ribs were stabilized after internal fixation (Figure 4). According to the follow-up CT scans at 6 months post-discharge, the fracture ends were in place, without any signs of displacement or abnormalities at the site of the thoracic aorta.
Discussion
BTAI is a clinically rare but fatal condition (17). RFs serve as a chief risk factor for BTAI (18,19). The retrospective study by Choi et al. showed that RFs contributed to approximately 22.9% of all closed TAI cases (20). The diagnosis of this TAI largely depends on the initial CT and clinical manifestations such as a hemorrhagic shock after injury. For acute BTAI, only about 20% of patients can make it to the hospital, and more than 40% die during their hospital stay (21).
In addition to acute injury to the aorta, RFs can result in delayed TAI, which has an insidious onset and escapes the initial imaging tests after injury. The exact mechanism of this injury is not fully understood. It is inferred that there is a small clot covering the perforated aorta, and the unintended removal of the clot leads to massive hemorrhage (22), or RF displacement due to movement penetrates the aorta and results in BTAI (13,14). Another possible explanation relates to nursing procedures (such as turning over the body and tapping the back) or vigorous passive movement during patient transfers. From the cases reported by previously published studies (14,16,22) and our hospital, it is evident that TAI is more likely in patients with ≥4 fractured ribs or multiple fractures in a single rib, of which the broken ends exist in the lateral erector spinae. This may be explained by the loss of local chest wall stability after multiple RFs that entails a risk of displacement. If a rib is broken in multiple places, the bone fragments will become free-floating and prone to penetrate the thoracic cavity. RFs beyond the lateral erector spinae are distant from the aorta and thus can hardly affect the aorta even if displacement occurs. Notably, the present study suggested that fractures of the 10th rib could induce TAI, whilst previous study reached different conclusions (23). Timely diagnosis plays a pivotal role in the treatment of delayed TAI. Therefore, it is recommended that patients receive active surgical intervention if fractures of the 4th–10th left ribs, including the bicortical ones, are present with such important factors.
Although the indications for RF internal fixation have been a controversial and disputed subject (24), it is generally accepted that patients with >3 fractured ribs should receive internal fixation (25). As far as RFs are concerned, the most important treatment principle is to prevent or minimize the risk of complications (26). Considering the potentially fatal consequences, surgical intervention should be undertaken early after diagnosis. Non-RF-induced closed TAI is associated with shearing forces, abrupt deceleration, and acute changes in intravascular pressure. These BTAI cases typically involve the aortic isthmus (6,7). By contrast, RF-induced TAI predominantly affects the aorta adjacent to the broken ends of RFs or surrounded by free bone fragments (15). For TAI caused by post-fracture free bone fragments, some researchers propose treatment plans centered on the removal of free bone fragments (14,27). However, given the lack of plates to stabilize the floating ribs, such plans cannot eliminate the risk of secondary TAI unless adequate resection margins are achieved (28). Notably, excessive resection can result in the loss of mineral elements from the affected ribs. In most cases, the broken ends of fractured posterior ribs contributing to TAI reside in the inside of lateral erector spinae, which can be partially resected or used as a strut to achieve internal fixation if they adjoin the transverse process of the corresponding vertebra (29). In patients with transverse process fractures who have been treated by our hospital and followed up for over a year, the steel plates have not become loose or significantly affected their daily activities even though further follow-ups are needed to assess the long-term outcomes. When a patient needs overlapping emergency surgery for spleen rupture and TAI, under which circumstances saving the patient’s life is always the top priority, the TAI should be repaired first to avoid displacement of the fracture ends due to traction of the left chest wall when handling the intra-abdominal organs to expose an incision. Otherwise, it can lead to fatal aortic rupture and massive hemorrhage. Vital signs require close monitoring throughout the operation, and the time of thoracic operation should be minimized by treating TAI and fixing displaced ribs as quickly as possible. Thoracoscopy is recommended for these procedures to look at the operation field from different angles and ensure the safe removal of free bone fragments.
Limitations
The present study has its limitations. First, it is limited by the modest sample size. Only 7 cases have been reported by our hospital because the condition has a low incidence. The overall sample size remains small even though other reported cases have been included for multi-center retrospective analysis. Second, the absence of a control group makes it impossible to provide statistical evidence for our conclusions and underpins the need for further validation of the study results with more cases.
Conclusions
For patients with bicortical and more severe fractures of the 4th–10th left posterior ribs, active surgical intervention is recommended if they have the following important factors for delayed TAI: there are ≥4 fractured ribs or a single rib fractured in multiple locations; or the fracture ends are in the inside of the lateral erector spinae. Surgical procedures are needed to fix floating ribs, remove free bone fragments, and stabilize the chest wall, while exploratory thoracoscopy can help assess the severity of TAI and develop treatment plans accordingly.
Acknowledgments
Funding: The project was supported by the fund of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital (No. ynhg201919).
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1359/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1359/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1359/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Shanghai Sixth People’s Hospital (No. 2020-KY-034). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Izumi S, Nakai C, Haraguchi T, et al. Retrospective study of thoracic endovascular aortic repair as a first-line treatment for traumatic blunt thoracic aortic injury. Gen Thorac Cardiovasc Surg 2022;70:16-23. [Crossref] [PubMed]
- Eghbalzadeh K, Sabashnikov A, Zeriouh M, et al. Blunt chest trauma: a clinical chameleon. Heart 2018;104:719-24. [Crossref] [PubMed]
- Kitamura R, Colon M, Dave J. Delayed presentation of aortic laceration from seventh rib fracture: an uncommon complication. J Thorac Cardiovasc Surg 2012;144:e121-e123. [Crossref] [PubMed]
- Cassidy S, Allouni K, Day C, et al. Blunt Thoracic Aortic Injury and Acute Trauma: The Effect on Aortic Diameter and the Consequences for Stent-graft Sizing. Ann Vasc Surg 2021;72:563-70. [Crossref] [PubMed]
- Arbabi CN, DuBose J, Charlton-Ouw K, et al. Outcomes and practice patterns of medical management of blunt thoracic aortic injury from the Aortic Trauma Foundation global registry. J Vasc Surg 2022;75:625-31. [Crossref] [PubMed]
- Yoon WJ, Mani K, Wanhainen A, et al. Anatomic feasibility of off-the-shelf thoracic single side-branched endograft in patients with blunt traumatic thoracic aortic injury. J Vasc Surg 2021;74:1456-1463.e2. [Crossref] [PubMed]
- Arbabi CN, DuBose J, Starnes BW, et al. Outcomes of thoracic endovascular aortic repair in patients with concomitant blunt thoracic aortic injury and traumatic brain injury from the Aortic Trauma Foundation global registry. J Vasc Surg 2022;75:930-8. [Crossref] [PubMed]
- Prendes CF, Stana J, Schneidwind KD, et al. Blunt traumatic thoracic aortic injuries: a retrospective cohort analysis of 2 decades of experience. Interact Cardiovasc Thorac Surg 2021;33:293-300. [Crossref] [PubMed]
- Brown SR, Still SA, Eudailey KW, et al. Acute traumatic injury of the aorta: presentation, diagnosis, and treatment. Ann Transl Med 2021;9:1193. [Crossref] [PubMed]
- Bauman ZM, Grams B, Yanala U, et al. Rib fracture displacement worsens over time. Eur J Trauma Emerg Surg 2021;47:1965-70. [Crossref] [PubMed]
- Kabiri el H. Atypical traumatic thoracic aorta after rib fractures. Asian Cardiovasc Thorac Ann 2007;15:180-1. [Crossref] [PubMed]
- Yanagawa Y, Kaneko N, Hagiwara A, et al. Delayed sudden cardiac arrest induced by aortic injury with a posterior fracture of the left rib. Gen Thorac Cardiovasc Surg 2008;56:91-2. [Crossref] [PubMed]
- Bruno VD, Batchelor TJ. Late aortic injury: a rare complication of a posterior rib fracture. Ann Thorac Surg 2009;87:301-3. [Crossref] [PubMed]
- Carter RR, Orr NT, Minion DJ, et al. Aortic injury from posterior rib fracture. Eur J Cardiothorac Surg 2011;39:138. [Crossref] [PubMed]
- Kano M, Chikugo F, Fujimoto E. Delayed aortic injury caused by sharp rib fracture. Asian Cardiovasc Thorac Ann 2014;22:500. [Crossref] [PubMed]
- Xie H, Ning S, Li N, et al. Two uncommon cases of thoracic aortic injury caused by rib fractures. J Thorac Dis 2019;11:S1113-8. [Crossref] [PubMed]
- Fox N, Schwartz D, Salazar JH, et al. Evaluation and management of blunt traumatic aortic injury: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2015;78:136-46. [Crossref] [PubMed]
- Yu L, Baumann BM, Raja AS, et al. Blunt Traumatic Aortic Injury in the Pan-scan Era. Acad Emerg Med 2020;27:291-6. [Crossref] [PubMed]
- Shibahashi K, Matsunaga H, Ishida T, et al. A new screening model for quantitative risk assessment of blunt thoracic aortic injury. Eur J Trauma Emerg Surg 2022; Epub ahead of print. [Crossref] [PubMed]
- Choi MS, Cho YH, Kim WS, et al. Favorable Outcomes of Open Surgical Repair for Blunt Aortic Injury in the Era of Endovascular Repair. Thorac Cardiovasc Surg 2017;65:105-11. [Crossref] [PubMed]
- Boutin L, Caballero MJ, Guarrigue D, et al. Blunt Traumatic Aortic Injury Management, a French TraumaBase Analytic Cohort. Eur J Vasc Endovasc Surg 2022;63:401-9. [Crossref] [PubMed]
- Park HS, Ryu SM, Cho SJ, et al. A treatment case of delayed aortic injury: the patient with posterior rib fracture. Korean J Thorac Cardiovasc Surg 2014;47:406-8. [Crossref] [PubMed]
- Talbot BS, Gange CP Jr, Chaturvedi A, et al. Traumatic Rib Injury: Patterns, Imaging Pitfalls, Complications, and Treatment. Radiographics 2017;37:628-51. Erratum in: Radiographics 2017;37:1004. [Crossref] [PubMed]
- Beks RB, Peek J, de Jong MB, et al. Fixation of flail chest or multiple rib fractures: current evidence and how to proceed. A systematic review and meta-analysis. Eur J Trauma Emerg Surg 2019;45:631-44. [Crossref] [PubMed]
- de Campos JRM, White TW. Chest wall stabilization in trauma patients: why, when, and how? J Thorac Dis 2018;10:S951-62. [Crossref] [PubMed]
- Senekjian L, Nirula R. Rib Fracture Fixation: Indications and Outcomes. Crit Care Clin 2017;33:153-65. [Crossref] [PubMed]
- Ryu DW, Lee MK. Cardiac tamponade associated with delayed ascending aortic perforation after blunt chest trauma: a case report. BMC Surg 2017;17:70. [Crossref] [PubMed]
- El Husseiny M, Karam L, Haddad F, et al. Perforation of the aorta by a rib edge: an unusual complication after chest wall resection. Ann Vasc Surg 2012;26:574.e15-7. [Crossref] [PubMed]
- Zhao W, He W, Yang Y, et al. A case of thoracic aortic injury caused by multiple rib fractures. AME Case Rep 2021;5:8. [Crossref] [PubMed]
(English Language Editor: C. Betlazar-Maseh)


